Translate this page into:
Laser Hair Removal as Adjunct to Surgery for Pilonidal Sinus: Our Initial Experience
Address for correspondence: Dr. Wagih Mommtaz Ghnnam, 14 Gawad Hosney Street, Sherbin, Dakahlia, Egypt. E-mail: wghnnam@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Chronic pilonidal disease is a common debilitating condition. It is a cause of considerable morbidity and social embarrassment. This prospective randomized study compared permanent laser hair removal following the excision of pilonidal disease with conventional methods for hair removal.
Materials and Methods:
Patients undergoing surgery for pilonidal disease were randomized to two groups: those using laser hair removal methods following completed healing of wounds (group I) or regular post-healing conventional methods for hair removal, mainly razor and depilatory creams, for at least 6 months (group II). Group I patients received regular, monthly laser hair treatment sessions using Alexandrite laser for four sessions.
Results:
Group I patients had a mean age of 23.6 ± 4.7 years. Group I patients had monthly laser hair removal session and then they were regularly followed up within the proposed schedule. They found the procedure comfortable with no complications. Group II patients had a mean age of 23.7 ± 6.6 years; they reported difficulty in maintaining hair removal with these conventional methods, and mostly, by the end of the first year, all cases stopped maintaining regular hair removal. Recurrence occurred in Group II patients (two cases) mostly due to failure in maintaining hair removal and area hygiene.
Conclusions:
We advocate the use of laser epilation after surgery for pilonidal sinus as it decreases the chance of recurrence but larger studies with long-term follow-up are still needed to approve this conclusion.
Keywords
Excision
laser hair removal
pilonidal sinus
INTRODUCTION
Pilonidal disease is a common condition, ranging from the routine cyst with abscess to extensive chronic infection and sinus formation. Pilonidal disease or sinus arises in the hair follicles in the gluteal or natal cleft. The estimated incidence is 26 per 100,000 people, affecting men twice as often as women.[1] These chronic discharging wounds cause pain and impact upon quality of life. The management of chronic pilonidal disease is variable, contentious and problematic. Principles of treatment require the eradication of the sinus tract, complete healing of the overlying skin and prevention of recurrence.
The optimal treatment strategy is still a matter of discussion. Many different approaches have been put forward, ranging from a conservative treatment to an extensive surgical excision. These procedures result in healing in 58% of cases within 10 weeks, but recurrence is common, varying from 11% to 14% depending on which treatment has been used.[2]
Lasers have been available for hair removal since 1996. This is by no means a permanent method of hair reduction. Numerous studies have been carried out, and patients often report a 60–80% reduction in hair growth at 6 months.Multiple treatments are often needed and some believe only anagen hair respond.[3–5] Multiple treatments seem to increase progressively the hair-free period between treatments, and also decrease the percentage of hair re-growth.[6] There are no scars, but temporary changes in pigmentation can occur in patients with dark skin types. Complications are few, but a significant number of patients experienced discomfort with the procedures. Most required topical anaesthesia. Hair destruction by laser is achieved by selective absorption of light energy by the melanin in dark hair. Short pulses of light treat a variable number of hair follicles within a target footprint. This is a safe and straightforward procedure with the appropriate training.[78]
Excessive hair growth in the natal cleft is thought to be a key factor in initiating these abscesses and their recurrence. Hair are often found trapped in the base of pilonidal wounds. Recurrence is common and many cases are difficult to heal. Weekly shaving is often advised as a compliment to surgical treatments. However, the natal cleft is difficult to access with a conventional razor. Patients often find that recurrence is delayed if the hair-free interval is prolonged. Blade shaving is the most traditional form of shaving, but also is the hardest. The natal cleft is not as easy to shave with a standard razor as the bikini area is. The natal cleft can be shaved easily if someone else does it for a person, since the usual results of self-shaving are nicks, cuts and horrible rashes afterwards.[9]
Long-term hair removal is open to debate. Most surgeons recommend shaving during healing and for a few months afterwards. A study concluded in 2009 that long-term hair removal was associated with an increased chance of recurrence.[9]
The aim of our study was to prospectively evaluate the efficacy of long-term laser hair removal as an adjunct to surgical treatment of pilonidal sinus and assess its feasibility.
MATERIALS AND METHODS
This is a prospective randomized study of all patients admitted to our hospital undergoing operative treatment of chronic pilonidal sinus disease from November 2007 to February 2011. Patients who presented with acute pilonidal abscesses were excluded from this study. An informed consent was obtained from all the patients. The study was approved by the local ethics committee and was carried out according to the declaration of Helsinki.
This study included 86 patients for whom surgical excision was done and wounds were left open for healing by secondary intention. They were divided randomly into two groups: Group I included 45 patients for whom post-healing (laser treatments were performed after healing from the surgery was completed) laser hair removal was done using Alexandrite laser (GenteLase™) for four sessions at monthly intervals . The Alexandrite laser has a wavelength of 755 nm, and was used at a fluence of 14–16 J/cm2 and fixed pulse duration of 3 ms, with spot size of 15 mm. The light (pulses) was delivered at 1 pulse/s, allowing large areas to be treated rapidly (we call it frequency). Post-treatment care consisted of (Fusicort cream TM, fusidic acid 2%, betamethasone valerate 0.1%, cream applied to the treated skin twice a day for 5 days).
Group II included 41 patients who used post-healing conventional methods for hair removal (razor shaving and cream depilation). All patients were followed up for a mean period of 2 years (range 1–3 years) at least post-healing (study ended by 2011).
Patients were given instructions regarding anal hygiene and hair removal from the area. Subsequently, patients were reviewed about 1 month after surgery in the outpatient department, every 3 months for about 1 year and then every 6 months yearly. The data of those patients were analyzed with special reference to hospital stay, complications, time of healing and recurrence rate. Recurrence was defined as the presence of any persistent purulent/blood-stained discharge from the previously operated or nearby area during the follow-up period.
Statistical analysis was carried out using SPSS, version 17 (SPSS, Chicago, IL, USA); data were expressed as means ± standard deviations for continuous data or as a percentage of the total for categorical variables. A t-test was used for analysis of continuous data and a chi-square test for categorical variables. A P-value of <0.05 was considered statistically significant.
RESULTS
The age of the patients ranged between 16 and 42 years, with a mean age of 23.3 ± 5.8 years.
A total of 75 of the 86 cases were males (87.2%) and 11 were females (12.8%). Most (82.6%) of the patients had primary pilonidal disease, whereas 15 patients (17.4%) had recurrent pilonidal disease [Table 1].

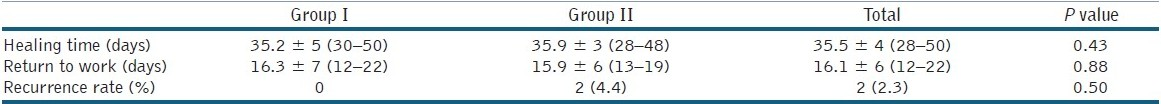
The mean number of laser treatments was four sessions. The overall recurrence rate was 2.3%, after a mean follow-up period of 2 ± 1 year. Group I patients had a mean age of 23.6 ± 4.7 years; 82.2% were males and recurrent cases were 17.7%. Group I patients had a monthly laser hair removal session; then they were regularly followed up within the proposed schedule. They found the procedure comfortable with no complications and only slight discomfort during the laser hair removal session, with no other complications [Table 1]. Group II patients had a mean age of 23.7 ± 6.6 years; 82.9% were males and there were 17.1% recurrent cases. A total of 23 patients used razor for post-healing hair removal while 18 patients use depilatory creams. They reported difficulty in maintaining hair removal with these conventional methods and mostly by the end of the first year, all cases had stopped maintaining regular hair removal and area hygiene; that is why, there was recurrence in two cases in this group [Figure 1]. Although it was found that there was no recurrence in group I while it was found for two cases in group II, this difference was statistically insignificant [Table 2].
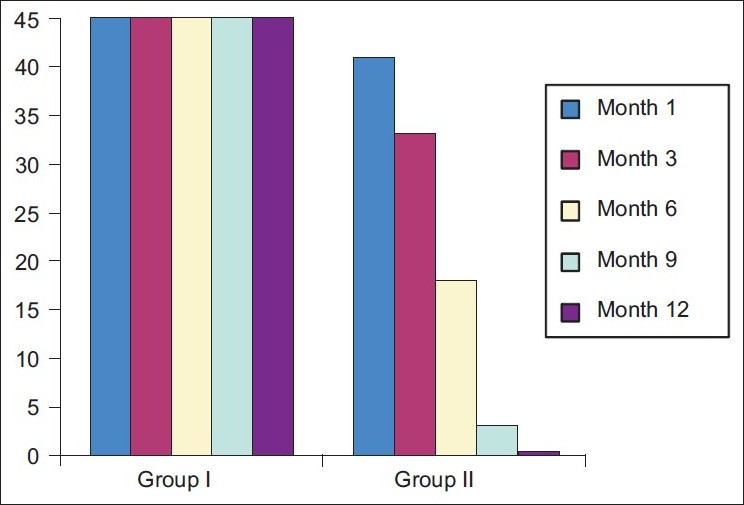
- Group I patients continue to have hair-free time while group II patients refrained from using conventional depilation methods (razor and creams)
DISCUSSION
Pilonidal disease can range from small asymptomatic pilonidal cysts or sinuses to complex chronic disease with multiple sinus tracts, often with chronic inflammation and drainage. The goal of the treatment of pilonidal disease includes excising and healing with a low rate of recurrence and minimizing patient inconvenience and morbidity after the surgical procedure. Men are affected twice as frequently.[10] The origin of pilonidal sinus has been a subject of interest for many years. In the 1950s, it was thought to be of congenital origin, involving the remnant of the medullary canal and the infolding of the surface epithelium or a faulty coalescence of the cutaneous covering in the early embryonic stage,[1112] but most authors now believe that the majority of pilonidal disease cases are acquired and the result of a foreign body response to entrapped hair.[13] After the onset of puberty, sex hormones affect the pilosebaceous glands, and the hair follicles become distended with keratin. As a result, a folliculitis is created, which produces edema and follicular occlusion. The infected follicle extends and ruptures into the subcutaneous tissue, forming a pilonidal abscess. This results in a sinus tract that leads to a deep subcutaneous cavity. The laterally communicating sinus overlying the sacrum is created as the pilonidal abscess spontaneously drains into the skin surface.[10] Loose hair are sucked into the pilonidal sinus by friction and movement of the buttocks whenever the patient stands and sits. This trapped hair stimulates a foreign body reaction and infection.[1011] Excess hair in and around the gluteal cleft increase the risk of the occurrence of the disease, and the frequency and severity of recurrences are directly related to the density of the hair present on the buttocks.[13] Long-lasting or permanent hair removal in the gluteal area in pilonidal sinus disease would eliminate the hair and decrease the risk of recurrent disease.[1415]
The recurrence rate of pilonidal sinus varies depending on the treatment method and the follow-up period of the study.[10–1416–18] In our study, the overall recurrence rate was very low compared to the literature, this is mostly attributed to the long-term laser hair removal in more than half of the cases with no recurrence in such group.
The recent literature coincides with our results on the benefits of laser epilation in pilonidal sinus disease. Benedetto and Lewis[13] reported two patients with recurrent pilonidal sinus disease treated with an 800-nm diode laser, resulting in a long-term relief. Similarly, Lavelle et al.[19] presented a case of pilonidal sinus disease. They treated the surgical scar site five times with ruby laser for epilation and did not observe recurrence in 6 months. Conroy et al.[20] reviewed 14 patients who underwent laser hair removal after pilonidal sinus surgery. The mean number of treatments was 3.9, and none of the patients had developed recurrent disease at 1-year follow-up. They suggested that laser hair depilation and the personal hygiene of the patient were useful in preventing recurrent pilonidal sinus disease. Schulze and colleagues[21] reported that 19 of 23 patients who had laser epilation after surgical interventions and remained in follow-up did not have recurrence or need further surgery. The inadequate follow-up period and small number of patients in these studies make it difficult to derive firm conclusions, but our results and the literature support the beneficial effect of laser epilation as an adjunct to surgery. From our results, we advise four sessions of laser hair removal to obtain the best results.
In our study, recurrences were detected on follow-up visits upon direct patient examination although we believe that the low recurrence rate in our study (2.3%) is probably due to the laser epilation treatments after surgery. In addition, we agree with the necessity of longer follow-ups of the patients, because 75% of the recurrences were detected a minimum of 5 years after the laser treatment.[17]
The main goals of the management of pilonidal sinus disease should be determining the ideal medical or surgical treatment, which includes minimal inconvenience to the patient, a short period of hospitalization, and most importantly, a low risk of recurrence. In this study, the recurrence rates for surgical intervention were found to be comparable with the results of previous studies, but our results strongly suggest that laser hair removal after surgical interventions in pilonidal sinus disease decreases the risk of recurrence in the long term. Laser epilation is simple and quick, without any complications. We recommend laser epilation to every patient with pilonidal sinus disease as an adjunct treatment after the surgical intervention to prevent further surgery.
ACKNOWLEDGMENT
We thank all our patients for their contribution and assistance.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust NZ J Surg. 1992;62:385-9.
- [Google Scholar]
- Does technique alters quality of life after pilonidal sinus surgery? Am J Surg. 2005;190:388-92.
- [Google Scholar]
- Long-term effects of postoperative razor epilation in pilonidal sinus disease. Dis Colon Rectum. 2009;52:131-4.
- [Google Scholar]
- The effect of ruby laser light on ex vivo hair follicles: clinical implications. Ann Plast Surg. 1999;42:249-54.
- [Google Scholar]
- A comparison of the long-pulse and short-pulse Alexandrite laser hair removal systems. Ann Plast Surg. 1999;42:381-4.
- [Google Scholar]
- A clinical study of hair removal using the long-pulsed ruby laser. Dermatol Surg. 1998;24:837-42.
- [Google Scholar]
- Long-term effects of postoperative razor epilation in pilonidal sinus. Dis Colon Rectum. 2009;52:131-4.
- [Google Scholar]
- Healing by primary closure versus open healing after surgery for pilonidal sinus: Systematic review and meta-analysis. BMJ. 2008;336:868-71.
- [Google Scholar]
- Pilonidal sinus disease treated by depilation using an 800 nm diode laser and review of the literature. Dermatol Surg. 2005;31:587-91.
- [Google Scholar]
- Laser hair removal for recurrent pilonidal sinus disease. J Cosmet Laser Ther. 2002;4:91.
- [Google Scholar]
- Successful treatment of recurrent pilonidal sinus with laser epilation. Dermatol Surg. 2005;31:726-8.
- [Google Scholar]
- Timeline of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum. 2007;50:1928-34.
- [Google Scholar]
- The natural history of the post anal (pilonidal) sinus. Ann Royal Coll Surg Engl. 1984;66:201-3.
- [Google Scholar]
- Recurrent pilonidal sinus treated with epilation using a ruby laser. J Cosmet Laser Ther. 2002;4:45-7.
- [Google Scholar]
- Laser depilation and hygiene: Preventing recurrent pilonidal sinus disease. J Plast Reconstr Aesthet Surg. 2008;61:1069-72.
- [Google Scholar]






