Translate this page into:
Safe Practice of Cosmetic Dermatology: Avoiding Legal Tangles
Address for correspondence: Dr. Shilpa Bhat, Department of Dermatology, Victoria Hospital Fort, Bengaluru, Karnataka, India. E-mail: docshilpabhatholla@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The present day dermatologists, in addition to conventional skin physicians, are also dermatologic-surgeons and cosmetologists in their practice. The cosmetic procedures have the inherent risk of malpractice litigations leaving an unsatisfied patient and a troublesome lawsuit against the doctor. A MEDLINE search was conducted for article with words such as legal issues and dermatology, malpractice in dermatology, safe practice of cosmetology etc. The selected articles are scrutinized and compiled so as to help the young dermatologists to have a comprehensive overview of safe cosmetology practice. This article aims at sensitizing the young dermatologists for the possible complications and provides an overview of safe practice. It also provides a list of simple routine precautions which helps the dermatologist to avoid unnecessary trips to the courthouse.
Keywords
Cosmetic procedures
informed consent
legal issues
INTRODUCTION
The demand for cosmetic procedures is ever increasing.[1] In this modern era, cosmetic procedures are a fancy, a fashion; however, for some patients it is their profession which compels them to undergo cosmetic procedures. Many other factors also contribute to this upward trend including the economic growth and thereby improved affordability, the booming middle class with high disposable incomes, the revolution in the mass media and thereby increased awareness about cosmetic procedures as well as the increase in medical tourism.
Cosmetic procedures are ‘need felt.’ It is the innate desire to ‘look good’ that drives the patient to seek such aesthetic procedures. However, the treating dermatologist should not be over enthusiastic, and need not succumb to the needs of an insisting and highly demanding patient. It is always preferable to play safe rather than being too accommodative. For every procedure, its alternatives and outcomes have to be discussed in detail beforehand with the patient.
There is an ever growing list of dissatisfied clients and obliging lawyers targeting the doctors. Keeping in mind that the patient's safety is always of utmost importance, the doctor's interest should also be simultaneously safeguarded, as their intention is not to harm the patient. The dermatologists, who have newly ventured into the cosmetic procedures, should be extremely careful and smart in handling the legal issues arising out of such situations. Although misdiagnosis of cancer is the commonest litigation, the present day dermatologists are performing increasing numbers of cosmetic procedures and surgeries, which have the inherent risk of malpractice litigations.[2]
A MEDLINE search was conducted for articles with words such as legal issues and dermatology, malpractice in dermatology, safe practice of cosmetology etc. The selected articles were scrutinized and compiled so as to help the young dermatologists to have a comprehensive overview of safe practice.
Individuals seeking a cosmetic procedure are referred to as ‘clients’ or ‘customers’ as they are otherwise healthy. However, in this article, we prefer to use the term ‘Patient’ for those who seek advice and ‘Dermatologist’ for all those who perform the procedures. (Cosmetologist/Cosmetic physician/Medical cosmetologist/Aesthetic surgeon/Dermato-surgeon).
Cosmetic patients profile
Understanding the needs of the patients (cosmetic clients) and then proceeding to the specific management is most appropriate for a dermatologist as it helps in addressing the basic needs of the patient. Dermatologists encounter various types of patients in their practice. They can be classified as below.
Professional need-based clients
The profession demands ‘Good looks’ for this category of patients. Marketing professionals, receptionists, air hostesses, actors, singers, dancers etc.
Look good-feel good clients
These are the patients who want to have a clean and neat look by having a healthy looking skin that matches their age. Patients who seek treatment for seborrheic keratosis, DPN's and acrocodons fall into this category. They may also seek procedures such as peels, botulinum toxin and fillers.
Emotional need-based clients
These are the helpless people who look up for a helping hand from the dermatologist and expect a solution to their genuine medical and aesthetic problems by enhancing their outlook. Middle age crisis, neglected housewives.
Clients of special occasion
This is a category who wants to look good on certain special occasions. A young bride/groom to be, close relatives of the bride/groom etc.
Clients with psychiatric problems
This category of patients is easily victimized and ever dissatisfied as the real problem is in their minds! Hence, they are best treated by a psychiatrist. Patients with body dysmorphic disorder (BDD) fall into this category. These are the patients who go on a doctor-shopping spree. Rate of BDD are as high as 14% in cosmetic patients.[3]
Selection of patients
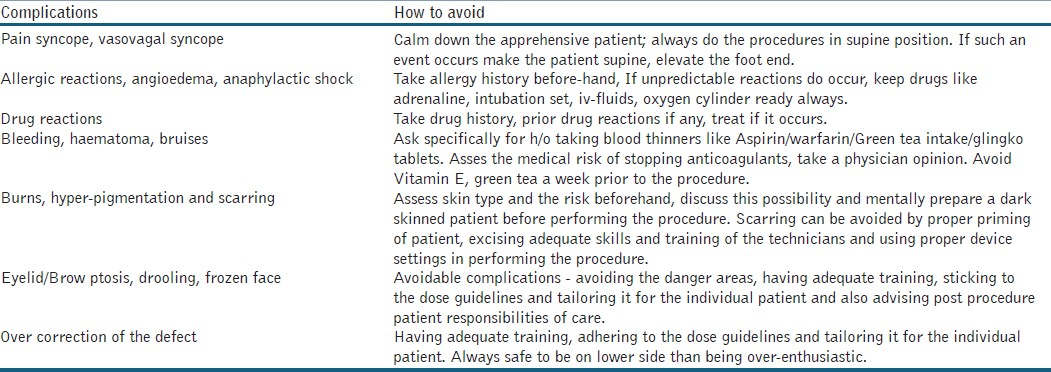
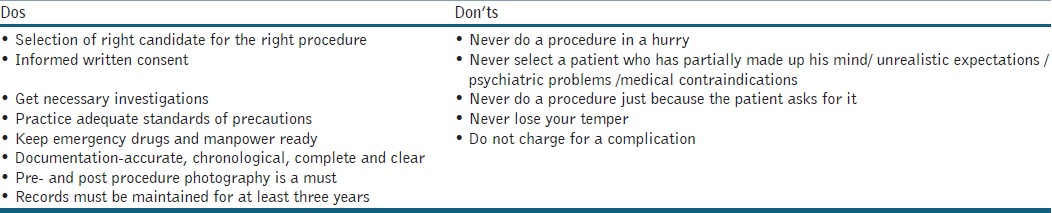
Choosing the right patient for a cosmetic procedure is the most crucial step. The expectations of the patient from the treating doctor needs to be assessed first. Patient's age, indication for the procedure, whether the expectations of the patient matches the expected outcome from the procedure, the possible complications [Table 1], are some of the basic considerations before any procedure. The doctor-patient relationship is always built on the foundation of ‘Trust’. Counselling the patient adequately is a mandatory pre-requisite and should be followed by a psychiatry consultation, though not a routine. Psychiatric disorders including BDD, narcissistic personality disorder and histrionic personality disorders are found among cosmetic patients. A basic understanding of the characteristic features of these conditions and pre-operative interview questions are valuable to dermatologic surgeons.[4]
It is useful to review past cosmetic interventions, including the number of previous procedures and their cosmetic and psychosocial outcome as perceived by the patients as well as family and friends. It is better to avoid patients who had numerous procedures performed by many practitioners, and particularly those who report the outcome of such procedures to have been unsatisfactory. Any history of legal proceedings or threats or overt violence towards previous cosmetic specialists is worrisome for the dermatologist.[5] Medical professionals who practice corrective dermatology should have a serious, non-profitable approach and select their patients carefully.[6]
Counselling
Adequate time should be given to this step. An adult patient can be accompanied by a friend /relative/parent in whom he/she has full faith. Children and adolescents must be accompanied by parents/legal guardian. It is an opportunity for the dermatologist to understand the needs of the patient and also to build up a rapport. The doctor's explanation and the patient's understanding of this explanation have been shown to improve the patient compliance.[7] One should put forth the available options to the patient and allow them to choose. In this stage important information should not be withheld, e.g., if a better/cheaper/more effective/safer procedure is available elsewhere. One need not undergo a laser just because the dermatologist has it! A detailed discussion about procedure goes a long way in winning their confidence as well as giving them the comfort of knowing the procedure beforehand. Doctor should discuss the advantages, disadvantages and adverse effects and the generally expected outcomes of the procedure chosen for the patient. Patient responsibilities like post procedure care, fees payable etc should also be discussed. One should encourage the patient to clarify their doubts. This interaction is equally important for the physician to know his patient and avoid a potentially dangerous patient. After all, choosing the right patient is an art! A patient who has consulted many doctors for a trivial issue, one who lacks trust, one whose questions appear never-ending, best way to treat them is to avoid them!
INFORMED CONSENT
Informed consent (IC) is important for ethical and legal reasons as well as to improve quality of care and patient satisfaction.[89] Presence of a witness is always preferred while taking IC. It should include the condition, need for treatment, other modalities of treatment, duration of given treatment, number of sittings, expected results; need to follow instructions before and after the procedure and possible side effects. Brochures designed to provide comprehensive, objective information for specific procedures can help physicians avoid malpractice claims. The consent should always be taken prior to the procedure and by the doctor only. It should be written in simple and comprehensible sentences and in the language which the patient understands better. It should be signed by the patient, parent/guardian in the case of minors. In the case of teenagers (13-18 years), it is better to take the consent of both the minor and the parent. The patient should have the liberty to revoke his consent at any time.
Consent forms are most protective for the provider in instances where unpredictable reactions occur after appropriate treatment. However, it does not provide immunity for the dermatologist from all guilt should an adverse event occur.[10]
The law of medical consent has been undergoing changes in recent years. Case law appears to be evolving towards a more patient centered standard of disclosure. Patient's expectations are higher and they are aware of the power of exercising their rights. Failure to obtain IC is one of the common allegations in medical malpractice suits.[11]
Pre-procedure work up
Adequate pre-procedure investigations should be done for all the cases including coagulation profile, complete blood counts, random blood sugars, ECG, pregnancy test for a woman in childbearing age and other necessary investigations depending on the history and clinical assessment. In addition to the medical history of the patient, a detailed account of the cosmetic procedures under gone in the past and the level of satisfaction from those procedures should be enquired [Table 2]. This can help the dermatologist to assess the expectations and level of risk. Patient's baseline state may have been altered by prior cosmetic procedures. Medical history should also include the factors affecting wound healing such as connective tissue disorders, diabetes and keloids. For example, a lady with hirsutism seeking laser hair removal may have underlying hormonal problems. Similarly, one who is seeking treatment for facial erythema may have an underlying lupus disease. Though such cases are encountered rarely, a dermatologist should have a watchful eye to pickup such cases. In doubtful cases, especially when dealing with nevoid lesions, dermatoscopy, Wood's lamp examination and even biopsy may be necessary before planning the surgery.
Patient's social history including occupation and recreational activities should be asked for. This helps the dermatologist to be conservative in the approach for professionals like actors and also whether the patient's lifestyle allows sufficient downtime for the procedure. History of smoking is very important as the wound healing process is hampered. Also, the drug history including over the counter drugs, antiplatelet drugs and vitamin E capsules (“blood thinners”) and consumption of green tea etc should specifically be asked for before any invasive cosmetic procedures that can result in excessive bleeding. Similarly history of use of topical retinoids before a chemical peel, use of isotretinoin before doing a laser resurfacing are vital as they affect the wound healing process. Evaluation of a cosmetic patient requires a good lighting, assessment of skin type and photo ageing.[10] Photographs should be taken from the same distance with similar lighting and magnification. In procedures where the size is to be reduced or enhanced, proper measurements should be documented. More specialized views of photographs may be required for procedures like hair transplantation, rhinoplasty etc.
Antibiotic/antiviral prophylaxis is important especially in those with a history of herpes. It is safer to give antiviral prophylaxis in all even if there is no previous history – especially if the procedure involves the face. A test dose of lignocaine is recommended if it is to be used in the procedure.
Procedure
The dermatologist must have adequate skills to perform the procedure. Such skills are acquired through specific workshops, certified courses and hands on training. The procedures should be “Tailor made” to suit the needs of the patient. High quality training in aesthetic procedures, knowledge of the possible complications [Table 1] and the ability to address them properly, along with the obligatory informed consent including photo-documentation form the framework of good practice.[6]
Standard of care practiced by a dermatologist should be based on current best evidence available.[12] Aseptic and universal precautions should be taken for all the cases. The operation theatre dimensions and guidelines of sterilization should always be followed while setting the dermato-surgery operation theatre. The dermatologist should always be prepared to handle any unforeseen events such as anaphylactic reactions, syncope etc. Communication with the patient remains vital during the procedure as the patient is conscious throughout. The probable complications should be explained in a gentle way even if that was discussed earlier. Post-procedure care can also be discussed.
A qualified assistant/nurse, referred to as “Physician extenders (PE)” is a valuable asset to a dermatologist. When adequately trained, they prove handy in the present day busy schedule of most practitioners.[13] PE's are highly prevalent in dermatologic surgery practices and are playing direct roles in the delivery of dermatologic care. Promoting patient safety through appropriate extender supervision and reporting of patient outcomes are highly needed.[14]
Not only they are trained to handle the patients and perform procedures assigned to them, they should also be encouraged to report the errors when it occurs and not hide the facts for the fear of litigation. This facilitates the early appropriate intervention that could address the origin of poor quality practices. The treating dermatologist would be vicariously liable if such events are not properly handled.
Medical record documentation is as important as performing the procedure skillfully. The operation notes should list all the steps and also the materials used for the procedure. It should also mention the date, time and signatures of the individual /team. It is considered as important evidence in the court of law.
POST PROCEDURE CARE
Post procedure care and patient responsibilities should be told clearly to the patient. Documentation of the advice is as important as the verbal communication. Physician should take great care to ensure complete and accurate records.[15] Many cosmetic procedures have a ‘down time’ which should be discussed with patient during counseling itself, should be told once again so that the patient is well aware of the events that would follow.
Patient should be asked to report if any unusual/unexpected events occur. The doctor should be available for contact for the early diagnosis and management of the probable complications.[16] It is advisable to accommodate these patients with some extra provisions in the schedule. Need for follow-up visits should be clearly told to the patients as lack of regular follow up may not ensure the desired results. Floating population should be avoided as for as possible.
WHAT TO DO WHEN SOMETHING GOES WRONG?
Even the most experienced and skilled dermatologist can have a bad day. Mistakes do happen even with the best hands!! In such a case, you are really better off acknowledging it. Be polite to the patient, listen to his complaints, counsel if necessary and redo or treat the patient. Above all do not charge the patient once again. By acknowledging, you may have a hassle on your hands, but you may not get to a lawsuit. Try to make an out of the court settlement if your defense is weak. This saves your reputation as well as the economic loss due to the time spent in attending the courthouse.[16]
In India, patients have an easy method of litigation as the medical profession has been brought under the provisions of the Consumer Protection Act, 1986. The Indian Supreme Court ruled in 1995 that doctors could be sued in India's consumer courts, for any service charged by the doctor. Only hospitals giving free service are exempted. A complaint can be filed in (1) the District Forum if the value of services and compensation claimed is less than 20 lakh rupees, (2) before the State Commission, if the value of the goods or services and the compensation claimed does not exceed more than 1 crore rupees, or (3) in the National Commission, if the value of the goods or services and the compensation exceeds more than 1 crore rupees.
An aggrieved patient can approach the consumer forum with a complaint of medical negligence within a period of two years from the date of cause of action. Once the complaint is filed, the forum decides whether the complaint is maintainable before it. If it is, it issues a notice to the doctor (‘the opposite party’), who is required to reply within 30 days. This is called as a written statement or version of the opposite party. The complainant is then allowed to file a rejoinder. Cross-examination is permitted in appropriate cases and affidavits can be filed. Whenever necessary, the forum may summon an expert to give evidence. It is always advisable to seek the advice of a legal advisor.[17] A proper legal reply from the doctor's side can alleviate the need to visit the courthouse, in case the patient has the intension of mere monitory gain!
WHAT MAKES THE PATIENT TAKE A LEGAL ACTION?
It is not always the actual surgical outcome that makes the patient sue the doctor. The patient's perception of his relationship with his/her doctor is the most important factor in deciding whether or not the patient will file a lawsuit against the doctor. A patient is more likely to sue if the patient perceives that his/her doctor is lacking in empathy and communication skills. Procedure not being performed properly, negligence on the part of the doctor and experimentations are other reasons for the patients suing the doctor.
“SAVE YOUR SKIN”
According to Dr. David J Goldberg, as long as you are doing what others are doing and not doing something unethical or as an outlier, you did not breach your duty. If there is no nexus between breach of duty and their alleged damages, they can take you to court, but they cannot win. A patient receiving an aesthetic procedure who sues a dermatologist over post procedure erythema that later resolves, for example, should not have a viable case.
The approach of the physician in dealing with the patient often determines whether postoperative problems are perceived by the patient as unfortunate complications or errors by the physician. An open, truthful, and caring approach by the physician can avoid unnecessary trips to the courthouse. Poor communication, retribution, economic gain and negligence are primary reasons that patients sue their physicians. Do your level best to minimize the damages!!
Cosmetic patients sue over hyperpigmentation and scarring. Selection of right candidate, good counseling, IC, sound knowledge of procedures, proper priming, ensuring patient compliance for post procedure care and follow-up are the basic considerations for any cosmetic procedure. Care should be taken to see that remedy should not be worse than the malady the patient had! Do not promise the patient that which is not achievable, just to make him undergo the procedure. Always promise less and deliver more!
SUMMARY
Dermatologists venturing into cosmetic procedures should be aware of the possible complications and the legal hassles that may arise. The law is different in various parts of the world, it is almost impossible to develop a method for whole world. The dermatologist should be aware of the local laws with respect to the dimensions of the clinic, the basic requirements of a specialty clinic (registration of the clinic, toilet facilities for patients, drinking water supply, waste management, medical record maintenance, taxes to be paid properly including service tax and other taxes like the VAT applicable to cosmetic procedures in India, periodic audits etc).
The aim of this article is to sensitize the dermatologist about the legal issues in their practice and to give the first hand look so as to maintain the standards in the practice, which would help in upgradation of the quality of care for the patients.
The message to the dermatologist of this cosmetic era is clear - A cordial doctor-patient relationship, empathetic handling of patients, proper counseling, proficiency in skills, and adherence to established guidelines are the best insurance against litigation. However, in this present era of consumer activism, it is recommended to avail professional indemnity insurance to cover the risk of allegations of medical negligence and its consequences.[18] By following some simple routine precautions and careful handling of a ‘difficult patient’ dermatologists can avoid unnecessary legal complications.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Dermatology: A medical, surgical and aesthetic profession. Isr Med Assoc J. 2008;10:404-5.
- [Google Scholar]
- The effect of medical malpractice on dermatology and related specialties. 2007. J Med Sci Res. 1:15. Available from: http://www.jmsr.org/index.php/journal/article/view/14/33
- [Google Scholar]
- Body dysmorphic disorder among dermatologic patients: Prevalence and clinical features. J Am Acad Dermatol. 2010;63:235-43.
- [Google Scholar]
- Understanding the psychology of the cosmetic patients. Dermatol Ther. 2008;21:47-53.
- [Google Scholar]
- How to protect medical professionals from unrealistic expectations of clients in corrective dermatology? Acta Clin Croat. 2010;49:509-13.
- [Google Scholar]
- Physicians’ communication skills with patients and legal liability in decided medical malpractice litigation cases in Japan. BMC Fam Pract. 2008;9:43.
- [Google Scholar]
- Legal issues in dermatology: Informed consent, complications and medical malpractice. Semin Cutan Med Surg. 2007;26:2-5.
- [Google Scholar]
- Quality of informed consent for invasive procedures. Int J Qual Health Care. 2008;20:352-7.
- [Google Scholar]
- Alum M, Gladstone BH, Tung R, eds. Cosmetic dermatology: Requisites in dermatology series. Edinbergh: Elseviers Publishers; 2009. p. :3.
- The role of a physician assistant in dermatologic surgery. Dermatol Surg. 1999;25:148-50.
- [Google Scholar]
- Practice models and roles of physician extenders in dermatologic surgery. Dermatol Surg. 2011;37:677-83.
- [Google Scholar]
- Physician's errors–legal advice for physicians accused of malpractice. MMW Fortschr Med. 2004;146:25-6. 28-9
- [Google Scholar]
- Association between physician explanatory behaviors and substandard care in adjudicated cases in Japan. Int J Gen Med. 2011;4:289-97.
- [Google Scholar]
- Safer practice of dermatosurgery. Indian J Dermatol Venereol Leprol. 2008;74:S75-7.
- [Google Scholar]






