Translate this page into:
Lymphatic Malformations: Current Status
Address for correspondence: Dr. Niti Khunger, Department of Dermatology and STD, VM Medical College and Safdarjang Hospital, New Delhi - 110 029, India. drniti@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
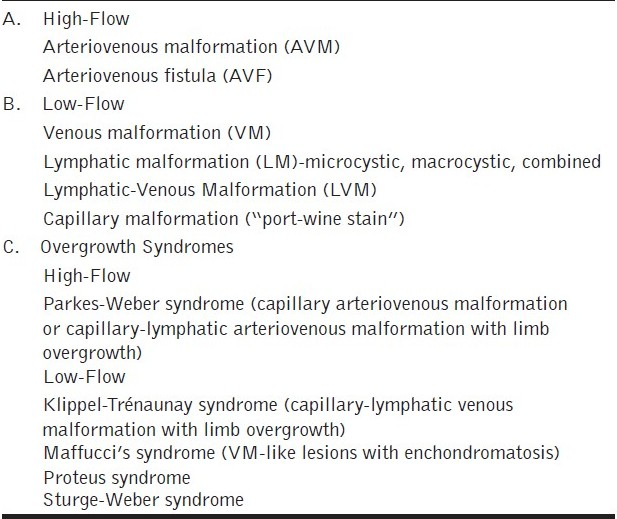
Vascular malformations (VMs) are the most common congenital vascular lesions that arise due to errors in vascular formation during embryonic life. They do not proliferate, but gradually enlarge and do not involute, unlike hemangiomas that proliferate and usually involute. There was a lot of confusion previously regarding the nomenclature of vascular lesions; however, that has been resolved to a great extent by the work of Mulliken and Glowacki.[1] A dramatic change in the understanding of congenital VMs, particularly with regard to classification, anatomy, pathophysiology, embryology, diagnostic and therapeutic modalities has occurred in the last two decades.[2] VMs are now classified based on the type of blood flow as follows: slow-flow (capillary, venous, lymphatic) lesions, high-flow (arterial) lesions and combined slow/fast-flow lesions [Table 1].
The nomenclature of lymphatic malformations (LMs) too has been revised. Based on the size of the lymphatic lumen, LMs (previously termed lymphangiomas) can be divided into microcystic lesions (previously termed lymphangioma circumscriptum), macrocystic lesions (previously termed cystic hygromas) and a combined form. Hence, the term cystic hygroma has now been replaced by the term macrocystic LM. Macrocystic LMs can be associated with several congenital disorders, including Down syndrome and other trisomy disorders, Turner syndrome, hydrops fetalis, Noonan syndrome and several others.
Patients should therefore undergo cytogenetic analysis for chromosomal aneuploidy and parents should receive genetic counselling because aneuploidic conditions can recur in subsequent pregnancies. The most important diagnostic tool in VMs is contrast-enhanced magnetic resonance scanning (MRI), which demonstrates the extent of the lesion and helps to differentiate between hemangiomas, and other venous, lymphatic and arterial lesions. Doppler ultrasound can confirm the flow of the lesion. Prenatal ultrasonography can detect relatively large lesions as early as the second trimester.[3]
Lymphatic VMs never involute, but expand or contract depending on the flow of lymphatic fluid, and the occurrence of inflammation or intralesional bleeding. Indications for treatment depend on the size, location and symptoms of the lesion. Cosmetic disability, presence of recurrent infection, oozing, crusting, ulceration and pain are the most frequent indications for treatment.[4] Rarely they may cause serious functional disability when present in the orbit or larynx. Treatment modalities of LMs include surgical resection and sclerotherapy.
Sclerotherapy is recently attracting attention and the procedure consists of transcutaneously injecting a sclerosant into the vessel, causing inflammation of the vessel wall, followed by fibrosis, with obliteration of the lumen of the vessel. Various sclerosants have been used including alcohol, bleomycin,[56] doxycycline,[7] polidocanol,[8] sodium tetradecyl sulfate[9] and OK32 (picibanil).[10]
Sclerotherapy can be performed by two ways; percutaneous or transcathetral, under fluoroscopic guidance. Foam sclerotherapy is a relatively newer technique that has been used predominantly for venous malformations.[11] Several studies have established the role of sclerotherapy. Bai et al.[5] treated 79 patients of oral and facial LMs; 42 patients with sclerotherapy alone, 14 patients with sclerotherapy followed by secondary surgery and 23 patients with surgery and sclerotherapy. The overall improvement was excellent in 55.7% (44 out of 79) of the patients. Cure rates were superior in the group having surgery with sclerotherapy (73.91%; P<0.05) compared to the group having sclerotherapy alone (42.86%). Similar results were observed by Kim et al.[12] who reported a marked improvement in two third of the studied patients. However, there was one mortality in the bleomycin group.
The advantages of sclerotherapy include relative ease of administration and safety as compared to surgery. It is particularly useful in VMs of the head and neck, which often involve multiple contiguous anatomic spaces and enclose critical neurovascular structures, making surgical treatment difficult and often unsuccessful. Further, though surgical excision is recommended for resectable lesions, there is a high recurrence rate. Raveh et al.[13] reported a recurrence rate of 22% in 74 children treated with primary surgical excision. Surgical intervention at a younger age, especially in neonates and the presence of associated symptoms like infection, dyspnea, dysphagia and hemorrhage was associated with a higher recurrence rate. Surgery should be avoided for large lesions and for lesions localized near vital structures such as the optic nerve, facial nerve, etc. Sclerotherapy can also be combined with other treatments such as surgery, radiofrequency ablation, particularly for microcystic LMs.[14]
Finally, it should be kept in mind that many patients may benefit by observation alone with out any intervention. Dasgupta et al.[15] reported that patients with asymptomatic macrocystic LMs of the head and neck, who underwent interventional procedures had a higher complication and recurrence rate compared to patients who were managed by observation alone. Thus, the decision to treat patients with asymptomatic macrocystic LMs should be undertaken by a multidisciplinary team, after careful consideration.
Sclerotherapy is a relatively safe modality, particularly for the treatment of low-flow VMs. Complications are few and include skin necrosis, small skin ulcers, urticarial reactions, scarring and allergic reactions. It is contraindicated if the patient is allergic to the sclerosant. Caution has to be exercised at sites where post-injection swelling can put another organ at risk, like injury to the optic nerve or airway swelling.
To conclude, sclerotherapy is a minimally invasive technique that is now well accepted as an independent as well as an adjunctive therapy in the treatment of the venous, lymphatic and combined low-flow VMs. Being a conservative and simple procedure, it helps to reduce the cost and morbidity associated with surgery. Its popularity has increased in recent years due to the availability of safer sclerosing agents and due to the evolution of newer techniques such as foam sclerotherapy. All patients should be managed in a multidisciplinary clinical setting, including a vascular surgeon, plastic surgeon, pediatric surgeon, diagnostic radiologist, interventional radiologist, dermatologist, ophthalmologist and orthopedic surgeon for optimum results.
REFERENCES
- Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412-22.
- [Google Scholar]
- A new approach to the congenital vascular malformation with new concept - Seoul Consensus. Int J Angiol. 2003;12:248-51.
- [Google Scholar]
- Current management of hemangiomas and vascular malformations. Clin Plast Surg. 2005;32:99-116.
- [Google Scholar]
- Vascular anomalies in the neonate: Dilemmas in management. J Neonatology. 2008;22:41-8.
- [Google Scholar]
- Sclerotherapy of microcystic lymphatic malformations in oral and facial regions. J Oral Maxillofac Surg. 2009;67:251-6.
- [Google Scholar]
- Bleomycin sclerotherapy in congenital lymphatic and vascular malformations of head and neck. Int J Pediatr Otorhinolaryngol. 2005;69:75-80.
- [Google Scholar]
- Percutaneous sclerotherapy of lymphatic malformations with doxycycline. Lymphat Res Biol. 2008;6:209-16.
- [Google Scholar]
- Sonographically guided percutaneous sclerosis using 1% polidocanol in the treatment of vascular malformations. J Clin Ultrasound. 2002;30:416-23.
- [Google Scholar]
- Definitive percutaneous treatment of lymphatic malformations of the trunk and extremities. J Pediatr Surg. 2008;43:136-9.
- [Google Scholar]
- Sclerotherapy for congenital lesions in the head and neck. Otolaryngol Head Neck Surg. 2004;131:307-16.
- [Google Scholar]
- Prognostic factors in the treatment of lymphatic malformations. Arch Otolaryngol Head Neck Surg. 1997;123:1061-5.
- [Google Scholar]
- Microcystic lymphatic malformation (Lymphangioma circumsciptum) treated with a minimally invasive technique of radiofrequency ablation and sclerotherapy. Dermatol Surg. 2010;36:1711-17.
- [Google Scholar]
- Noninterventional treatment of selected head and neck lymphatic malformations. J Pediatr Surg. 2008;43:869-73.
- [Google Scholar]





