Translate this page into:
Complications of Medium Depth and Deep Chemical Peels
Address for correspondence: Dr. Nanma Nikalji, 54 OPD, Skin OPD, 1st Floor, Dr. D. Y. Patil Hospital, Nerul, Mumbai, India. E-mail: drnanma@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Superficial and medium depth peels are dynamic tools when used as part of office procedures for treatment of acne, pigmentation disorders, and photo-aging. Results and complications are generally related to the depth of wounding, with deeper peels providing more marked results and higher incidence of complications. Complications are also more likely with darker skin types, certain peeling agents, and sun exposure. They can range from minor irritations, uneven pigmentation to permanent scarring. In very rare cases, complications can be life-threatening.
Keywords
Chemical peel
complications
superficial and medium depth
INTRODUCTION
Chemical peel is the most popular and common non-invasive cosmetic procedure done since the 18th century. The earliest use of caustic preparations for peeling procedures was described in the Egyptian medicine in the Ebers papyrus as early as 1550 BC.[12] Dermatologists began to show interest in peeling in the 19th century. In 1874 in Vienna, the dermatologist Ferdinand von Hebra used the technique to treat melasma, Addison's disease, and freckles. In 1882 in Hamburg, Paul G. Unna described the actions of salicylic acid, resorcinol, trichloroacetic acid (TCA), and phenol on the skin.
During the first half of the 20th century, phenol and TCA were used in several centers. Alpha-hydroxy acids (AHAs) became available as superficial peeling agents in late 1980s and the 1990s. AHAs are used in treating aging skin, melasma, photoaging and acne.
They are classified as superficial, medium, and deep peels. The superficial chemical peels are very safe when used properly but can cause itching, erythema, increased skin sensitivity, epidermolysis, allergic and irritant contact dermatitis, and post-inflammatory hyperpigmentation (PIH). All peels can cause activation of herpes viral infection, whereas medium and deep peels can cause scarring. Deep peels are no longer popular in Indian skin. They can cause milia, secondary infection, and scarring.
COMPLICATIONS OF CHEMICAL PEELS
Chemical peeling involves the application of a chemical agent of a defined strength that results in exfoliation of the skin followed by regrowth of new skin leading to skin rejuvenation. It is a technique-dependent procedure. Although rare, complications may occur including persistent erythema, milia, scarring, etc.[3]
CLASSIFICATION
-
Intraoperative[4]
-
Incorrect peel pharmacology
-
Accidental solution misplacement
-
-
Post-operative
-
Local infection
-
Contact dermatitis
-
Improper care during healing
-
Based on the time of onset, complications can be immediate or delayed.
-
Immediate (within minutes to hours after peeling):[5]
-
Irritation, burning, pruritus, and pain
-
Persistent erythema
-
Edema
-
Blistering
-
-
Delayed (within a few days to weeks):
-
Infections (bacterial, herpetic, and candidal)
-
Scarring, delayed healing, milia, and textural changes
-
Hyperpigmentation, hypopigmentation, and lines of demarcation
-
Loss of cutaneous barrier and tissue injury
-
Acneiform eruptions
-
Allergic reactions, toxicity, and ectropion
-
-
Accidental
-
Ocular complications.
-
Usually, complications are minor and are more common in dark-skinned individuals. They are seen more in medium and deep depth peels.
PAIN AND BURNING
Prolonged sun exposure, inadequate application of sunscreen, using topical retinoid or glycolic acid immediately after peels can lead to this complication. Paradoxically, in some patients, sunscreens can themselves cause contact sensitization or irritant dermatitis.[6]
Pain and burning is commonly encountered during a peel procedure in sensitive skin. It can persist up to 2-5 days after the peel till re-epithelialization is completed.
Treatment
-
Immediate ice application reduces the pain and burning sensation
-
Topical calamine lotion soothes the skin
-
Topical steroids such as hydrocortisone or fluticasone reduce the inflammation
-
Emollients to moisturize the skin
-
Sunscreens to prevent PIH.
Persistent erythema
It is characterized by the skin remaining erythematous beyond what is normal for an individual peel. Erythema disappears normally in 3-5 days in superficial peel, 15-30 days in medium peel,[4] and 60-90 days in deep peel. Erythema persisting beyond the above-mentioned time is abnormal and is an alarming sign. It is a predictor of potential scarring.
Causes
-
Usage of topical tretinoin just before and after peel
-
Isotretinoin administration (<0.5 mg/kg body weight) prior to peel
-
Minimal amount of alcoholic beverages[7]
-
Contact dermatitis
-
Contact sensitization
-
Exacerbation of pre-existing skin disease
-
Genetic susceptibility.
It is due to angiogenic factors stimulating vasodilation which indicates that the phase of fibroplasia is being stimulated for a prolonged period of time. Hence, it can be accompanied by skin thickening and scarring.
Treatment
-
Topical, systemic, or intralesional steroids if thickening is occurring
-
Pulsed dye laser to treat the vascular factors.
Pruritus
It is more common after superficial and deep peels, although may occur following re-epithelialization.[8]
-
It may be due to contact dermatitis to a topical agent (retinoid)
-
If papules, pustules, and erythema occur along with pruritus, it is suspected to be contact dermatitis and treatment should start as early as possible to prevent PIH
-
Care should be taken not to start any new topical agent during maintenance period after peel
-
If erythema with pruritus or burning or stinging, rule out active infection or flaring of an underlying skin condition.
Edema
It is more common with medium and deep peels occurring within 24-72 h of chemical peeling. In case of superficial peels, care should be taken while peeling patients with thin, atrophic, dry skin and in the periocular area since edema can occur in these settings because of deeper penetration.[8]
Treatment
-
Usually subsides spontaneously
-
Application of ice
-
Systemic steroids (short courses).
Blistering
It is more common in younger patients with loose periorbital skin and around eyes. Deeper peels, especially AHAs, can cause epidermolysis, vesiculation, and blistering especially in the sensitive areas such as nasolabial fold and perioral area. TCA 50% and glycolic acid 70% can cause blistering [Figure 1].

- Blistering seen post-chemical peel on cheeks
Prevention
The nasolabial folds, inner canthus of the eye, and corners of the mouth should be protected with petroleum jelly.
Ocular complications
Accidental spillage of any chemical peel agents in the eyes can cause eye injuries in the form of corneal damage.
Treatment
In cases of accidental spillage, the eyes should be flushed copiously with normal saline to prevent corneal damage. If phenol peels have been used, flushing should be done with mineral oil instead of saline. Referral to an ophthalmologist should be done.
Prevention
-
Extreme care should be taken while peeling the periorbital area
-
Dry swab stick should be kept ready to absorb any tears
-
Peeling agents should not be passed over the eyes.
Ectropion of the lower eyelid
It is usually seen after a Baker Gordon phenol peel.[8]
Predisposing factors
-
Older patients with senile lid laxity
-
Patients who have undergone previous transcutaneous blepharoplasty
-
Patients with thin skin.
Treatment
Most of the time the process is self-limiting and corrects spontaneously or with conservative care.
CONSERVATIVE CARE
-
Massaging of lower lid skin
-
Adequate taping of the eyelid, especially at night
-
Protection of the globe with artificial tears.[9]
INTRALESIONAL STEROIDS
Surgical repair
Prevention
Be cautious when using phenol in the periorbital area to avoid burning in the eye.
An assistant should always have a clean dry cotton-tipped applicator in his hand which should be used to absorb any tears that may drip down the face or into the temporal area.[9]
Inherent errors
-
Incorrect peel pharmacology
-
With resorcinol combinations, TCA, or phenol formulas, evaporation of the alcohol or water vehicle base can occur, inadvertently producing a stronger solution.
-
-
Accidental solution misplacement
-
Avoid accidental spillage of the solution
-
Never move the cotton-tipped applicators directly over the eye area
-
INFECTIONS
They are rare in TCA and phenol peels since these peels are bactericidal.
-
Impetigo and folliculitis (streptococcal and staphylococcal)
-
Pseudomonas or Escherichia coli infections.[10]
PRE-DISPOSING FACTORS
Prolonged application of biosynthetic membranes or thick occlusive ointments and poor wound care.
Clinical features
-
Delayed wound healing
-
Folliculitis
-
Ulceration, superficial erosions, crusting, and discharge.
Treatment of bacterial infections
-
Swab for culture and sensitivity
-
Appropriate antibiotics: Topical and oral
-
Wound cleaning with potassium permanganate soaks or acetic acid soaks three to four times a day
-
Topical mupirocin for gram-positive infections
-
Light debridement.
Candidal infections
-
Recent intake of oral antibiotics is often a pre-disposing factor
-
Superficial pustules can occur in candidal infections
-
Immunocompromised patients Diabetics
-
Oral thrush
-
Prolonged topical steroid use.
Treatment
-
Topical clotrimazole, 1%
-
Systemic anti-fungals (fluconozole, 50 mg/day).
Herpes simplex infection
It is characterized by reactivation of herpes simplex on face and perioral area presenting as sudden appearance of grouped erosions associated with pain.
Treatment
Active herpetic infections can easily be treated with anti-viral agents. A course of Valaciclovir, 1 g twice daily for 10 days may be given. If detected early and treatment is given on time, they do not scar.[11]
Prevention
Patients with a positive history of herpes simplex should be given 400 mg of acyclovir three times a day beginning on the day of the peel and continuing for 7-14 days, depending on whether it is a medium depth or deep chemical peel. Few recommend acyclovir 200 mg five times a day or valaciclovir, 1 g times a day starting 2 days before a peel and continued for 14 days. It is preferred to treat all patients with anti-viral agents regardless of a positive history as many patients do not remember prior herpes simplex infection that may have occurred years ago. A negative history of cold sores cannot predict development of post-operative herpes simplex virus infection after a procedure.[1011] Since all anti-viral agents inhibit viral replication in the intact epidermal cell, the drug would not have an inhibitory effect until the skin is re-epithelialized, which is 7-10 days in medium and deep peels. In the past, these agents were discontinued at 5 days and in these patients, clinical infection became apparent in 7-10 days.
Prevention of infections
-
Frequent post-operative visits should be done so that it can be ensured that appropriate home wound care is being performed and to minimize the risk of infection.
-
Avoid occlusive dressing in the immediate post-operative period because of its propensity to promote folliculitis and streptococcal and staphylococcal infections.
Delayed healing
Prolongation of granulation tissue beyond 1 week to 10 days signifies delayed healing. Presence of persistent erythema is a sign of the wound not healing normally. It could be due to the following:
Treatment
-
Treatment of infections already discussed
-
Debridement if necessary
-
Treatment of contact allergic or irritant dermatitis with steroids
-
Change of contact agents or protection with a biosynthetic membrane. Daily dressing along with a close watch on healing skin is a must.
Prevention
-
Strict sun avoidance and use of broad spectrum sunscreens before and after the peels indefinitely
-
Hypopigmenting agents (hydroquinone, kojic acid, and arbutin) should be strictly enforced in the post-peel period too.
Treatment
Triple combinations of hydroquinone, tretinoin, and steroids should be started once re-epithelialization is completed.
-
Hypopigmentation [Figure 2] superficial peels
-
Transient lighter complexion is seen due to sloughing off of the epidermis and removal of excess melanin.
- Hypopigmentation seen post-peel
Medium peels
-
More prolonged hypopigmentation because of removal of basal layer
-
Especially with 50% TCA and phenol peels.
Hyperpigmentation
It can occur any time after a peel and can be persistent, if treated inadequately. It is the most common complication of TCA peeling.
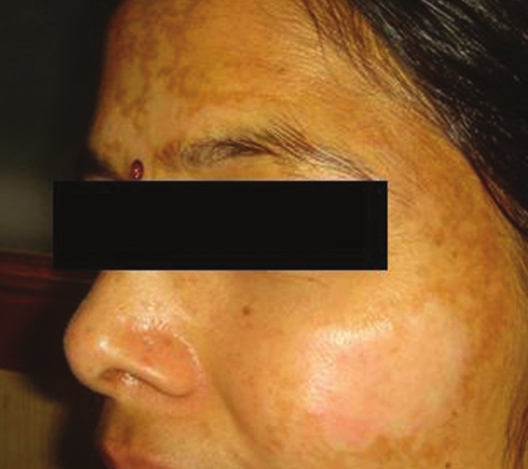
Complications from superficial peels are limited to transient hyperpigmentation or dyschromia especially in dark-skinned patients. With medium depth peels, irregular pigmentation can occur. Temporary accentuation of lentigines and nevi may also occur because the existing sun damage has been cleared. Patients should be warned that lesions like solar lentigines may initially disappear and then return after chemical peel. This occurs because the melanocytes that are responsible for pigmentation reside below the level of chemical peel [Figure 3].

- Hyperpigmentation post-peel
High-risk groups
-
Types III-VI skin
-
Types I and II skin following intense sun exposure and tanning or use of photo-sensitizing agents
-
Use of photosensitizing agents such as Non steroidal anti-inflammatory drugs, oral contraceptives, etc.
-
Early exposure to sunlight without adequate broad spectrum sunscreens
-
Estrogen containing medication, e.g., oral contraceptives and hormone replacement therapy
Treatment
-
Retinoic acid, 0.05% cream in combination with 4% hydroquinone once or twice daily for 3 weeks or longer if necessary
-
Hydrocortisone cream can be used for several weeks as needed if erythema due to retinoic acid poses a concern
-
Use of sunscreen with Sun protection factor 30.
In some cases, a superficial peel (glycolic acid, 30-40%) is used to hasten resolution.
Prevention
Good skin care regimens can sustain more long-lasting results though studies have shown that peeled skin returns to its baseline status within 2-6 months without maintenance therapy.
-
Strict sun avoidance and use of broad spectrum (ultraviolet A and B) sunscreens before and after the peels indefinitely
-
Pre-treatment with a depigmenting agent and tretinoin
-
In case of superficial peels, start at low strengths and titrate up very slowly
-
Cessation of use of birth pills during peripeel period because it may invoke pigmentary changes.
Incorporate broad spectrum sunscreens/bleaching agents (hydroquinone, kojic acid, arbutin)/retinoids/AHAs and beta-hydroxy acids/other anti-oxidant cosmeceuticals and bleaching creams singly or in combination as post-peel skin care regime.
Skin depigmentation
Bleaching effect can be seen after phenol peels. It is often noticed in the jaw neck region where untreated skin in the neck appears more obvious as it abuts the newly rejuvenated cheek or periorbital skin. This appearance may be desired in some but in patients undergoing regional facial peeling, this bleaching may become noticeable and troublesome. It is due to melanocytes losing their function to produce melanin.
Lines of demarcation
These are seen in medium and deep depth peels in darker skin types. They can be prevented by feathering edges using peeling agents of lower concentrations to merge with surrounding normal skin.
Milia
These are inclusion cysts which appear as a part of the healing process and are more common with dermabrasion than chemical peels. It is usually seen during the first few weeks of the recovery period. The post-peel care of deeper peeling may cause milia by occluding the upper pilosebaceous units with ointments. Thicker-skinned patients have been said to be in greater risk.
Treatment
Milia often resolve spontaneously with normal cleansing of the face. Sometimes, extraction or gentle electrodessication is effective.
Prevention
Returning to gentle epidermabrasion after re-epithelialization or the use of tretinoin both before and after peeling may retard their appearance.
Texture changes
Temporary appearance of enlarged pores post-peel can occur due to removal of stratum corneum. If the wounding agent is not capable of peeling below the defect, lacks the surfactant to provide an even depth of wounding, or has a very high surface tension, then uneven results will be produced from the selection of this inadequate wounding agent to peel below defect depth. Patients with telangiectasias may notice a worsening after phenol peeling which can be treated with vascular lasers.
Atrophy
It is characterized by the loss of normal skin markings in the absence of scarring. It may occur with phenol peels but has not been usually seen with superficial or medium depth TCA peels. Periorbital skin is very prone since it is physiologically thinner than most facial areas.[1]
INTRALESIONAL STEROIDS
Surgical repair
Scarring
Patchy erythema which may be indurated or persistent erythema can predict early scarring. The risk of hypertrophic scarring from medium depth peels is rare. If it occurs, it is most commonly seen along the mandibular region and in the perioral regions. TCA is more caustic than phenol and may be more likely to produce scarring [Figure 4].[13]

- Scarring seen on left cheek after peel
Predisposing factors
-
History of smoking
-
History of recent intake of 0.5 mg/kg isotretinoin (during the previous 12 months). Clinically, it is safe to perform a peel on patients after their skin begins to produce normal oil. Before performing any resurfacing procedure, most practitioners recommend to wait for 18-24 months after high-dose isotretinoin has been stopped, except in case of superficial peels. Low-dose isotretinoin in the dose of 10-20 mg three times a week is found to be safe and effective during the peel period.[14]
-
Recent facial surgery that required significant undermining
-
Recent ablative resurfacing procedures including dermabrasion or laser within 6 months of procedure. Since re-epithelialization occurs from adnexal structures, some authors have theorized that patients recently treated for hair removal with lasers may have trouble healing after medium or deep depth peels.[15]
-
Past history of keloids/hypertrophic scars.
-
Overzealous application of TCA
-
Medium depth peels on the areas like mandible, neck, and chest because these areas are more likely to scar
-
Thin-skinned patients are more prone for scarring because the TCA is more likely to penetrate deep into the reticular dermis.
Treatment
-
Scar massage
-
Topical/oral/intralesional steroids
-
Surgical revision after scar maturation
-
Pulsed dye laser therapy
-
Silicon gel sheet.
Systemic side-effects
Phenol peels can cause cardiac, renal, and pulmonary toxicities. The best management of these complications is to avoid them.
Cardiac arrhythmias
In patients deliberately face peeled with phenol in 30-min time, tachycardia was usually noted first followed by premature ventricular contractions, bigeminy, paroxysmal atrial tachycardia, and ventricular tachycardia. Some progressed to atrial fibrillation,[1617] Resorcinol resembles phenol in its systemic actions. Theoretically, similar complications might be induced if painted over one-third of body surface. A 40% peeling resorcinol paste applied daily for 3 weeks produced dizziness, pallor, cold sweat, tremors, and collapse on final application.[318] Resorcinol has an anti-thyroid activity. Hence, continuous application can cause myxedema. Repeated applications should be applied with caution in low body weight patients.
Laryngeal edema
Stridor, hoarseness, and tachypnea have been reported developing within 24 h of phenol peeling. It may be due to hypersensitivity reaction in a larynx already chronically irritated by cigarette smoke and may resolve with warm mist therapy. Anti-histamines prior to peel may prevent this.
Toxic shock syndrome
Physician should be alerted if patients develop fever, syncopal hypotension, vomiting, or diarrhea 2-3 days after a peel followed by scarlatiniform rash and desquamation. Other symptoms include myalgias, mucosal hyperemia, and hepatorenal, hematological or central nervous system involvement. Beta-lactamase-resistant antibiotics with large volumes of parenteral fluid should be given to prevent vascular collapse.[1920]
Prevention of complications
-
Select only skin types I and II for deep peel
-
Limit systemic levels of phenol due to absorption from skin
-
Intravenous hydration with 0.5-1 of fluid (lactated ringers) before and during procedure to enhance phenol excretion and avoid renal toxicity.[15]
-
Cardiac monitoring to detect any electrocardiography abnormality (premature ventricular contraction/premature atrial contractions).[21] In such cases, the procedure should be halted.
-
In a series of full face phenol peels, the incidence of cardiac arrhythmias was 6.6%.
-
Full face peels should be performed over a 60-90 min period of time. Each cosmetic unit (forehead, cheeks, nose, perioral, and periorbital areas) should be peeled in 15 min increments.[9] Peeling segments of the face in intervals with diuresis will allow metabolism and excretion of phenol and reduce arrhythmias.[3]
Intraoperative oxygen to prevent arrhythmias.
Allergic reactions
Allergic contact dermatitis is more common with resorcinol, salicylic acid, kojic acid, lactic acid, hydroquinone, etc.
Irritant contact dermatitis can be caused by glycolic acid. Any peel can cause irritant dermatitis when used with excessive frequency, inappropriate high concentration, and vigorous skin preparation using acetone or another degreasing solution.
Deeper penetration of peel
Predisposing factors
Beginning a regimen with tretinoin
Facial shaving
Use of exfoliating scrubs.
Prevention
-
Closely examine condition of skin
-
Elicit a good history from the patient prior to peel
-
Correct patient and peel selection
-
Priming of skin
-
Post-peel care and sun protection
-
Beware of habitual skin pickers
-
Beware of those who have a tendency for PIH
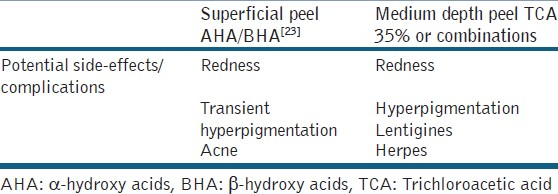
The complications of superficial and medium deep peels are summarized below [Table 1].
SUMMARY
Chemical peels represent a flexible and useful tool for improving skin texture and the effects of ageing. The level of expertise of a dermatologist is crucial for the rate of side-effects and for the final peel results. Superficial peels are easy to perform and their complications are rare if appropriate pre-peel and post-peel care is taken.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- The papyrus Ebers. New York: Hoeber; 1930.
- Prevention of complications in chemical peeling. J Cutan Aesthet Surg. 2010;3:186-8.
- [Google Scholar]
- Sunscreens. In: Handbook of Dermatological Drug Therapy (1st ed). New Delhi: Elsevier; 2007. p. :299-304.
- [Google Scholar]
- Complications. In: Step by Step Chemical Peels (1st ed). New Delhi: Jaypee Medical Publishers; 2009. p. :279-97.
- [Google Scholar]
- Chemical peels. In: Cosmetic Dermatology Vol 1. (1st ed). Saunders, Philadelphia: Elsevier; 2008. p. :97.
- [Google Scholar]
- Exacerbation of facial herpes simplex after phenolic face peels. J Dermatol Surg Oncol. 1984;10:57-8.
- [Google Scholar]
- Dermabrasion and chemical peel: A guide for facial plastic surgeons. New York: Thieme Medical Publishers; 1988. p. :43-54n.
- Chemexfoliation for aging skin and acne scarring. Arch Otolaryngol. 1965;81:278-83.
- [Google Scholar]
- Oral isotretinoin as part of the treatment of cutaneous aging. Dermatol Surg. 2000;26:649-52.
- [Google Scholar]
- Chemical peels. In: Alam M, Gladstone H, eds. Cosmetic Dermatology. Vol 1. Murad Alam: Hayes Gladstone; p. :83.
- [Google Scholar]
- Cardiac arrhythmias during phenol face peeling. Plast Reconstr Surg. 1984;73:590-4.
- [Google Scholar]
- Major electrocardiographic changes during chemical face peeling. Plast Reconstr Surg. 1979;63:44.
- [Google Scholar]
- Systemic reactions to topically applied drugs. Howard Fox memorial lecture. Bull N Y Acad Med. 1973;49:613-27.
- [Google Scholar]
- Chemical face peel complicated by toxic shock syndrome. A case report. Arch Otolaryngol. 1983;109:170-1.
- [Google Scholar]
- The importance of cardiac monitoring in superficial and deep chemical peeling. J Dermatol Surg Oncol. 1987;13:949-50.
- [Google Scholar]
- Chemical peels in aesthetic dermatology: An update 2009. J Eur Acad Dermatol Venereol. 2010;24:281-92.
- [Google Scholar]






