Translate this page into:
Idiopathic Calcinosis Cutis of Nasal Dorsum
Address for correspondence: Ms. Shwetha Shenoy M, Department of ENT, KS Hegde Medical Academy, Derlakatte, Mangalore - 576 018, Karnataka, India. E-mail: shwetha_shenoy@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 23-year-old lady presented with a slowly progressing firm mass on the nasal dorsum since 8 months. Her biochemical, haematological and collagen vascular disease screening tests were normal. Radiographs of the nasal bones showed a subcutaneous calcifying lesion with no evidence of nasal bone erosion. A diagnosis of idiopathic calcinosis cutis (ICC) was made. The mass was excised and soft tissue defect was augmented with silicone prosthesis. The histopathology with the haematoxylin and eosin staining and von Kossa stain confirmed the diagnosis of calcinosis cutis. This is an unusual presentation of ICC involving the nasal dorsum requiring surgery and nasal dorsal augmentation with silicone prosthesis.
Keywords
Calcinosis cutis
idiopathic
nasal dorsum
INTRODUCTION
Calcinosis cutis is characterized by the deposition of insoluble calcium salts in the skin and subcutaneous tissue. It is classified into five subtypes: Dystrophic calcification, metastatic calcification, idiopathic calcification, iatrogenic calcification and calciphylaxis.[1]
Idiopathic calcinosis cutis (ICC) occurs in the absence of any metabolic disorder or tissue damage. ICC includes tumoural calcinosis, sub-epidermal calcified nodules and scrotal calcinosis.
The commonest sites of ICC include the scalp, extremities, joints and scrotum.[2]
ICC of the nasal dorsum is a very rare clinical entity. It has to be evaluated to rule out calcinosis occurring as a part of collagen disorders like CREST syndrome and systemic lupus erythematosis, dermatomyositis and inherited pseudoxanthoma elasticum.[3]
CASE REPORT
A 23-year-old lady presented to our hospital complaining of an asymptomatic subcutaneous nodule over the dorsum of the nose which had started about 8 months ago. The nodule had progressively grown in size over the past few months. There was no history of trauma. She gave a history of similar nodules over the scalp and great toes. The nodules over the scalp healed after discharging a chalky material. The nodules over the great toes were left untreated as the patient did not give consent for its evaluation as they were not cosmetically detrimental. There was no family history of similar lesions.
At the time of presentation, she had no complaints of joint pain, muscle weakness, skin rashes, Raynaud's phenomenon, dysphagia or dyspnoea. She was not on any medication and had not undergone any surgery [Figure 1].
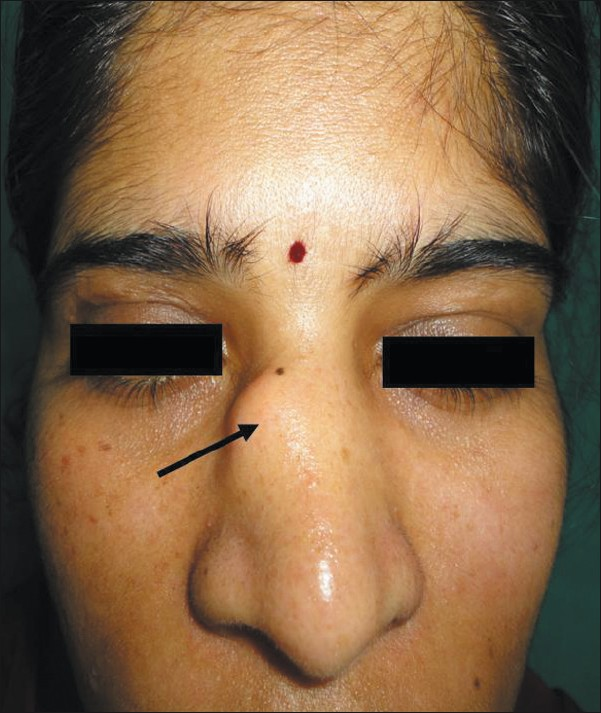
- The mass on the right nasal dorsum
On physical examination, we found a firm subcutaneous nodule measuring approximately 0.7 × 1 cm. Intra-nasal examination was normal. The systemic evaluations including the neurological examination were normal, and the patient had no symptoms such as muscle weakness or stiffness.
The laboratory investigations revealed within normal serum calcium levels of 8.6 mg/dl and phosphorus levels of 4.8 mg/dl.
Biochemical examinations gave normal results for a complete haemogram, erythrocyte sedimentation rate, blood sugar, uric acid, electrolyte, and liver function and kidney function tests. Routine urine examination was normal. Screening tests for collagen vascular disease, including anti-nuclear antibodies, anti-deoxyribo nucleic acid, anti-SM, anti nuclear cytoplasmic antibodies, serum C3, C4 and CH50 levels, and rheumatoid arthritis (RA) test were within normal limits. A radiological examination of the nose showed calcification at the region adjacent to the lower one-third of the right nasal bone with no bony invasion or erosion [Figure 2].
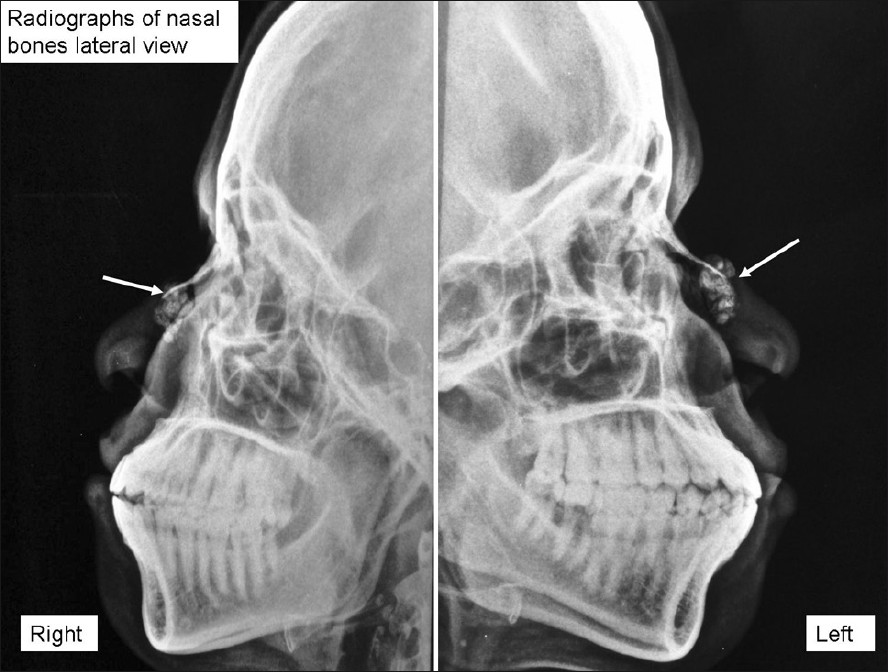
- Radiographs of the nasal bones showing subcutaneous calcification
The nasal mass was excised via an external approach. The mass was noted to be arising from the skin over the nasal dorsum and was overlying the lower one-third of the right nasal bone. There was no attachment from the mass to the underlying bone. The mass contained a pasty white material within it. After the excision, the soft tissue defect over the nasal dorsum was augmented using silicone block prosthesis [Figure 3].
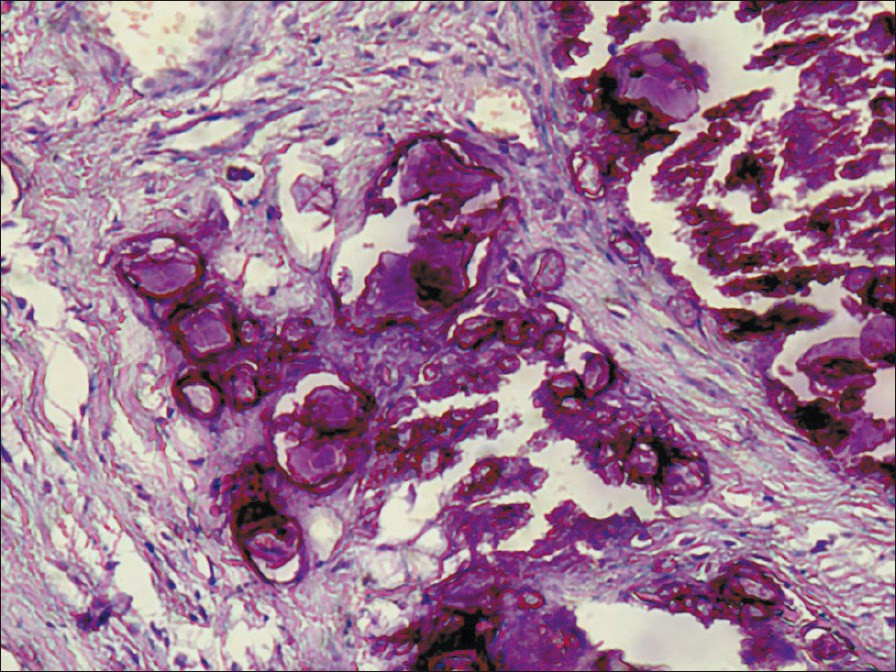
- Haematoxylin and eosin staining showing calcium deposits and foreign body reaction
The histopathology of the swelling (on haematoxylin and eosin staining) showed calcified nodules of varying size within the fibrotic tissue, and some areas were surrounded by foreign body cell reaction consistent with calcinosis cutis [Figure 4]. This was confirmed by von Kossa staining [Figure 5].
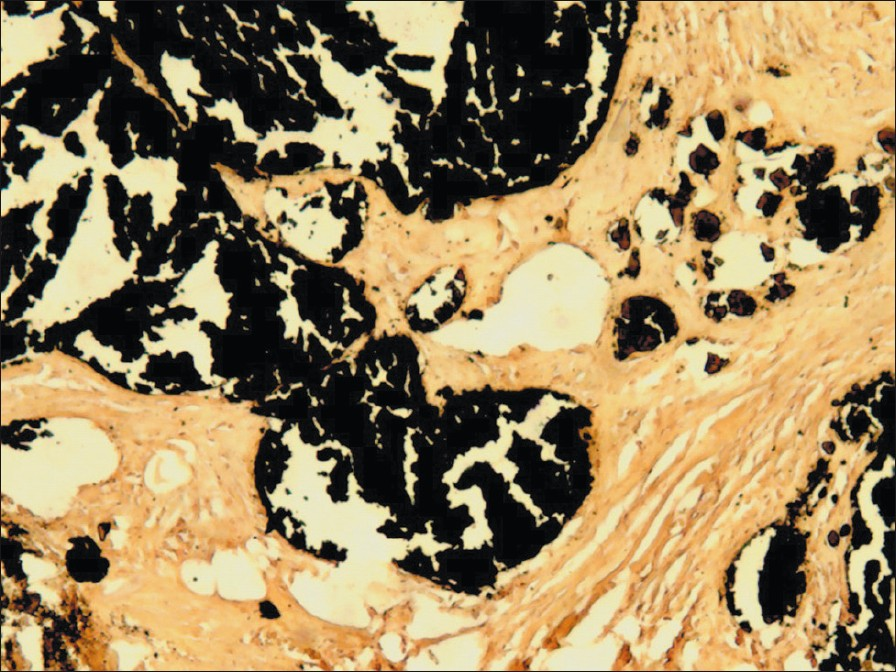
- Confirmation of calcium deposits with von Kossa staining (black deposits)

- Post-operative result after augmentation with silicone
On the basis of clinical, radiological and histopathology data, a diagnosis of ICC of the right nasal dorsum was made. Post-operatively, she was started on a bisphosphonate, ibandronate 150 mg once a month. The hospital stay was uneventful, and she patient was discharged after suture removal. She is presently asymptomatic and has no nasal deformity.
DISCUSSION
Cutaneous calcinosis is a rare dermatosis defined as the deposition of insoluble calcium salts in the cutaneous tissue. The different types are classified based on serum calcium and phosphorus levels. Dystrophic and idiopathic calcinosis cutis have normal calcium and phosphorus levels and occur due to local tissue trauma or abnormalities like dermatomyositis (dystrophic) or without any cause (idiopathic).[4]
Subcutaneous calcification occurs in 25–40% of patients with limited systemic sclerosis. Calcinosis cutis can be found in 30% of adults and in up to 70% of children and adolescents with dermatomyositis.[2]
Idiopathic calcinosis is subclassified into (a) tumoural calcinosis, characterized by masses around major joints mainly appearing in otherwise healthy adolescents; (b) sub-epidermal calcified nodules occurring on the head and extremities, the disorder being usually seen in children and (c) scrotal calcinosis.[1]
Metastatic calcinosis cutis is the spontaneous deposition of calcium and phosphate in normal tissues. It is characterized by increased serum calcium and/or phosphate levels or both. Primary hyperparathyroidism, hypervitaminosis D, renal failure, milk-alkali syndrome and destructive bone disease can cause metastatic calcinosis.[5]
Iatrogenic calcinosis is seen at sites of previous surgical incisions and due to infusions of calcium intravenously. Calciphylaxis is small vessel calcification mainly affecting blood vessels of the dermis or subcutaneous fat, seen in end-stage renal disease.[6]
Biochemical profile, collagen vascular disease screening and haematological investigation was normal. Our patient was diagnosed to have idopathic calcinosis cutis.
ICC occurs in the absence of any metabolic condition, inherited disease or tissue disorder. ICC may present as sub-epidermal calcified nodules occurring on the scalp, extremities and scrotum. They present mainly as solitary, hard, white-yellowish papules of size 3–11 mm. It is a disorder occurring in children and has been thought to represent calcified adnexal structures.[2]
Intensely basophilic sub-epithelial calcific deposits beneath the acanthotic, papillomatous epidermis are the pathognomic of ICC on histopathology. The deposits stain with the von Kossa stain for calcium. The foreign body giant cell reaction and transepidermal elimination of calcium granules can be observed.[7]
Differential diagnosis is made with milium, osteomas, warts, xanthomas, contagious molluscum, gout, perforans annular granuloma and epidermoid cyst.[8]
Curettage or surgical excision is the first-line therapy for ICC.[9] Indications for surgical treatment include painful masses, recurrent infection, ulcerations, functional impairment and cosmetic concerns.[10]
No pharmacological treatment is generally accepted as standard treatment to prevent or reduce calcinoisis. The treatment of calcinosis cutis suffers from a notable lack of controlled clinical trials. Warfarin, colchicine, probenecid, bisphosphonates and diltiazem have been tried. Newer advances in treatment include intralesional steroids, anti-tumour necrosis factor, intravenous immunoglobulins and extracorporeal shockwave lithotripsy.[11]
Bisphosphonates is a group of drugs which act by the way of inhibition of osteoclastic bone resorption and the decrease in bone resorption. It causes selective destruction of macrophages, inhibiting macrophage proinflammatory cytokine production (IL-1β, IL-6, TNF-α).[12] Bisphosphonates are therefore supposed to stop and partially reverse the calcifying process.
Our patient was diagnosed to have ICC. Her biochemical and collagen vascular disease screening was normal. She underwent surgical excision of the nodule and augmentation of the resultant soft tissue defect on the nasal dorsum with silicone implantation for cosmetic reasons.
CONCLUSION
This is an unusual presentation of ICC as it involves the nasal dorsum and required surgery and nasal dorsal augmentation with silicone prosthesis. To the best of our knowledge, this is the first case of ICC of the nasal dorsum requiring surgical excision and augmentation, to be reported.
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- Calcinosis cutis. Part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:12. quiz 13-4
- [Google Scholar]
- Calcinosis cutis in juvenile dermatomyositis responsive to aluminum hydroxide treatment. J Dermatol. 1993;20:558-60.
- [Google Scholar]
- Unusual idiopathic calcinosis cutis universalis in a child. Case Rep Dermatol. 2009;1:16-22.
- [Google Scholar]
- Pathogenesis of Calciphylaxis: Study of three cases with literature review. Hum Pathol. 1995;26:1055-64.
- [Google Scholar]
- Lever's Histopathology of the Skin (9th ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2005. p. :444-7.
- Idiopathic circumscripta calcinosis cutis of the knee. Dermatol Surg. 2003;29:1222-4.
- [Google Scholar]
- Calcinosis cutis. Part II. Treatment options. J Am Acad Dermatol. 2011;65:15-22. quiz 23-24
- [Google Scholar]
- Bisphosphonates: Mode of action and pharmacology. Pediatrics. 2007;119(Suppl 2):S150-62.
- [Google Scholar]






