Translate this page into:
Surgical pearl: The “dumbbell” technique: An attempt to simplify nail dressing
*Corresponding author: Muhammed Mukhtar, Mukhtar Skin Centre, Katihar Medical College Road, Katihar, Bihar, India. drmmukhtar20@gmail.com
-
Accepted: ,
How to cite this article: Mukhtar M. Surgical pearl: The “dumbbell” technique: An attempt to simplify nail dressing. J Cutan Aesthet Surg. 2024;17:337-9. doi: 10.4103/JCAS.JCAS_72_21
Abstract
A stable and less voluminous nail dressing is required after nail surgery over the nail unit. The bandage should take care of trauma, water and discharge from the wound. We described the use of two layered non-sticky and absorptive bandages. It was cut into dumbbell shape and wrapped over the toe with a nail, and tied at the base of the toe with moderate pressure. To observe the toe, a window is made in the center of the bandage.
Keywords
Dumbbell
Finger gloves
Nail dressing
Nail surgery
Nail unit
Toe
PROBLEM STATEMENT
Nail surgery is commonly done on the nail unit. After the procedure, a stable dressing of the nail unit is required, which is a major challenge. An ideal dressing should allow the mobility of the digit, protect the operated site from trauma and water, and absorb the postoperative discharge.1
The nail dressing is often very bulky and may fall off during the postoperative period. It should be less voluminous and tightly bandaged.2 Here a “dumbbell”- shaped bandage technique is used to simplify the nail dressing.
RECOMMENDED SOLUTION
To secure the dressing in place over the operated nail field, I have been using the “dumbbell”-shaped, two- layered bandage. In this technique, a nonabsorbent paraffin gauze and an absorbent gauze are put on each other to make a two-layered bandage. The proximal half part of the bandage is kept under the toe and the distal half is everted over the toe to cover the nail unit. Subsequently, both layers of the bandage are cut obliquely from the lateral edge to the side of the nail unit [Figure 1a-d]. On cutting the bandage, its shape is like a “dumbbell”. Then proximal part of bandage is wrapped and fixed on the ventral part of the toe with micropore or leucoplast on the base of toe, which gives stability and prevents dislodgement of the bandage [Figure 2a-c]. After this, the distal half of the bandage is wrapped and stabilized over the dorsum of toe in the same manner [Figure 2d-g]. The inner layer provides nonstickness to the site and the outer layer takes care of the discharge. Over the bandage, a cut-finger glove can be mounted, which gives further stability to the bandage and protects it from wetting. I found that this “2-in-1” bandage is more stable and limits the use of multiple layers and steps of bandage. In addition, the dressing technique is fast, simple and due to small- sized, it does not interfere the functions of the digit.
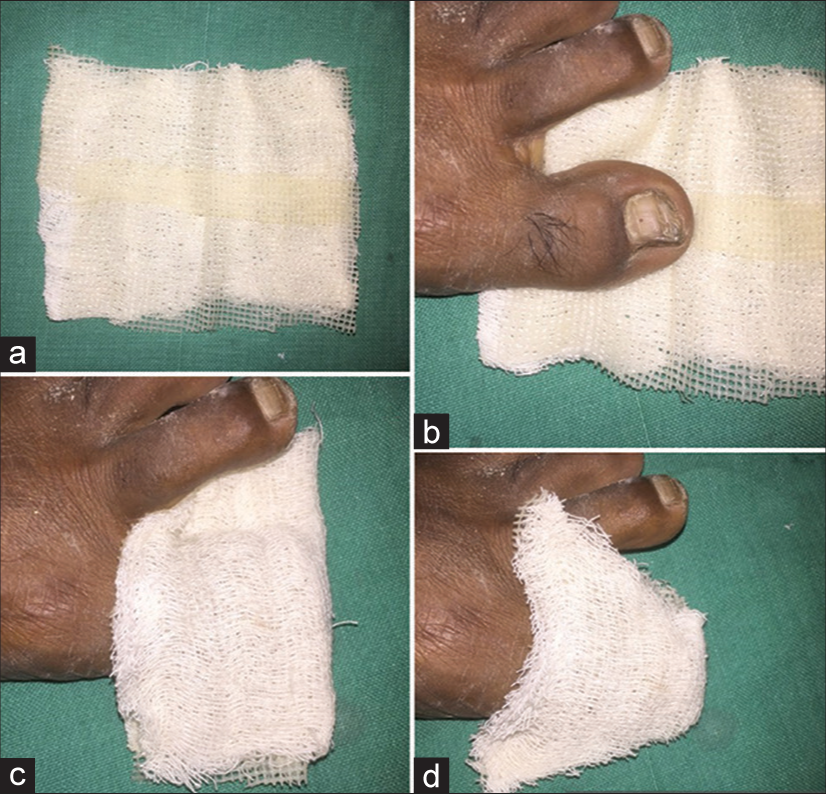
- (a-d) The double-layered (nonsticky and absorbent) bandage is made and put over the toe, and obliquely, the lateral part of the bandage is cut.

- (a-g) The dumbbell shape of two-layered bandage; the ventral part of the bandage is wrapped and (a-c) stabilized first on the toe and (d-g) then the dorsal part on the toe with the nail unit.
For visualization of the toe, a window can be created in the dressing [Figure 3a-c].

- (a-c) A window can be created to visualize the operated toe.
Authors’ contributions
Muhammed Mukhtar: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his/her consent for his/her images and other clinical information to be reported in the journal. The patient understands that his/her names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Ingrown toenails. Indian J Dermatol Venereol Leprol. 2012;78:279-89.
- [CrossRef] [PubMed] [Google Scholar]
- “Y” technique: An attempt to standardize nail dressing. J Am Acad Dermatol. 2018;78:e103-4.
- [CrossRef] [PubMed] [Google Scholar]






