Translate this page into:
Necrobiotic Xanthogranuloma
Address for correspondence: Dr. Banavasi S. Girisha, Department of Dermatology, KS Hegde Charitable Hospital, Deralakatte, Mangalore - 574 160, Karnataka, India. E-mail: drgirishbs@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Necrobiotic xanthogranuloma is a rare, chronic, progressive granulomatous disorder which manifests as yellowish plaques and nodules, most commonly in the periorbital region. The exact aetiology is not known. It is commonly associated with monoclonal gammopathy. Various treatment modalities used include chemotherapy, intralesional and systemic steroids, radiotherapy and surgical excision. We report a case of necrobiotic xanthogranuloma involving the periorbital area causing cosmetic disfigurement.
Keywords
Necrobiotic xanthogranuloma
periorbital area
surgery
INTRODUCTION
Necrobiotic xanthogranuloma (NXG) is a rare, chronic, progressive granulomatous disorder. It manifests as yellowish plaques and nodules. The periorbital area is the commonest site of involvement. Extra-cutaneous involvement is also known.[1] A systemic association in the form of serum monoclonal gammopathy usually of IgG k and λ type is seen in 80% of the patients. There is also an increased risk of haematological and lymphoproliferative malignancies.[23] A recent study demonstrated Borrelia in NXG by focus floating microscopy, a modified immunohistochemical technique.[4] Approximately, 125 cases of NXG have been described in the literature till now.
CASE REPORT
A 61-year-old woman presented to our skin department with complaints of yellowish brown swellings around both the eyes since 5 years. These lesions were mostly asymptomatic other than the occasional itching. She also complained of restriction of her field of vision, which was worse on the right side. Lesions were gradually progressive in nature. On examination, there were soft to firm, non tender, yellowish brown nodules and plaques present over bilateral infraorbital areas [Figure 1]. They were not fixed to underlying tissues. Both upper eyelids were also involved with the yellowish plaques and nodules. An ophthalmological examination revealed swellings around the orbital area with involvement of lids and restriction of the temporal field of vision. The skin over the nodules and plaques showed few senile comedones and dermatosis papulosa nigra. A physical examination revealed that the patient had pallor but no associated regional lymphadenopathy or hepato-splenomegaly. On investigations, she was found to have anaemia (Hb, 7.7 g/dl) and raised ESR (45 mm at the end of 1 h). Her peripheral smear and bone marrow examination showed no significant findings. Her biochemical parameters were within normal limits. The coagulation profile and fasting serum lipid profile were also normal. Serum electrophoresis revealed no paraproteinaemia. Incision biopsy was done. Histopathology showed atrophic epidermis with dermis showing sheets of epitheloid histiocytic granulomas, numerous dispersed foreign bodies and Touton giant cells. These granulomas were seen entrapping the dermal structures. Focal lymphoid aggregates and degenerated collagen were also seen [Figures 2a and b]. Features were suggestive of NXG. Surgical excision was planned for lesions around each eye with a 2-week gap between the procedures. Both procedures were done under local anaesthesia. Lesions over upper eyelids were excised and wounds were closed with continuous sutures. Lesions over the infraorbital region were removed in the same way. However, considering the close proximity of the lesions to lower eyelids, subsequent eversion of the same and lack of skin in the inner canthus for wound closure, a repair using a flap was planned. A full thickness flap over the cheek was released and advanced [Figure 3]. Wound closure was done by continuous sutures. Suture removal was done after 7 days. She was followed up once in 2 months for 12 months, and still continues to be on follow-up. We did not observe any recurrence [Figure 4].

- Yellowish brown plaques and nodules around the eye
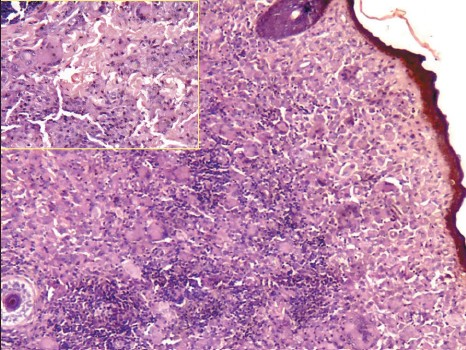
- Epitheloid histiocytic granulomas in the dermis with Touton and foreign body giant cells. The inset picture shows foci of the degenerated collagen with Touton giant cells
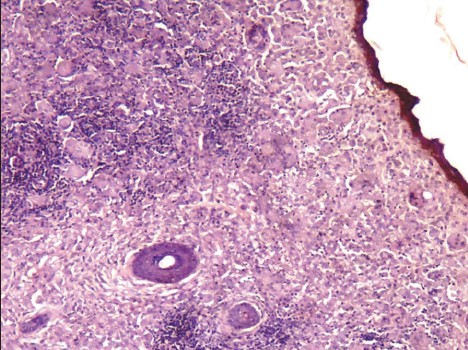
- Entrapped hair follicle with lymphoid aggregates (H and E, ×100)

- Intra-operative photograph showing the released full thickness flap over the cheek

- No recurrence after 1 year
DISCUSSION
Necrobiosis refers to the degeneration of collagen fibres. In 1980, Kossard and Winkelmann first distinguished NXG from normolipemic and hyperlipemic plane xanthomas. Several hypotheses have been postulated as the exact aetiology is not known.
Our patient presented with lesions involving the periorbital area which was a common finding noted by Mehregan and Winkelmann[1] in NXG. Our patient had involvement of upper eyelids and root of nose in addition. Associated symptoms like itching, burning and pain, or surface changes like ulceration seen in studies by Wood et al.[5] and Mehregan and Winkelmann[1] were not seen in our patient. Ocular manifestations can occur in about 50% of patients. They include burning, itching, blurred vision, diplopia and acute transient loss, periocular lesions, lesions in the anterior orbit, proptosis, blepheroptosis and restricted ocular motility.[1–3] Our patient had ocular findings in the form of lid swellings and visual field defect.
Monoclonal gammopathy was found in 23% of patients by Ugurlu et al. in their study.[2] Wood et al. reported a mean time of 2.4 years from the first appearance of NXG lesions to the development of haematologic disorders. They recommended continued surveillance for malignancies throughout life. Monoclonal gammopathy, plasmacytosis and multiple myeloma were noted in their study.[5] Despite the presence of NXG lesions for 5 years, no paraproteinaemia was observed in our patient.
Various modalities of treatment have been tried as there is no single well-established treatment available. Wood et al. reported chemotherapy as the most commonly administered treatment and found that chlorambucil and low-dose corticosteroids either alone or in combination were most effective. Other modalities of treatment tried are excision, melphalan, methotrexate and intralesional steroids.[12] Shaudig and Al-Samir reported surgical modality as a successful treatment modality with no recurrence during their 4 years of follow-up.[6] Ugurlu et al. reported a recurrence rate of 42% after surgical excision.[2] Such high recurrence rate may probably be due to the fact that most of their patients (77%) had associated paraproteinaemia. There are also reports where no relationship between the activity of skin lesions and the quantitative level of paraproteins was observed.[3] In our patient, the lesions were excised as they were cosmetically disfiguring and obstructing her visual field. No recurrence of lesions was observed even after 1 year of follow-up.
Currently, there is not enough evidence to prove the exact aetiology and the most effective treatment due to the rarity of disease. The choice of treatment needs to be individualized to the patient. Further studies focussing on the pathogenesis and evaluation of the therapeutic outcome are required for a better understanding and management of the disease.
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- Necrobiotic xanthogranuloma: Long-term outcome of ocular and systemic involvement. Am J Ophthalmol. 2000;129:651-7.
- [Google Scholar]
- Detection of spirochetal micro-organisms by focus-floating microscopy in necrobiotic xanthogranuloma. J Am Acad Dermatol. 2007;57:1026-30.
- [Google Scholar]
- Necrobiotic xanthogranuloma-A review of 17 cases with emphasis on clinical and pathologic correlation. Arch Dermatol. 2009;145:279-84.
- [Google Scholar]
- Upper and lower eyelid reconstruction for severe disfiguring necrobiotic xanthogranuloma. Orbit. 2004;23:65-76.
- [Google Scholar]






