Translate this page into:
Cutaneous Angiosarcoma of the Head, Neck, and Face of the Elderly in Type 5 Skin
Address for correspondence: Dr. Moutusi Audhya, Department of DVL, Mahatma Gandhi Medical College and Research Institute, Pondicherry - 607 402, India. E-mail: drmoutusiaudhya@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cutaneous angiosarcoma is a rare, highly malignant vascular tumor with three clinical types. It is predominantly seen in the white-skinned people and rarely dealt with among the colored races. Cutaneous angiosarcoma of head and neck of the elderly is a great mimicker with many clinical presentations. The condition needs to be differentiated from several other common conditions and the diagnosis may be extremely difficult in some cases. Herein, we report the case of a 65-year-old man with type 5 skin who presented with an unusual and extensive involvement of the scalp and face presenting a diagnostic challenge.
Keywords
Cutaneous angiosarcoma
hematoma
type 5 skin
INTRODUCTION
Cutaneous angiosarcoma is a rare, highly malignant vascular tumor. There are three clinical types of cutaneous angiosarcoma which include angiosarcoma of head, neck and face of the elderly angiosarcoma associated with chronic lymphedema, and post-irradiation angiosarcoma. More than 50% of them are localized to the skin of the head and neck regions.[1] It is predominantly seen in the white-skinned people and rarely dealt with among the colored races.[2] Here, we report the case of a 65-year-old man of type 5 skin with cutaneous angiosarcoma of the head neck and face.
The report is unusual for the rarity of the condition in type 5 skin and also due to the extensive involvement of the patient.
CASE REPORT
A 65-year-old apparently healthy man was referred from the ophthalmology department and reported to us with a blackish swelling around his left eye of 1-month duration, associated with severe headache. He attributed it to the fall he had sustained 1-month prior to the onset of the swelling.
The lesions started as a papule over the left side of the scalp which started to bleed when the patient picked it and a few days later, he developed swelling around the left eye which was reddish and then turned black.
There was no history of fever, vomiting, loss of weight, or appetite.
On examining the patient's skin, a diffuse ill-defined dusky red, woody hard, hematoma-like swelling was noted around the left eye which extended up to the cheek. There was a marked edema of both eyelids, disabling the patient from opening his eyes [Figures 1 and 2].

- Solitary firm nodule with central ulceration over left parietal region and bluish red indurated plaques in the retro-auricular regions

- Eyelid edema with indurated plaques over both eyes
A reddish hue along with peau-de-orange appearance of skin of forehead was noted.
On the left parietal region of scalp, there was a solitary firm nodule with central ulceration (2 × 2 × 2 cm). Bluish red indurated plaques were present in the retro-auricular regions.
His general physical parameters were normal and all other systems were found to be within normal physiological limits.
We considered the provisional diagnoses of hematoma, cutaneous angiosarcoma of the head and neck of the elderly, and primary systemic amyloidosis.
During the 2 weeks' time while under our supervision, we visualized the evolution of the swelling to the other half of the face.
Investigations included complete hemogram with erythrocyte sedimentation rate, blood sugar, renal parameters, chest X-ray, ultra sonography test abdomen, computed tomography scan of the head, Echocardiogram and all were within normal limits. Skin biopsy (punch) from a representative site over the left forehead showed features suggestive of hemangioma. A repeat excisional biopsy of the excoriated nodule over scalp turned out to be cutaneous angiosarcoma [Figure 3]. Immunohistochemical study was positive for CD31, CD34, and Ki67, thus confirming the initial diagnosis of a high-grade cutaneous angiosarcoma.
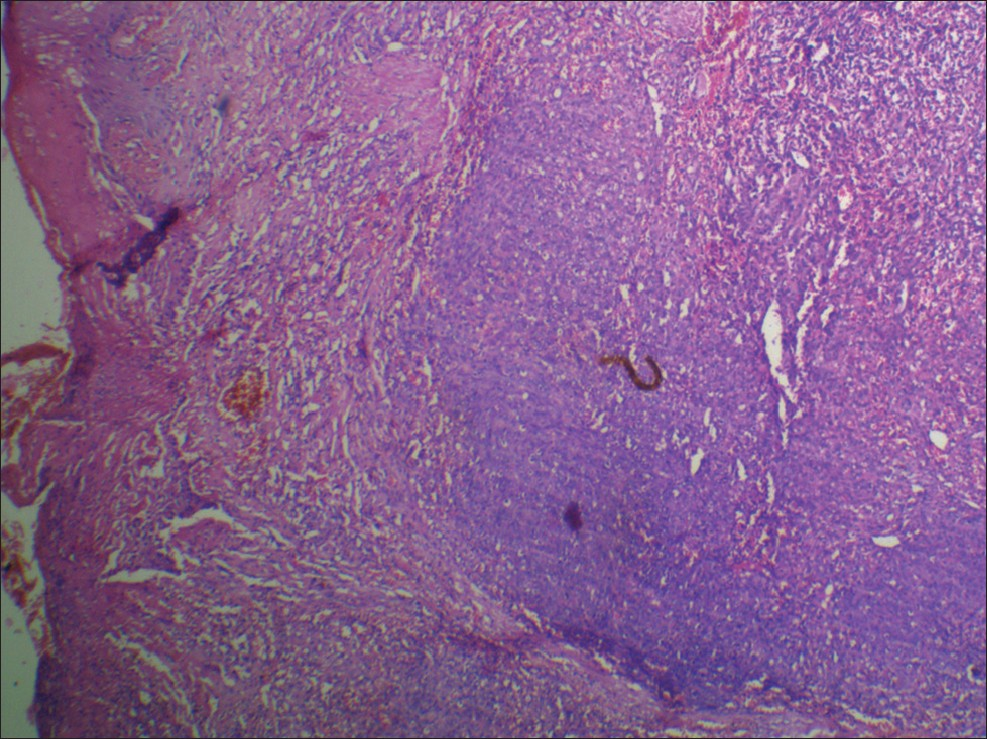
- Dermis showed an ill-defined tumor composed of anastomosing infiltrative vascular channels lined by crowded variably plump and atypical endothelial cells. The mitotic figures are 32 per 10 hpf. The lumen showed presence of RBCs
The patient was referred to a cancer institute where after appropriate discussion, he was started on radiation therapy. But the patient did not complete the treatment and was subsequently lost to follow-up.
DISCUSSION
Cutaneous angiosarcoma of head and neck of the elderly is a great mimicker with many clinical presentations which include bruise-like lesion, violaceous nodules and plaques, and flat infiltrating hemorrhagic areas. They may also mimic rosacea, xanthelasma, cellulitis, and facialangioedema.[13] At times, the clinical presentation can mimic hematoma.[4] Our patient presented with a hematoma-like lesion.
Advanced lesions may present as other malignancies such as squamous cell carcinoma, basal cellcarcinoma, malignant melanoma, and lymphomas.[5–7]
The involvement of the eyelid and the periocular region which was seen in our patient has been reported in only a few patients in the past.[8–13]
Angiosarcoma is a fast spreading tumor with the highest rate of lymph node metastasis among all soft tissue sarcomas of the head and neck.[14] Even though our patient had an extensive involvement of the scalp and face, the lymph nodes were spared and a thorough search for distant metastasis showed negative results.
However, literature also mentions that metastases to nodes or internal organs arises as a late complication.[15]
It is mentioned that in most patients, trauma alerts the presence of the lesion.[16] Our patient had a history of fall from his bicycle prior to the onset of the lesion. Trauma was involved in 27% of patients in a case series.[17] Though it is said that trauma is not responsible for the development of angiosarcoma, with a positive history in many patients, the authors doubt whether the relation between trauma and angiosarcoma is a mere coincidence.
Histologically, angiosarcoma has variable features. The well-differentiated lesions may be misinterpreted as hemangioma or lymphangioma, whereas the poorly differentiated lesions mimic melanoma.[18] As such, a definite diagnosis by histopathology may not always be possible. In such situations, immunostaining for markers will help in the diagnosis.
In our patient, CD31, CD34, and Ki67 were positive, favoring the diagnosis of a high-grade angiosarcoma.
Although complete surgical resection followed by wide-field radiation therapy has been established as a therapeutic standard for angiosarcoma, a delay in diagnosis and older age with comorbidities warrant for a safe and effective adjuvant treatment. Pegylated liposomal doxorubicin combined with radiotherapy seems to be a useful and safe alternative.[19]
Cutaneous angiosarcoma is a rare malignant vascular tumor and predominantly seen in the white-skinned people.[2] Very few cases have been reported in Indian patients. In our patient, the tumor was very extensive making surgical resection unlikely. Also the molecular immunology Borstel1 (MIB1) index and the Ki67 were high, suggesting a highly proliferative tumor. The previous case reports in Indian patients talk of a more localized variant with low proliferative index.[20]
Here, we would like to report this case for its rarity, especially in the dark-skinned individuals, the uncommon clinical presentation resembling a hematoma and the absence of metastasis in a fast spreading, extensive tumor.
ACKNOWLEDGEMENT
Dr. S. Krishnan, Professor and Head, Department of DVL, Mahatma Gandhi Medical College and Research Institute, Puducherry.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Cutaneous angiosarcoma presenting as an unusual facial bruise. Age Ageing. 2004;33:512-4.
- [Google Scholar]
- Prognosis of cutaneous angiosarcoma in Japan: A statistical study of sixty-nine cases. Chir Plastica. 1986;8:151.
- [Google Scholar]
- Cutaneous angiosarcoma of the face: Clinicopathologic and immunohistochemical study of a case resembling rosacea clinically. J Am Acad Dermatol. 1998;38:837-40.
- [Google Scholar]
- Infraorbital cutaneous angiosarcoma: A diagnostic and therapeutic dilemma. Head Face Med. 2008;4:18.
- [Google Scholar]
- Vascular tumors. In: Fletcher CD, ed. Diagnostic Histopathology of Tumors Vol 1. (3rd ed). Philadelphia: Churchill Livingstone; 2007. p. :41-81.
- [Google Scholar]
- Expression of Fli-1, a nuclear transcription factor, distinguishes vascular neoplasms from potential mimics. Am J Surg Pathol. 2001;25:1061-6.
- [Google Scholar]
- Vascular tumours. Cutaneous angiosarcoma. In: LeBoit PE, Burg G, Weedon D, eds. World Health Organization Classification of Tumours. Pathology and Genetics of Skin Tumours (1st ed). Lyon: IARC Press; 2006. p. :245-6.
- [Google Scholar]
- Angiosarcoma of the eyelid: Yellow plaques causing ptosis. J Am Acad Dermatol. 1996;34:308-10.
- [Google Scholar]
- Unilateral eyelid swelling as an initial manifestation of angiosarcoma. Hautarzt. 2000;51:419-22.
- [Google Scholar]
- Cutaneous angiosarcoma presenting as recurrent angio-oedema of the face. Br J Dermatol. 2000;143:1346-8.
- [Google Scholar]
- Angiosarcoma of the of scalp with calvarium involvement in a 50-year-old African-American man. J Natl Med Assoc. 2004;96:1507-12.
- [Google Scholar]
- Vascular tumor: Tumors and tumor-like conditions of blood vessels and lymphatics. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, eds. Lever's Histopathology of the Skin (9th ed). Philadelphia: Lippincott Williams and Wilkins; 2005. p. :1043-5.
- [Google Scholar]
- Cutaneous angiosarcoma of the head and neck: A case presentation and review of the literature. Ear Nose Throat J. 2006;85:672-4.
- [Google Scholar]
- An unusual case of the cutaneous angiosarcoma of the face and scalp. Hong Kong dermatol Venerol Bull 2003:209-13.
- [Google Scholar]
- Cutaneous angiosarcoma is a rare aggressive malignant vascular tumour of the skin. J Eur Acad Dermatol Venereol. 2011;25:964-8.
- [Google Scholar]
- Primary cutaneous angiosarcoma of the nose. Indian J Dermatol Venereol Leprol. 2012;78:496-7.
- [Google Scholar]






