Translate this page into:
Evaluation of Tissue Tightening by the Subdermal Nd: YAG Laser-Assisted Liposuction Versus Liposuction Alone
Address for correspondence: Dr. Alberto Goldman, Av. Augusto Meyer 163 conj. 1203, Porto Alegre RS, Brazil 90550-110. E-mail: alberto@goldman.com.br
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Skin tightening is a desirable outcome for skin flaccidity.
Objective:
We evaluated the applicability, safety, capacity and intensity of skin tightening with the subdermal 1,064 nm Nd: YAG laser application to the upper arms, and compared the results with liposuction.
Materials and Methods:
Patients with lipodystrophy and mild-to-severe skin laxity of the arms were included (n=28). In half of patients, a single treatment with a subcutaneous laser and liposuction was performed, while the other 14 had a regular liposuction. Treatment parameters, adverse effects and photographic documentation were recorded.
Results:
Aesthetic improvement and skin retraction was superior by laser lipolysis. The procedure was well tolerated without significant complications.
Conclusions:
The subdermal laser-assisted liposuction using a 1,064 nm Nd: YAG laser achieves improved skin tightening.
Keywords
Laser lipolysis
liposuction
skin tightening
INTRODUCTION
Laser-assisted liposuction is a relatively new option in the treatment of localised adipose tissue hypertrophy and skin laxity.[1–5] Adiposity of the arms as well as flaccidity in these regions represent a frequent cosmetic concern associated with ageing. These characteristics can be observed in young patients as well. Traditional approaches to treat this condition included liposuction and, in severe cases, brachioplasty with resection of excess tissue. Liposuction is effective in some cases but there has been no evidence that the procedure improves the skin laxity. Additionally, skin retraction with regular liposuction is very limited. Surgical brachioplasty or arm lift leads to variable scarring. These scars, even when well located, present a significant inconvenience to patients and are aesthetically challenging. The main side effects related to arm lift are seroma, hypertrophic scarring, cellulitis, wound dehiscence, subcutaneous abscess, nerve injury and irregularities.[6]
Recently, the internal use of the neodyminium: Yttrium-aluminum-garnet (Nd: YAG) laser for laser lipolysis was approved by the FDA in the US and in some European and South American countries. Many studies have demonstrated the useful aspects of the subdermal laser action not only in the fat but also in surrounding tissues (dermis, vessels, sweat glands and sebaceous glands).[7–11] Among the effects related directly to the use of 1,064 nm Nd: YAG laser are fat cell disruption and stimulation of new collagen formation.[12–15] The consequent skin and tissue tightening represents the most useful aspects of this modality for skin laxity and localized fat of the arms.[16–19]
Direct comparative trials for sculpturing of upper arms have yet not been performed. We aim to present first data comparing liposuction and laser-assisted liposuction for this delicate indication. In this study, lipodystrophy and flaccidity of the arms were treated with either the Nd:YAG laser-assisted lipolysis or microcannular liposuction (suction-assisted liposuction) to compare the efficacy and safety. This pilot study focuses on the skin tightening effect of these techniques.
MATERIALS AND METHODS
Twenty-eight female patients with skin flaccidity and lipodystrophy of the arms (median age 42.3 years, range 35–54 years) took part in this prospective pilot study at Clinica Goldman de Cirurgia Plastica, in Porto Alegre, Brazil and at Maimonides Day Hospital in Porto Alegre, Brazil [Table 1]. All subjects included in the study had smooth-to-moderate skin laxity with loss of the normal contour of the arms. Additionally, the localized fat on the arms compromised the aesthetics of this anatomical region. Patients with previous surgical treatment such as axillary lymphadenectomy, brachioplasty or liposuction were excluded from the study. Lactating and pregnant women, smokers and obese patients were also excluded. Subjects with infection in the area to be treated or with a weight variation of more than 5% in the follow-up evaluation were not included in the study. All patients underwent a pre-operative assessment including laboratory tests to determine their general medical condition and signed informed consent.

Standardized photodocumentation and measurements of arm circumferences was done immediately before the procedure in order to determine the circumference of each arm as well as to verify the asymmetries. The photographs have been analyzed independently.
Since circumferential measurements may be difficult to standardize, particular attention was paid to the exact positioning during measurement. Arms were measured in standing position hand down. The measures were taken based on an imaginary point demarcated in the posterior aspect of the arm, distally 10 cm from the posterior axillary fold. This represented the reference point for the measurement of the circumference of each arm and standardized the data collection [Figure 1]. These standardized measurements were repeated in the follow-up period of 3 months. The analysis of variance was performed on the arm circumference percentage of reduction using the Statistical Package for the Social Sciences for Windows®.

- The assessment of circumference of each arm was based on an imaginary point demarcated in the posterior face of the arm, 10 cm from the posterior axillary fold in a distal direction
Surgical technique
All surgeries were performed on an ambulatory basis under aseptic conditions. No prophylactic antimicrobial was used except in one patient with a previous history on endocarditis.
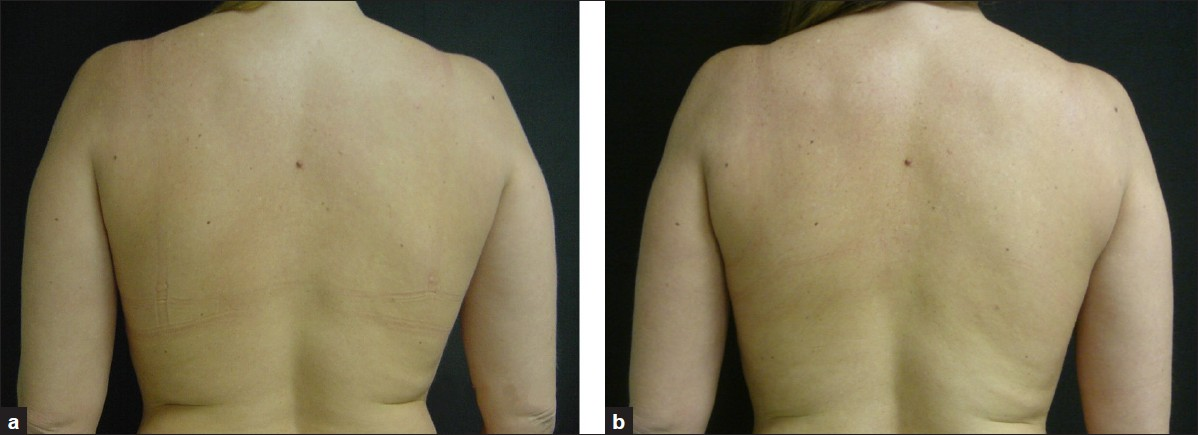
After adequate measurement and evaluation of the localized adiposity, skin texture and laxity of the arms, with the patient in an upright position, the area was marked. Preoperative sedation with midazolam was used for anxious patients. In all cases, an anesthesiologist was present in the operating room. The procedure was initiated 20 minutes after the local subcutaneous tumescent infiltration of Klein's solution using lidocaine 0.05%–0.1%, epinephrine 1:1000 and 10 milliequivalents per liter sodium bicarbonate added to each liter of warm normal saline. The total volume injected per treated arm ranged from 175 to 850 cc. The injection was delivered using infusion pump or syringes. A 20-minute delay allowed an adequate diffusion of the solution as well as appropriate vasoconstriction. One 1 to 2 mm incision was made in the internal aspect of each arm, near the elbow. Up until this step, the procedure was the same for both groups.
Patients intended to treat were allotted to one of the two treatment procedures only based upon their appearance at the departments with every second patients included in group 1. The treatment groups 1 and 2 were only different by the addition of a subdermal laser to microcannular liposuction. In group 1, a pulsed 1,064 nm Nd: YAG system (Smartlipo, Deka, Calenzano (FI), Italy) was combined with liposuction. The energy was delivered to the subcutaneous tissue through a 300–600-micron optical fiber with a 1–1.4 mm diameter stainless steel microcannula of variable length connected to the tip of the fiber. The distal portion of the fiber optic was extended 2 mm beyond the distal end of the cannula. Protective goggles were used by patients as well as the staff. The cannula, containing the optical fiber, was inserted through a small skin incision. In order to visualize the subcutaneous laser action in the fat and subdermal tissues, a helium: Neon (He: Ne) red beam is added to the YAG laser. This provides a reddish transillumination effect acting as a constant and exact locator of the activated laser energy at all times. The more intense the light, the more superficial is the laser action. The cannula is moved in the fat at various depths, including the very superficial subdermal layer at approximately 2 to 3 cm/s. The total energy delivered was individualized according to the amount of fat present, the necessity of dermal stimulation and the consequent tightening effect. The total accumulated energy per side ranged from 5.040 J to 16.560 J. The endpoint of the laser action is achieved when the resistance of the cannula in the fat is overcome showing an effective laser lipolysis. The tissue consistency should also be evaluated by the pinch test. The skin temperature was also controlled during the laser activity on the arms using an external digital thermometer. When the external skin temperature reached 42°C, the laser energy delivered was interrupted thus avoiding a possible tissue burn. As a consequence of the laser action producing cellular lysis, the fat tissue consistency is transformed into a less dense solution. This oily lysate containing fragments of cells, oil and also the infiltrated solution is removed from the arms. Suction using a two holes 2.5 mm cannula under negative pressure was used. The amount of aspirated tissue per patient ranged from 170 to 1180 cc [Table 2].
In group 2, no optical fiber was used but tunnelization with 1–1.4 mm cannulas was exactly the same as in group 1. Immediately after this step, liposuction by the 2.5 mm cannula and negative pressure, similar to the first group, was conducted. Sutures were not used in both groups, allowing a natural and spontaneous drainage following the procedure. A smooth garment was used in all patients for 10 days. Physiotherapy in the form of external lymphatic drainage and ultra sound were begun on the first post-operative day for all patients in group 1 and 2 for 2 weeks with the same frequency of application.
The patients were evaluated and photographed at three months after the procedure. The circumference of each arm was re-measured using same preoperative reference points. The results are given as mean ± standard deviation. The follow-up period ranged from 3 to 20 months.
RESULTS
Both treatment groups were comparable in the means of pre-treatment measurements. There was slightly higher mean age in group 2 (±1.4 years). The range and mean of removed tissue was comparable, what points to the fact that difference in outcome are not related to the amount of tissue removed but rather to the tissue response following the procedure.
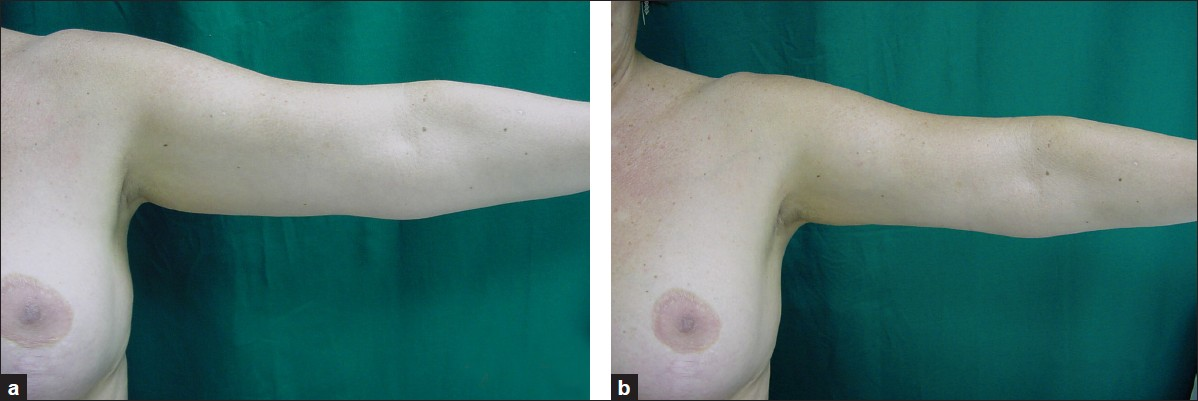
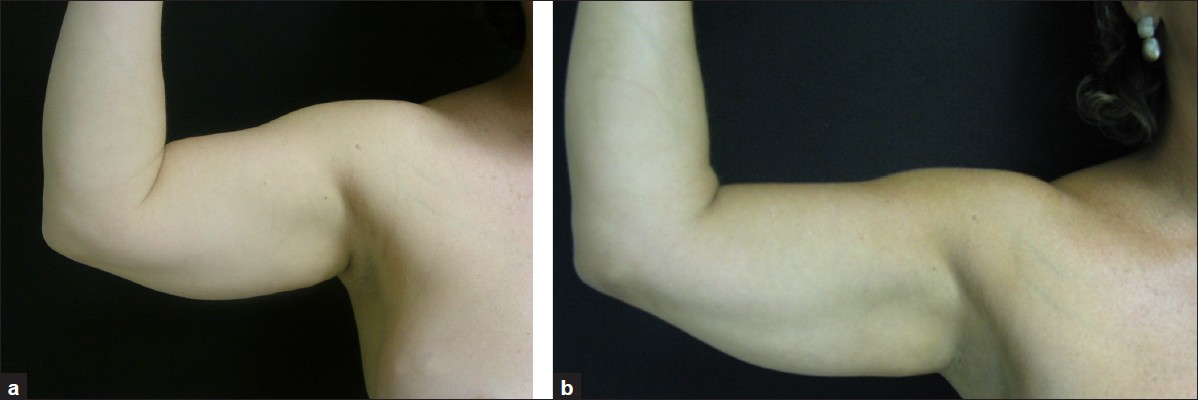
The major outcome in both groups was a reduction in the circumference of the arms with a consequent aesthetic improvement [Figures 2–7].
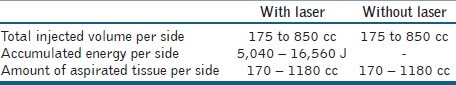
- A 54-year-old patient is shown before (a) and 3 weeks after (b) laser-assisted liposuction of the arms
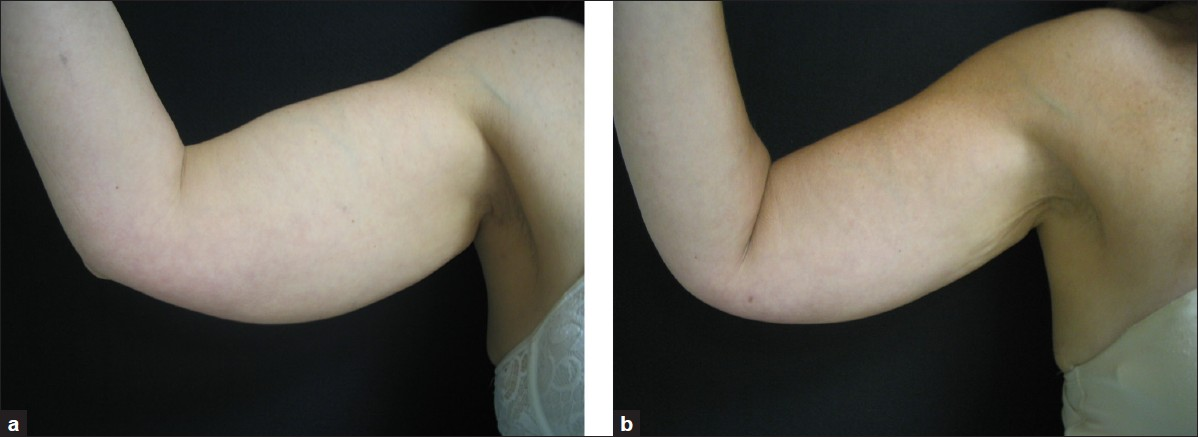
- Lipodystrophy of the arms, posterior view before (a) and 6 months after (b) subdermal laser treatment
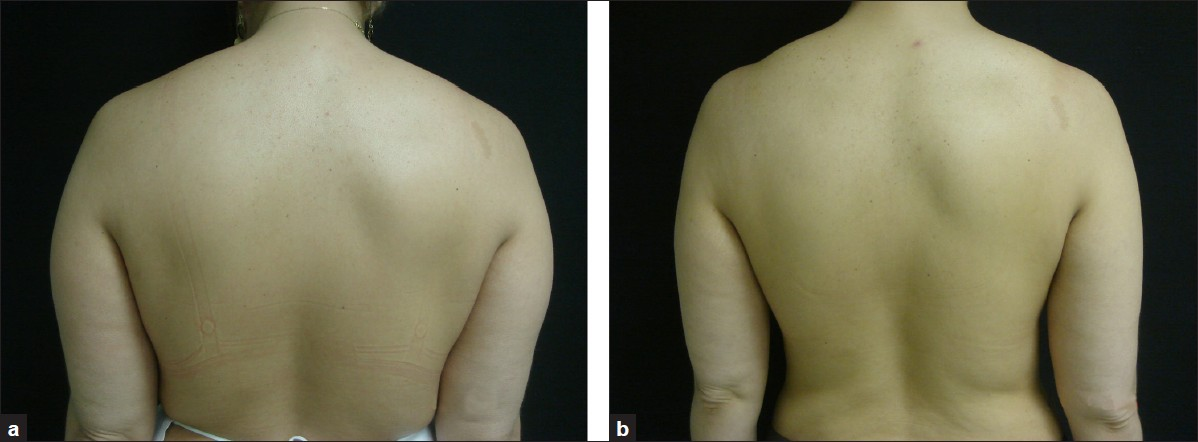
- A 46-year-old woman is shown before (a) and 6 months after (b) laser-assisted liposuction of bilateral the arms
- Patient with localised fat and skin flaccidity is shown before (a) and 3 weeks after (b) laser-assisted liposuction of the arms
- A 49-year-old woman is shown before (a) and 1 year after (b) laser-assisted liposuction of the arms
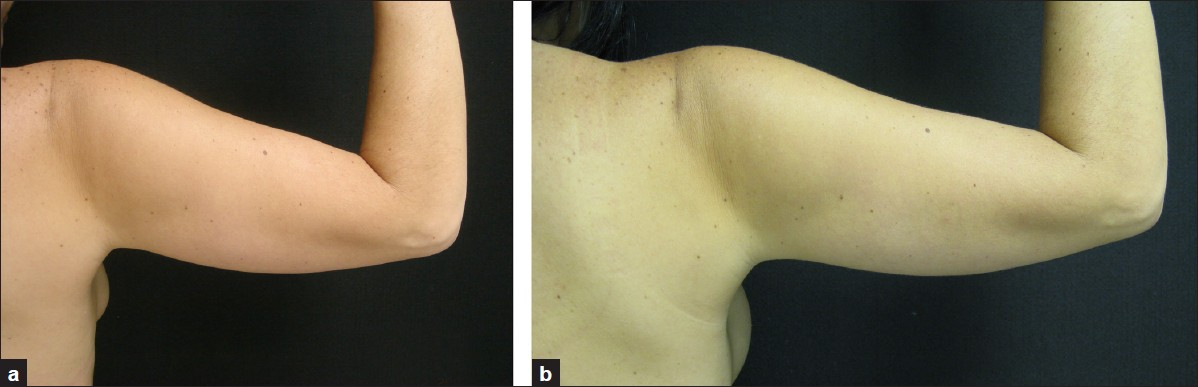
- A 36-year-old woman is shown before (a) and 6 months after (b) laser-assisted liposuction of the arms
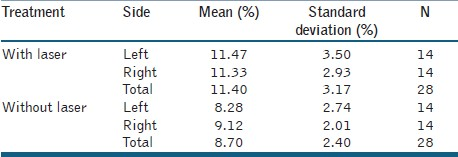
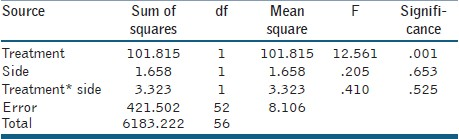
Percentage of reduction in the arm circumference of both groups was tabulated and compared. Both the subdermal 1,064nm Nd: YAG laser-assisted liposuction group and liposuction only group, presented skin and tissue tightening as well as a decrease in the circumference of the arms [Table 3]. Arms treated with laser presented a mean skin retraction of 11.4 ± 3.17%, whereas the group treated without laser had a mean of 8.70 ± 2.40%. Circumference reduction of the laser lipolysis group was significantly higher than the group without laser (P = 0.001) [Table 4]. That is substantiated by pinch testing before and at the end of follow-up and by photodocumentation.
The photographs have been analysed independently. The aesthetic outcome was rated higher with laser lipolysis.
Adverse effects
Ecchymosis, edema and a temporary decline in the sensitivity in the treated areas were observed in some patients in both groups and lasted about 1 to 5 weeks. No other adverse effects or complications such as burns, unaesthetic scarring or irregularities were observed.
DISCUSSION
Various lasers and lights have been used in the past for the improvement of skin quality and texture. They act by stimulating new collagen formation leading to skin retraction in the body and face. All these devices are applied externally and the energy (laser, light, high frequency and ultrasound) must cross the epidermal and dermal barriers to reach their targets in the connective tissue.[1516] Recently, a new laser source applied internally, in the subcutaneous tissue, has been described for the treatment of localized fat using the 1,064 nm Nd: YAG laser.[1820–21] Despite the fact that the initial indication for the use of this laser was lipolysis, the capacity to produce subcutaneous tissue retraction and mainly skin tightening represents a relevant and important aspect widening the indication of liposuction to many other situations. Patients who probably were candidates for skin resections with consequent scars would now benefit from the use of this approach.[17–19]
The major effects of the laser action in the fat and surrounding tissues are photomechanical and photothermal. The preferred parameters include low laser power, continuous wave irradiation, and relatively long irradiation times (>2 min) with bare fibers. This approach reduces the operation risk and stress for the patient reduces. Hereby interstitial tissue coagulation can be achieved for volumes with diameters of up to 5 cm. Of particular interest is the fact that expansion of adipose tissue is linked to the development of its vasculature. Indeed, adipogenesis is tightly associated with angiogenesis, as shown by the findings that adipose tissue explants trigger blood vessel formation, whereas in turn adipose tissue endothelial cells promote preadipocyte differentiation. Modulation of angiogenesis as laser coagulation of vessels may have the potential to impair adipose tissue development and thus provide a novel therapeutic approach for prevention of recurrence of adipocyte growth.[22]
Significant histological findings following laser lipolysis have already been described in the literature.[141523] The energy delivered to subcutaneous tissue leads not only to fat cell disruption (laser lipolysis) but also to the stimulation and remodeling of new collagen with a consequent skin tightening effect.[31424] This observation can be easily explained by mathematical modelling showing that the temperature increase inside the lower dermis is sufficient (48–50°C) to induce skin tightening. Nd: YAG induced hyperthermia allows heating of a precisely defined volume of tissue. The resulting wound repair is associated with new formation of both collagen and elastin.[24]
Formation of small channels, coagulation of collagen and reorganisation of reticular dermis result in increased skin elasticity and reduced flaccidity.[13151825]
Quantification of this effect is a major tool to optimize the procedure. We performed an evaluation of upper arm perimeter and found a significant benefit of laser-assisted liposuction compared to microcannular liposuction. In a small laser lipolysis study involving five male patients with focal abdominal fat deposits skin shrinkage was measured from four quadrants of tattoo skin markings and evaluated using a three-dimensional camera. Skin tightening was measured with a skin elasticity device. In this study, it could be demonstrated that elasticity increased by 26%; the average skin shrinkage was 17%.[26]
Some points remain challenging in our study: What is the extent of skin flaccidity that can be improved by this technique and how much retraction of the skin would be possible to achieve in each situation? Are these results reproducible? The results of this pilot study open potential indications of the use of the laser as an effective tool for skin and tissue retraction in other areas of the body and face. Subdermal Nd: YAG laser could be used as an isolated procedure or in association with traditional surgical and non surgical techniques. The treatment of wrinkles would be another possible indication of this entity due to its collagen and elastin stimulation with consequent skin retraction and improvement of skin texture. Further studies to evaluate the amount of energy needed to produce an effective action without damaging the tissues, the clinical effect of association with other wavelengths of Nd: YAG laser, determining the endpoint to the laser action, the quantification of the retraction and long term results are required in the future.
Based on the subjective evaluation comparing the photographic documentation and the objective mathematical evaluation of the arm circumference, it was evident that skin tightening produced by the subdermal use of the Nd: YAG laser represents a useful and versatile tool in the management of the skin flaccidity and lipodystrophy.
The positive aspects of this modality include lack of overtly evident scars, minimal discomfort in the recovery period, high patient satisfaction, educed complication rate and a relatively simple technique. Added to this is the significantly improved outcome in the appearance of the arms.
The procedure proved to be effective for skin tightening and lipodystrophy of the arms and represents another useful option to treat these conditions in this anatomic area. Further studies are required in order to determine the reproducibility of these effects in other anatomical regions.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Laser lipolysis: Liposuction using Nd: YAG laser. Rev Soc Brasil Cirurgia Plástica. 2002;17:17-26.
- [Google Scholar]
- Liposuction using neodymium: Yttrium-aluminium-garnet laser. Plast Reconstr Surg. 2003;111:2497.
- [Google Scholar]
- Fat liquefaction: Effect of low-level laser energy on adipose tissue. Plast Reconstr Surg. 2002;110:912.
- [Google Scholar]
- Submentale laserassistierte Liposuktion: Klinische Erfahrungen und histologische Ergebnisse. Kosmet Med. 2005;26:4-11.
- [Google Scholar]
- Long-term outcomes and complications associated with brachioplasty: A retrospective review and cadaveric study. Plast Reconstr Surg. 2006;117:2219-23.
- [Google Scholar]
- Lipoaspiração a Laser. In: Toledo LS, ed. Laserlipólise em Lipoplastia. Brazil: DiLivros Rio de Janeiro; 2006. p. :111-21.
- [Google Scholar]
- Noninvasive treatment of bromidrosis by frequency doubled Q-switched Nd: YAG laser. Aesthetic Plast Surg. 2000;24:198-201.
- [Google Scholar]
- Laser-assisted suction of axillary sweat glands and axillary epilation. In: Shiffman MA, Di Giuseppe A, eds. Liposuction - Principles and Practice. Berlin, Heidelberg: Springer-Verlag; 2006. p. :505-15.
- [Google Scholar]
- Effect of low-level laser therapy on abdominal adipocytes before lipoplasty procedures. Plast Reconstr Surg. 2004;113:1796.
- [Google Scholar]
- Histologic evaluation of the pulsed Nd: YAG laser for laser lipolysis. Laser Surg Med. 2005;36:43-6.
- [Google Scholar]
- Comparison of histologic, biochemical and mechanical properties of murine skin treated with the 1064 nm and 1320 nm Nd: YAG lasers. Exp Dermatol. 2005;14:876-82.
- [Google Scholar]
- Laser induced collagen remodeling: A comparative study in vivo on mouse model. Lasers Surg Med. 2008;40:13-9.
- [Google Scholar]
- Laser lipolysis with sequential emsission of 1064 nm and 1320 nm wavelengths. Cynosure Whitepaper. Available at: http://ebookbrowse.com/dibernardo-lipolysis-white-paper-pdf-d48622404
- [Google Scholar]
- Laser lipolysis. In: Alam M, Doner JS, eds. Procedures in Cosmetic Dermatology - Non-surgical Skin Tightening and Lifting. Netherlands: Saunders – Elsevier; 2008. p. :157-64.
- [Google Scholar]
- Smartlipo MultiPlex–an advanced system for laser lipolysis. In: Cynosure Whitepaper. 2008.
- [Google Scholar]
- Laser lipolysis. In: DiBernardo Barry E, Pozner Jason N, eds. Lasers and Non-Surgical Rejuvenation. Netherlands: Saunders- Elsevier; 2009. p. :115-27.
- [Google Scholar]
- Cellulite: A new treatment approach combining subdermal Nd: YAG laser lipolysis and autologous fat transplantation. Aesthetic Surg J. 2008;28:656-62.
- [Google Scholar]
- Evaluation of skin tightening after laser-assisted liposuction. Aesthet Surg J. 2009;29:400-7.
- [Google Scholar]






