Translate this page into:
Aggressive Curettage-Cryosurgery for Human Papillomavirus-16 Associated Subungual Squamous Cell Carcinoma In Situ
Address for correspondence: Dr. Bo C Stenquist, Department of Dermatology and Venereology, Sahlgrenska University Hospital, SE-41345 Gothenburg, Sweden. E-mail: bossestenquist@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Squamous cell carcinoma (SCC) in situ is an uncommon tumour of the nail unit. Mohs micrographic surgery or wide surgical excision are often the preferred treatments. As an alternative therapy two patients with human papillomavirus (HPV)-16 associated SCC in situ were treated by curettage-cryosurgery. After a careful curettage with different-sized curettes freezing with liquid nitrogen in a double freeze-thaw was performed. Both patients were treated successfully and healed completely within 3 months. No adverse events were observed during a follow-up of at least 5 years and no recurrences were noted. Curettage-cryosurgery might be a safe and non-resource-demanding alternative treatment for patients with subungual SCC in situ.
Keywords
Curettage
cryosurgery
human papillomavirus
nail unit
squamous cell carcinoma in situ
INTRODUCTION
Squamous cell carcinoma (SCC) or SCC in situ are uncommon tumours of the peri- and subungual region. In this area SCCs in situ or Bowen's disease (BD) are frequently found as hyperkeratotic red patches, verrucous, crusted or even ulcerated lesions in the periungual zone.[12] However, often the malignancy also develops in the epithelium of the subungual tissue and there is a subsequent risk of invasive SCC, but metastases are rare.[3] Well-known aetiologies are high-risk human papillomavirus (HPV) in about 90%,[3] but ionizing or ultraviolet radiation, as well as arsenic could be a cause.
SCCs in situ of the nail unit are difficult to treat and even with wide surgical excisions or Mohs micrographic surgery (MMS) recurrences are not uncommon.[14] Fifteen and five years ago, respectively, we have treated two patients with HPV-16 DNA-positive subungual SCC in situ with a combination of meticulous curettage and cryosurgery (CC) as an alternative to suggested digit amputation.
CASE REPORTS
Case 1
The first patient was a 58-year-old female with a subungual BD on a finger. She had previously been described as having a patient-specific HPV-16 strain in archival sample from intraepithelial neoplasia grade II on the portio of the uterine cervix in 1970 and subsequently in a subungual BD of the left ringfinger.[5]
In 1995 an incomplete surgical excision of the subungual tumour was performed and therefore the surgeon suggested extirpation of the terminal phalanx. However, the patient, as being a pianist, wanted to try another form of treatment. In 1996 CC was carried out. After avulsion of the nail the tumour was found to cover most of the nail-bed. The patient had slight pain during the first few days after treatment but no analgesics were needed. Healing by secondary intention was without any complications. The final result was good with a well-functioning finger and with no recurrence after more than 5 years [Figures 1a–e].

- Treatment with curettage-cryosurgery of a subungual squamous cell carcinoma in situ of the left ring-finger – case 1 (a) Before treatment, (b) After a meticulous curettage the tumour was found to infiltrate most of the subungual zone, (c) The tumour area frozen with liquid nitrogen, (d) The result after 2 weeks, (e) The result obtained after 6 months
Case 2
The second patient was a 57-year–old male. Since 2000 he had had a periungual lesion on his right index finger. The diagnosis was SCC in situ or BD, in which HPV-16 DNA was found. Two incomplete surgical excisions followed by grafting were performed. Photodynamic therapy (PDT) was also tried a couple of times with insufficient result. Instead of suggested amputation of the distal phalanx he was referred for CC in 2006. Also in this patient the curettage indicated that most of the nail-bed was infiltrated by the lesion. Post-operatively the wound had healed within 3 months with no pain at all and after 5 years, no recurrence was found. There was no history of HPV-associated genital lesions on the patient or his wife.
Cryosurgical technique
After a proximal digital nerve-block (mepivacaine 10 mg/ml) avulsion of the nail was performed. Then a thorough curettage using different-sized ring curettes (Thiemann, New York, USA) was carried out. At first a large curette (no. 3) was used to remove the bulk of the tumour, then a medium-sized one (no. 2), and finally a small curette (no. 1) to remove any extensions of the malignancy. In both our presented patients, before the avulsion of the nail, the tumour was just seen a few millimetres outside the nail as a discreet superficial slightly scaling lesion [Figure 1a]. However, after the meticulous curettage the lesion was found to infiltrate most of the nail-bed [Figure 1b]. The curettage was a heavy-handed one according to Strum and Leider[6] implying a vigorous treatment not just a debulking procedure. When you perform the curettage you can “feel” that the soft tumour tissue separates from the firm and fresh basis. You continue the curettage until no more tissue can be separated. Of course there are small remnants of malignancy left [Figure 2] but these rests of tumour should be erased by the freezing. The curettage material was sent for histopathological examination, which confirmed the diagnosis SCC in situ. A cotton stick dipped in a 50% iron chloride solution was used for haemostasis.
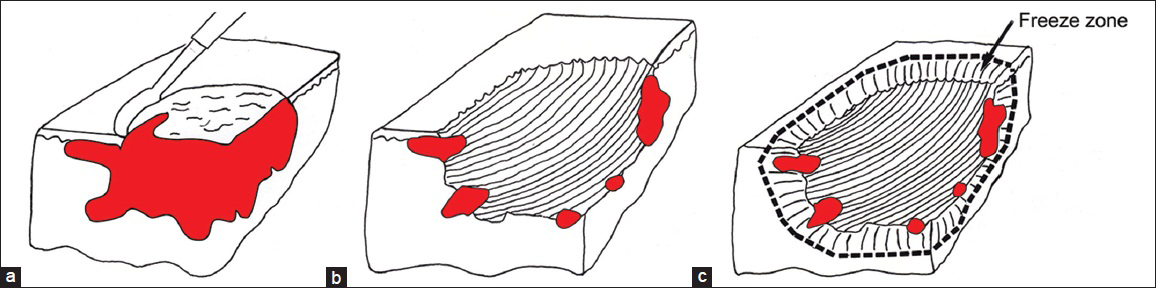
- Schematic view of the cryosurgical technique for subungual SCC in situ, (a) Curettage, (b) After the curettage still some small nests of tumour remain, (c) A double freeze-thaw cycle with liquid nitrogen will erase any tumour extensions
Then the freezing with liquid nitrogen (-196°C) in a double freeze-thaw cycle was carried out using a handheld Cry-Ac (Brymill Corp., USA). The spray tip, size B, was moved in circular motions over the treatment zone at about 1 cm distance until the lateral spread of freeze had reached a minimum of 5 mm outside the tumour border. The freezing was a maiximal continuous spraying of liquid nitrogen for 20-25 s, the halo thaw time was more than 60 s, and the complete thaw time was about 4 min [Figure 1c]. Thermocouples were not employed. The treatments were performed at a single out-patient visit by the same physician (PN). The patients were examined 2 weeks after treatment [Figure 1d], then at 3, 6 [Figure 1e], and 12 months and yearly for at least 5 years.
DISCUSSION
SCCs in situ in the peri- and subungual region often grow insidiously and are difficult to delimit. Different types of treatment have been used. The most preferred treatment modalities are MMS 47] and wide surgical excision.[8] However, the recurrence rates are higher than expected when treated HPV-associated digital SCC or SCC in situ.[3] Alternative therapies are PDT, [9] radiotherapy, [10] and cryosurgery, [1112] which have been more or less successful. In order to guarantee that all tumour strands have been removed and especially if bone involvement is found, amputation of the distal phalanx could be necessary. As alternative therapy we have used CC according to a method established for non-morpheiform BCCs on the nose [13] and on the ears [14] to successfully eradicate subungual SCC in situ on fingers in two patients.
A very important part of the this treatment is the meticulous curettage to delineate the tumour margins and remove the majority of the malignancy [Figure 2a and b]. The following freezing with liquid nitrogen in a double freeze-thaw cycle should eliminate any remaining tumour extensions and minimize the risk of recurrence [Figure 2c]. The treatment is performed during a finger block but no application of a bloodless field is necessary. The wound is left for healing by secondary intention and no grafting is needed. Both patients have been followed for at least 5 years with no recurrence.
Compared with extensive surgical excision and MMS, CC is a less resource-demanding out-patient procedure. A disadvantage with the powerful freezing is that the nail matrix will be destroyed, and thus no new nail will grow out. However, an advantage is that the risk of development of spicules could be minimized. This may be a problem after surgery.[8]
Another post-surgical complication is that the extensor tendon may be injured as it inserts into the base of the distal phalanx.[8] A great advantage with cryosurgery is that cellular tissue is more sensitive to cold than stromal tissue, implying that connective tissue, cartilage and bone, is affected but not damaged. Therefore the risk of injury of the extensor tendon as well as of the distal phalanx after the freezing would be minimal. Immunological response after the high freeze rate would also play a part in the healing process of these virus-associated tumours.[15]
Curettage-cryosurgery may be an alternative conservative therapy for subungual SCC in situ when wide surgical excision is insufficient and resources for MMS are lacking. Moreover, the risk for tumour recurrence could be reduced if a thorough curettage for tumour demarcation followed by freezing with liquid nitrogen in a double freeze-thaw cycle is performed.
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Bowen's disease of the nail bed and periungual area: A clinicopathological analysis of seven cases. Arch Dermatol. 1994;130:204-9.
- [Google Scholar]
- Squamous cell carcinoma of the nail apparatus:Clinicopathological study of 35 cases. Br J Dermatol. 2007;156:871-4.
- [Google Scholar]
- Human papillomavirus-associated digital squamous cell carcinoma: Literature review and report of 21 new cases. J Am Acad Dermatol. 2003;48:385-93.
- [Google Scholar]
- Mohs micrographic surgery of the nail unit and squamous cell carcinoma. Dermatol Surg. 2001;27:246-51.
- [Google Scholar]
- DNA analysis indicates patient-specific human papillomavirus type 16 strains in Bowen's disease on fingers and in archival samples from genital dysplasia. Br J Dermatol. 1997;136:678-82.
- [Google Scholar]
- Micrographic surgery for subungual squamous cell carcinoma. Br J Plast Surg. 1996;49:414-9.
- [Google Scholar]
- Subungual Bowen's disease treated by topical aminolevulinic acid-photodynamic therapy. J Am Acad Dermatol. 2005;53:S273-6.
- [Google Scholar]
- Cryosurgery for skin cancer: 30-year experience and cure rates. Dermatol Surg. 2004;30:297-300.
- [Google Scholar]
- Cryosurgery as adjuvant to Mohs micrographic surgery in the management of subungual squamous cell carcinoma. Dermatol Surg. 2011;37:256-8.
- [Google Scholar]
- Five-year results of curettage-cryosurgery of selected large primary basal cell carcinomas on the nose: An alternative treatment in a geographical area underserved by Mohs’ surgery. Br J Dermatol. 1997;136:180-3.
- [Google Scholar]
- Five-year results of curettage-cryosurgery for 100 consecutive auricular non-melanoma skin cancers. J Laryngol Oncol. 2002;116:893-8.
- [Google Scholar]
- Rate of freeze alters the immunologic response after cryoablation of breast cancer. Ann Surg Oncol. 2009;17:1187-93.
- [Google Scholar]






