Translate this page into:
Surgical Approach for Nevoid Hyperkeratosis of the Areola
Address for correspondence: Mr. Andreas Foustanos, 32 Kifisias Avenue, Megaro Atrina, Paradeisos Amarousiou, Athens - 151 25, Greece. E-mail: diabahmad1@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nevoid hyperkeratosis of the breast is a rare condition affecting the nipple, the areola or both. It appears in both sexes and it can by lateral or unilateral. It can also accompany other skin diseases or systemic conditions including malignancies. Treatment may not be easy due to aesthetic consequences but surgery seems to be the most preferable therapeutic option. We report such a case successfully managed by surgical intervention.
Keywords
Nevoid hyperkeratosis
nipple and areola
surgical approach
INTRODUCTION
Nevoid hyperkeratosis of the nipple and the areola (NHNA) of the breast is a rare condition which is characterized by verrucose thickening and “café au lait” pigmentation of the nipple and areola. First described in the medical literature by Tauber in 1923 as a benign dermatologic change in the nipple and areola, it may involve the nipple, the areola or both.
Athough, in most cases, NHNA is a benign condition, and the location and the potential recurrence may have serious consequences on the breast, of both functional and aesthetic nature.
Nevoid hyperkeratosis can be managed surgically or by conservative modalities; however, it can either threaten the breast function or it can lead to a bad aesthetic result due to mismanagement.
CASE REPORT
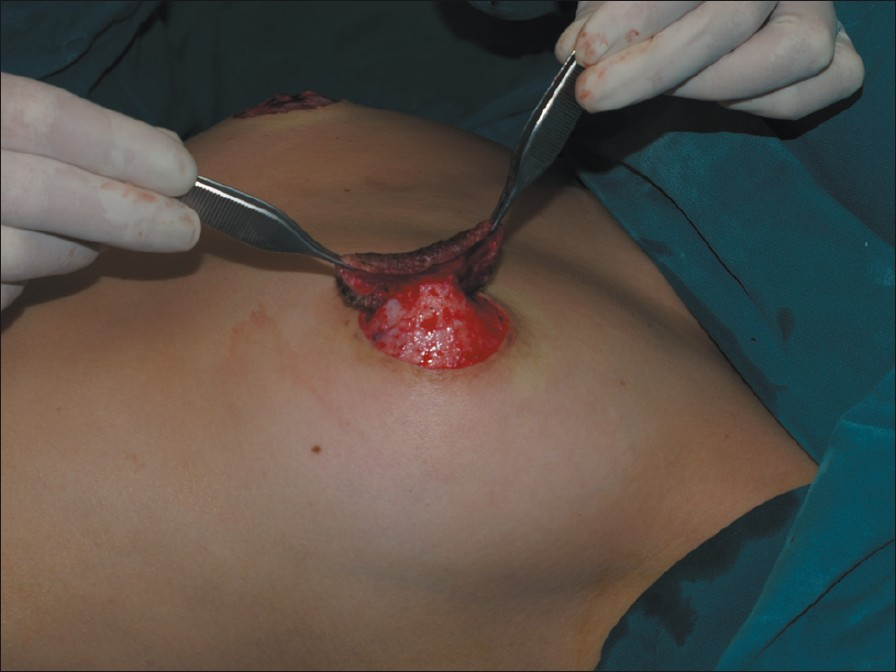
A 19-year-old Greek girl presented to our plastic surgery unit with a bilateral nevoid hyperkeratosis [Figure 1]. She complained that the lesions appeared 7 years ago in both breasts, without any other symptoms apart from the local changes. There was not any remarkable past medical history; her family medical history was also unremarkable. Therefore, she visited our department asking for a surgical treatment. No medical or surgical interventions were tried before.

- The nevoid hyperkeratosis of the areola before the surgery
On examination, there was no sign or history for any endocrine disease; menarche occurred at 13 year. There was no clinical evidence for a dermatosis or a lymphoma. She was not under any regular medication. Her blood examination test was unremarkable; urinalysis and serum biochemistry was normal. A pregnancy test was negative. On immunoelectrophoresis, no paraprotein was detected in serum or in urine. Serology for hepatitis viruses (A, B, C), human immunodeficiency virus and venereal disease research laboratory test (VDRL) was negative. Imaging studies revealed no hepato-splenomegaly, enlarged lymph nodes or abdominal or mediastinal masses.
A punch biopsy revealed hyperkeratosis, acanthosis and papillomatosis thus confirming a VHA type 3 according to the classification of Levy–Frankel.[1]
We performed a surgical shaving of the right nipple and areola; we also performed surgical resection of the left areola without shaving of the left nipple [Figure 2]. The areolae were repaired with skin graft from the internal surface of the thigh under general anaesthesia. The patient was discharged the next day. Histology testing in the surgical material confirmed the initial diagnosis.
- Surgical shaving of the left nipple and areola
Two years after operation, the patient is well; there is no evidence for a recurrence of the disease [Figure 3].
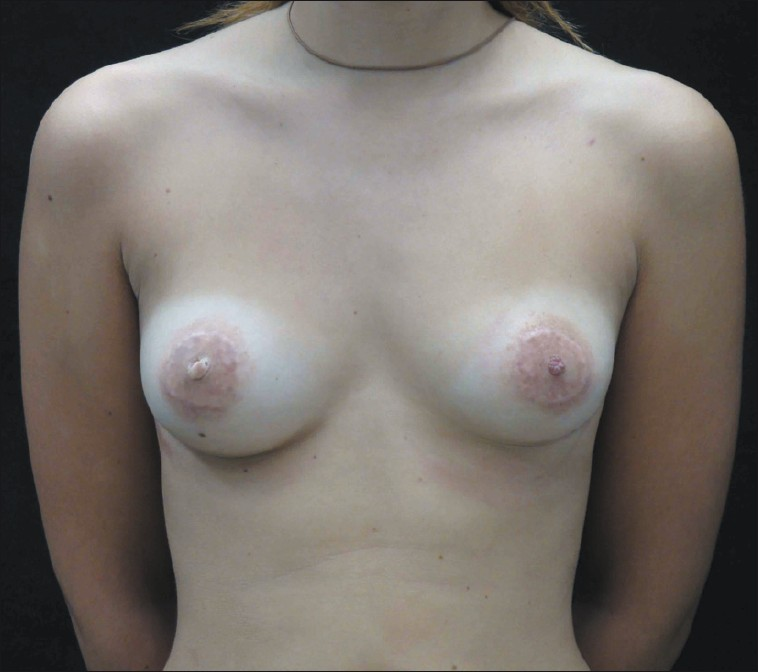
- The patient 2 years after the surgery
DISCUSSION
NHNA is a rare condition of unknown aetiology. So far, less than 90 cases, mainly sporadic, have been reported in the literature.[2] . It mostly affects women in the second or third decade of life, mainly during pregnancy. It can also occur in males.[3]
NHNA can pose a serious aesthetic and psychologic problem to the patient. It is believed that today it is more common than in the past; no evident explanation is provided for that, but it may be due to more accurate diagnosis.[4] The diagnosis is histologically confirmed; deferential diagnosis includes Paget's disease, superficial basal cell carcinoma, dermatophytosis and Bowen's disease.
Although it is considered as benign condition, it may accompany other more serious systemic disorders. According to Levy and Frankel, it can be classified into the following three types:[1]
-
Type 1: Hyperkeratosis of the nipple and areola representing an extension of a verrucosus (epidermal) nevus, usually unilateral in both sexes.
-
Type 2: Hyperkeratosis of the nipple and areola associated with other dermatoses such as ichthyosis, ichthyosiform, acanthosis nigricans, Darier's disease, cutaneous T-cell lymphoma, chronic eczema and erythroderma. It may also be a manifestation of graft versus host reaction (GVHR) following allogeneic bone marrow transplantation.[5] This type may be bilateral.
-
Type 3: This type is also known as idiopathic or nevoid hyperkeratosis of the nipple and areola. This unusual variant, according to Obayachi et al.,[6] mainly (80%) affects women in the age range of 20–40 years. It is usually bilateral and it affects both the nipple and areola in more than 70% of the cases. According to some authors, it may appear at puberty or during pregnancy in women, and in men treated with diethylstilbestrol for prostatic carcinoma. It may also be the result of hormonal disturbance(s).
The therapeutic options to NHNA can be summarized as follows:
-
Conservative approach includes keratolysis as salicylic acid 6%, lactic acid lotion, topical steroids, topical trietinoin, oral vitamin A and calcipotriol 2.
-
Non-conservative methods are cryotherapy,[7] laser[8] and surgery.[9]
The surgical management of NHNA was first applied by Mehregan et al. in 1977.[9]
In managing NHNA, one has to consider the need for restoring function and aesthetic appearance of the breast especially in the young. Surgery seems to be preferable due to a longer lasting and more aesthetically acceptable result. Our own case is now free of any discomfort or evidence for a local relapse. To the best of our knowledge, this case is the first reported one in the Greek medical literature.
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- Unilateral nevoid hyperkeratosis of the nipple and areola treated with topical calcitriol. Actas Dermosifiliogr. 2008;99:493-501.
- [Google Scholar]
- Nevoid hyperkeratosis of the areola in men: Response to cryotherapy. Dermatology. 1999;199:73-4.
- [Google Scholar]
- Hyperkeratosis of the nipple and areola: Report of 3 cases. Arch Dermatol. 2001;137:1327-8.
- [Google Scholar]
- Hyperkeratosis of the nipple associated with chronic graft versus host disease after allogeneic haematopoietic cell transplantation. Acta Derm Venereol. 2003;83:385-6.
- [Google Scholar]
- Naevoid hyperkeratosis of the nipple and areola in a man. Br J Dermatol. 2000;142:382-4.
- [Google Scholar]
- Treatment of hyperkeratosis areola mammae naeviformis with carbon dioxide laser. J Am Acad Dermatol. 1999;41:274-6.
- [Google Scholar]






