Translate this page into:
Patient Profile and Outcome of Pilomatrixoma in District General Hospital in United Kingdom
Address for correspondence: Mr. Nader Naguib, Prince Charles Hospital, Merthyr Tydfil, CF47 9DT, United Kingdom. E-mail: nadernaguib71@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
A pilomatrixoma is a benign appendage tumour related to hair cells matrix. Most of the literature review about pilomatrixoma is in the form of case reports with fewer cohort studies. The objective of this cohort is to study the variable demographic characteristics, presentation and histopathology of this condition among a larger group of patients.
Materials and Methods:
We conducted a retrospective study of patients who had excision of pilomatrixoma between February 1998 and August 2011 in a District General Hospital in UK.
Results:
The study included 67 patients with histopathologically diagnosed pilomatrixoma. The mean age was 32 years. Male to Female ratio was 35:32. The average diameter of the lesion at presentation was 13 mm (range: 2–30 mm). 66 of 67 (98.5%) patients presented with solitary lesion, while 1 patient (1.5%) had two lesions.
Conclusion:
Pilomatrixoma is not an uncommon benign lesion. It is more common in the maxillofacial area.
Keywords
Pilomatrixoma
epithelioma of Malherbe
patient Profile
INTRODUCTION
A pilomatrixoma is a benign appendage tumor related to hair cells matrix. It was believed to be a rare tumor, but increasing reports in the literature show that it is not uncommon. Presently, pilomatrixoma is the most common hair follicle tumor. It usually manifests as a solitary, asymptomatic, firm nodule. It is more common in children, but occurrence in adults is increasingly being recognized. Most cases have been reported in patients from white racial background with slight female predominance.[1–4] The treatment of choice is always surgical excision. Multiple pilomatrixomata have been observed, mainly in association with myotonic dystrophy and less commonly with other conditions such as Gardner’s syndrome and sarcoidosis.[5–13] Pilomatrix carcinoma is a rare condition.[14–18]
Pilomatrixoma affects <200,000 people in the United States.[3] In the United Kingdom, pilomatrixoma accounted for 1:500 to 1:2000 histological specimens.[5] There were 37 cases published in Japanese dental journals between 1977 and 1994.[19] In Turkey, 15 patients were seen in a pediatric surgery clinic from 1984 to 1994.[1] In France, a retrospective study in one surgery clinic revealed 33 patients who had surgery for pilomatrixoma between 1989 and 1997.[2]
Most of the literature review about pilomatrixoma is in the form of case reports with fewer cohort studies. The objective of this cohort is to study the variable demographic characteristics, presentation, and histopathology of this condition among a larger group of patients.
MATERIALS AND METHODS
We conducted a retrospective study of patients who had excision of pilomatrixoma between February 1998 and August 2011 in the District General Hospital in UK. The study included 67 patients with histopathologically diagnosed pilomatrixoma. Only patients with confirmed pathology report of pilomatrixoma (post-surgical excision) were included. The study was a comparison between two groups: Pediatric-age and adult-age groups.
The following data were collected from patients’ notes and histology reports: Patients’ demographics, site of lesions, lesions characteristics, differential diagnosis, histopathological features, associated medical co-morbidities, family history, and recurrence whether at same site or at site other than that of the primary lesion. Statistical analysis was performed using Fisher’s exact test.
RESULTS
During the study period, 67 patients had surgical excision of skin lesions, which were confirmed to be pilomatrixoma by histopathology. Patient’s mean age was 32 years (age range: 2–84 years), with a male to female ratio of 35:32. The average diameter of the lesion at presentation was 13 mm (range: 2–30 mm), although 51 cases (76.11%) were less than or equal to 15 mm in size. A total of 66 out of 67 (98.5%) patients presented with solitary lesion, while 1 patient (1.5%) had two lesions. The location of the lesions is shown in Table 1.
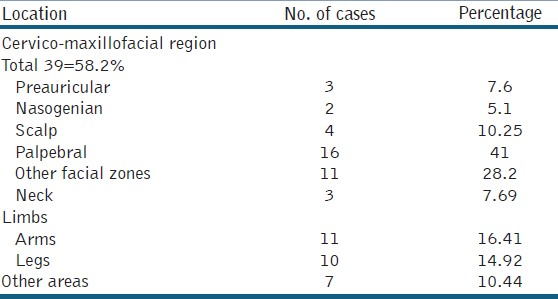
The most common clinical presentation was an incidental finding of a painless solitary skin lesion that was almost always firm to hard in consistency, well-circumscribed, freely mobile, and not attached to the underlying structures [Figure 1]. The lesion was attached to the skin in 8% of the cases. In few patients, the lesion was tender on palpation although this may not be reliable in the pediatric age group. Around 50% of the lesions were clinically diagnosed as sebaceous cysts.

- Pilomatrixoma of the left arm in a female child
There were 26 patients in the pediatric age group (<16 years) and 41 in the adult age group. The most common site in both the groups was the head and neck with no statistical differences between both the groups. There was also no statistical difference in gender distribution in either groups (P = 1). Similarly, there was no statistically significant difference between the male and female groups with regard to the site of the lesion (P = 0.32), with the head and neck being the most common site in both groups. No preoperative cytology or imaging investigations were done to the majority of the patients included in the study prior to surgical excision. One patient had a magnetic resonance imaging for a lesion in the upper arm, which was described as possible dermal tumor.
Simple resection and histological examination was performed for all cases where macroscopic appearance of the excised lesion showed the following: 18 lesions were described as skin nodules, 16 lesions were described as creamy or cheesy whitish to yellowish material, and 14 lesions were described as simple skin cysts. A single lesion was described as warty lesion, one as skin lesion with central pigmentation, one as skin lesion with central ulceration, and the remainders were described as non-specific tissue fragments. Calcification was macroscopically described in 7 cases.
All cases more or less shared the same microscopic features of ghost cells, calcification, and foreign body type giant cells, presenting features of a calcifying epithelioma of Malherbe (pilomatrixoma) [Figure 2].
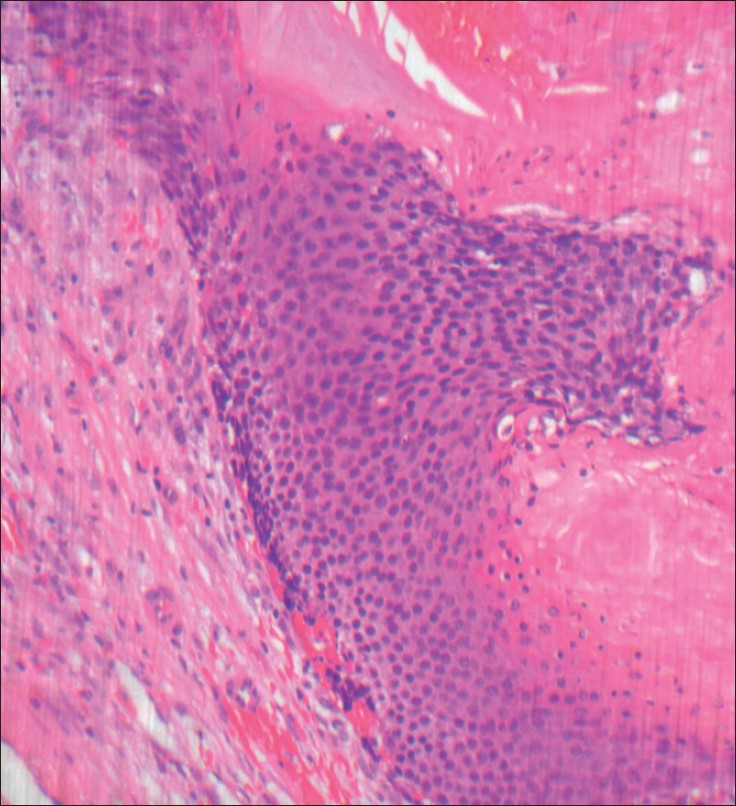
- Pilomatrixoma: Typical biphasic appearance with peripheral lobules of small darkly staining basaloid cells maturing into larger, pink æghostæ cells in the centre
Four patients had recurrence of skin lesion at the same site (3 of which had the same pathological diagnosis of pilomatrixoma and 1 was diagnosed as seborrheic keratosis at the site of previous pilomatrixoma excision). Rate of recurrence was 3/67 (2.01%). Recurrence occurred within 3-12 months (mean = 7 months).
Six patients developed pilomatrixoma at different sites and 2 patients had excision of various skin lesions from different sites (one was actinic keratosis with mild atypia and the other one was basal cell carcinoma “BCC”). No malignant transformations were reported in our cohort; hence, no regular follow-up was offered to the patients. As all patients belong to the same community group, they mostly presented to the same district hospital.
Patients’ notes and clinical portals were reviewed for all patients to identify any associated medical conditions or family history. There were no relevant past medical history or family history identified as a predisposing factor for the pilomatrixoma to occur.
DISCUSSION
Pilomatrixoma is the most common hair follicle tumor. Most of the literature reviews were case reports with fewer studies. Pilomatrixoma is more common in childhood, although it can develop at any age. In our study, it was more common in pediatric age group <16 years (26 cases) and adults between 30-60 years old (30 cases), while it was relatively less common in the old age group (only 5 patients >70 years).
In comparison to another study conducted in 2011 on 205 patients, our results were comparative in relation to gender (slight male predilection in our study), age, size, and number of the lesions.[20]
The most frequent locations were the head and maxillofacial zones (particularly the facial region), coinciding with observations of other case series.[21–24]
The treatment of pilomatrixoma comprises simple tumor resection.[25] Relapses are probably due to incomplete removal of the lesion, with a recurrence rate of 2–6%.[26] This range is almost the same as the relapse rate recorded in our series (2.01%). In some cases, due to the volume of the lesion or in the presence of adherences to the epidermis, skin grafts may be required to cover the resection defect.
Malignant change of pilomatrixoma is rare. In the literature, about 60 cases of malignant transformation have been documented until date. The principal indicators of malignancy are cellular pleomorphism, frequent mitotic figures or atypia, central necrosis, and infiltration of the skin, soft tissues, and lymphatic or vascular elements. The malignant version of pilomatrixoma is more frequent in males (with a ratio of 3:1) and in elderly individuals (60% were over 40 years in age).[27] Malignant pilomatrixoma had the same site distribution as the benign version of the tumor. Once the diagnosis was confirmed, management consisted of radical excision with adequate resection margins due to the high associated relapse rate in some studies.[27–29] There were no malignant changes in our study.
Distant metastases are rare, with only 6 cases described until date in the literature. Patient survival in such cases was 3-18 months from the time of diagnosis of metastatic disease.[2729]
CONCLUSIONS
Pilomatrixoma is not an uncommon benign lesion. It is more common in the maxillofacial area. Due to the benign nature of pilomatrixoma, simple removal of the lesion as a day surgery procedure is considered to be the treatment of choice, with a very low relapse rate.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Phil. Brumwell, consultant histopathologist and Clinical Lead, Cwm Taf LHB, Royal Glamorgan Hospital for his valuable time in providing the microscopic pictures of the clinical cases in this study.
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Pilomatrixoma of the head and neck in children: A study of 38 cases and a review of the literature. Arch Otolaryngol Head Neck Surg. 1998;124:1239-42.
- [Google Scholar]
- Pilomatrixoma: Patient report of a common childhood tumor. Clin Pediatr (Phila). 1993;32:749-50.
- [Google Scholar]
- Pilomatrixoma. 2010. E. Medicine. Available from: http://www.emedicine.medscape.com/article/1058965.overview
- [Google Scholar]
- Multiple pilomatricomas in association with myotonic dystrophy and a family history of melanoma. J Am Acad Dermatol. 1997;37:268-9.
- [Google Scholar]
- Multiple giant pilomatrix carcinomas of the head and neck. Otolaryngol Head Neck Surg. 1993;109:543-7.
- [Google Scholar]
- Multiple pilomatricomas and myotonic dystrophy in a patient with AIDS. Clin Exp Dermatol. 1995;20:423-4.
- [Google Scholar]
- Multiple pilomatrixomata and myotonic dystrophy: A familial association. Br J Plast Surg. 1999;52:143-5.
- [Google Scholar]
- Multiple familial pilomatricomas associated with myotonic dystrophy. Int J Dermatol. 1996;35:732-3.
- [Google Scholar]
- Multiple pilomatrixomas and myotonic dystrophy: A case report. Riv Neurol. 1988;58:124-6.
- [Google Scholar]
- Multiple pilomatricomas (calcifying epitheliomas of Malherbe) Pediatr Dermatol. 1984;2:23-5.
- [Google Scholar]
- Pilomatrix carcinoma with multiple metastases: Report of a case and review of the literature. Eur J Cancer. 1999;35:433-7.
- [Google Scholar]
- Pilomatrix carcinoma of the back treated by mohs micrographic surgery. Dermatol Surg. 2004;30:1174-6.
- [Google Scholar]
- Pilomatrix carcinoma: A report of a case arising from a previously excised pilomatrixoma and a review of the literature. J Am Acad Dermatol. 2001;44:358-61.
- [Google Scholar]
- Calcifying epithelioma (pilomatrixoma) of the head and neck: Analysis of 37 cases. Br J Oral Maxillofac Surg. 1997;35:429-32.
- [Google Scholar]
- Pilomatrixoma (calcifying epithelioma). A statistical study. Arch Dermatol. 1973;108:532-4.
- [Google Scholar]
- Pilomatrixoma of the head and neck in children: A study of 38 cases and a review of the literature. Arch Otolaryngol Head Neck Surg. 1998;124:1239-42.
- [Google Scholar]
- Malignant pilomatrixoma with multiple local recurrences and distant metastases: A case report and review of the literature. Clin Oncol (R Coll Radiol). 2001;13:386-9.
- [Google Scholar]
- Pilomatrix carcinoma with multiple metastases: Report of a case and review of the literature. Eur J Cancer. 1999;35:433-7.
- [Google Scholar]






