Translate this page into:
Linear supravenous hypopigmentation secondary to intralesional corticosteroid injection
*Corresponding author: Muthu Sendhil Kumaran, Department of Dermatology, Venereology, and Leprology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. drsen_2000@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Meena A, Dev A, Bhandari A, Kumaran MS. Linear supravenous hypopigmentation secondary to intralesional corticosteroid injection. J Cutan Aesthet Surg. doi: 10.4103/JCAS. JCAS_183_22
Abstract
Intralesional steroid injections are used to treat several dermatological conditions, however such injections often lead to local side effects such as pain, hemorrhage and ulceration. Atrophy and hypopigmentation after intralesional/intra-articular injections of corticosteroids in a linear supravenous pattern is rarely reported in literature. We need to be aware of this rare side effect which can be alarming to the patient thus suitable patient guidance is necessary.
Keywords
Atrophy
hypopigmentation
linear
steroid
veins
INTRODUCTION
Intralesional steroid injections are used to treat several dermatological conditions; however, such injections often lead to local side effects such as pain, hemorrhage, ulceration, atrophy, pigmentary changes, calcification, secondary infection, granuloma formation, and allergic reactions. Few rare side effects include linear atrophy and hypopigmentation. We, hereby, report two patients recently seen.
CASE REPORT 1
A 22-year-old man presented with linear streaks of hypopigmentation on his right forearm for 4–5 months. He previously had a keloid over the dorsal aspect of the wrist for 1 year, for which he had received two doses of intralesional triamcinolone acetonide 40 mg/mL 5 months before presentation. Subsequently, the keloid resolved; however, 2 months after keloid healing, he noticed a hypopigmented patch over the dorsum of the hand, which started at the previous keloid site and gradually extended proximally along the forearm in an ascending manner along the course of superficial veins. Hypopigmented patch stabilized over a month without any further lesion progression. Clinical examination revealed two hypopigmented atrophic patches, linear in orientation on the dorsum of the right hand. This extended along the distribution of superficial veins along the extensor aspect of the forearm in a branching pattern [Figure 1a]. Dermoscopy showed an absence of a pigment network along with prominent eccrine openings [Figure 1b]. There were also overlying multiple telangiectasias arranged in a polygonal network. He was advised topical tacrolimus and on subsequent follow-up, repigmentation was noted [Figure 1c].
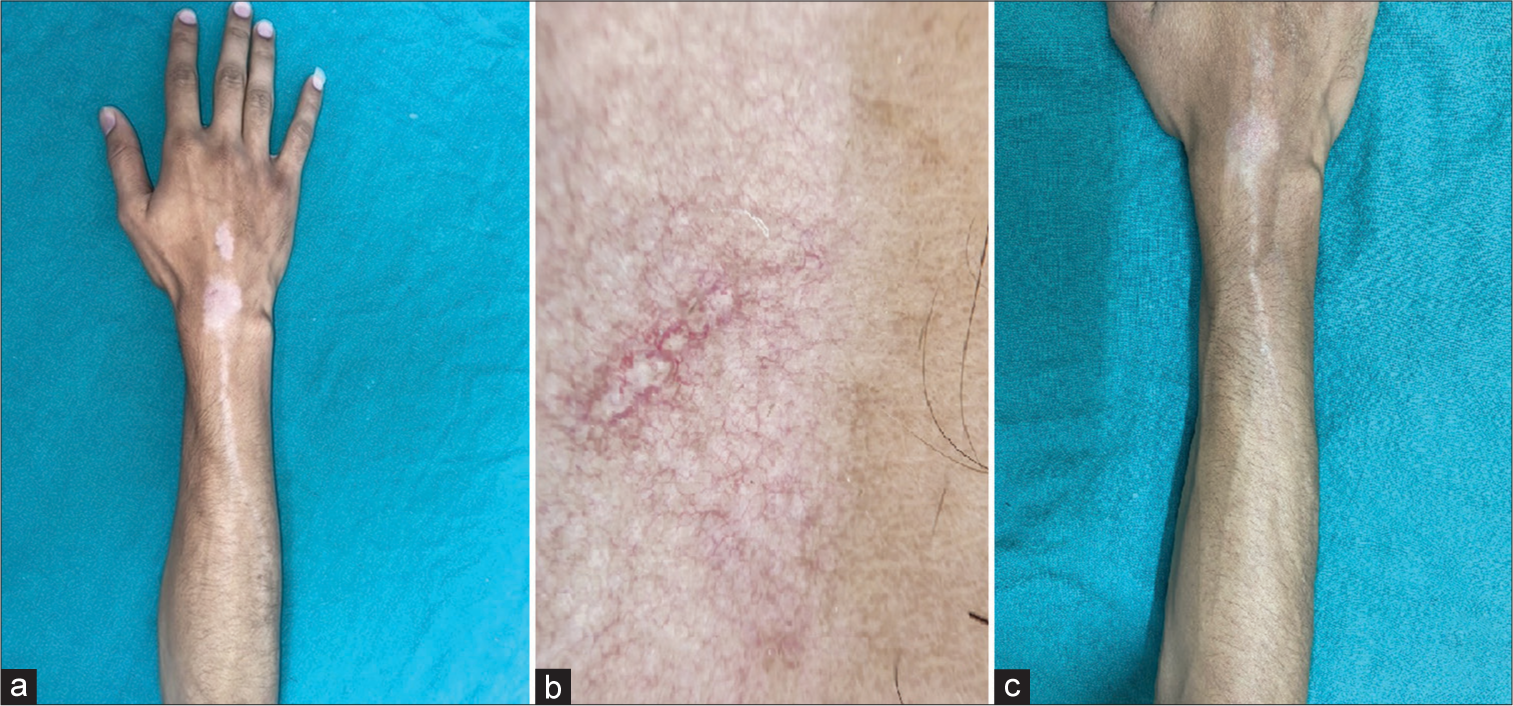
- (a) Depigmented patches on the dorsum of the hand and wrist in Patient 1 along with extension of the depigmentation along the forearm in a branching fashion along the course of the superficial veins. (b) Dermoscopy of the depigmented areas depicts loss of pigment network with overlying polygonal telangiectasias. (c) Repigmentation in the lesions after applying topical tacrolimus 0.1% for 1 month.
CASE REPORT 2
A 30-year-old male patient presented with expanding hypopigmented atrophic patch on his right elbow for 6 months. The patient had a hypertrophic scar on his right elbow following trauma, for which he had received three intralesional injections of 40-mg/mL triamcinolone acetonide 10 months before presentation. There was a significant improvement in scar following injections; however, 2 months later he noted a hypopigmented patch surrounding the keloid. Clinical examination revealed that a 1 cm × 2 cm atrophic scar was observed at the site of the keloid. The surrounding area was hypopigmented and atrophic in a stellate pattern. At the borders of the hypopigmented patch, there were also linear streaks of hypopigmentation along the course of superficial veins [Figure 2]. Dermoscopy showed similar findings of absence of pigment network, atrophy, and multiple polygonal vessels.

- Depigmented patch surrounding a treated keloid on right elbow. The depigmentation has occurred in a stellate fashion, extending along the superficial veins that have become more prominent due to atrophy.
DISCUSSION
Intralesional corticosteroid enables delivery of a high concentration of steroids at the lesional site, thereby avoiding any systemic adverse effects. They are commonly used in dermatological and nondermatological indications (Refer Box). However, cutaneous changes after local corticosteroid administration are common including dermal atrophy, hyperpigmentation, alopecia, and hypopigmentation.1 The development of atrophy and hypopigmentation after intralesional/intra-articular injections of corticosteroids in a linear supravenous pattern is rarely reported in the literature. Sharma et al.,2 Bjorklund and Fernandez Faith,3 and Liang and McElroy4 reported similar findings as ours.
Non dermatological indications of intralesional corticosteroids
| BOX | |
| Rheumatoid arthritis | Chalazion |
| Osteoarthritis | Allergic |
| Rhinitis | |
| Multiple sclerosis | Nasal polyp |
| Periocular capillary hemangioma |
The exact pathogenesis of corticosteroid-induced hypopigmentation is unknown. Multiple hypotheses regarding the linear extension of hypopigmentation have been proposed. One hypothesis suggested that corticosteroids inhibit prostaglandin production in the epidermis, thereby altering the melanocyte function without causing their destruction.5 Histopathology has shown reduced melanin in the presence of normal melanocyte numbers in these areas.6 Another hypothesis suggested that the linear extension of the lesions has been explained by the uptake of steroid crystals in the lymphatics, which cause localized lipolysis and depigmentation. Kikuchi and Horikawa7 demonstrated staining of the lymphatics on injecting blue dye in an area of steroid-induced atrophy. The supravenous distribution that was observed in both of our patients could be attributable to accidental extravasation or drainage of the drug into the perivascular tissues, adventitial layer of the superficial vein, or through the abnormal capillaries in keloid into the large subcutaneous veins.8
The depigmentation may persist long or even spontaneously repigment.5 The depigmentation becomes more prominent in the skin of color; hence, patients often seek immediate cosmetic correction and treatment with fear of being vitiligo. Modalities like topical tacrolimus, microneedling, saline and platelet-rich plasma injections, narrowband ultraviolet B, 308- and 10,600-nm laser phototherapies, melanocytekeratinocyte transplantation, and fat grafting have been tried to correct atrophy and hypopigmentation.9
CONCLUSION
As dermatologists often use intralesional steroid injections in various conditions, we need to be aware of this rare side effect, which can be alarming to the patient; thus, suitable patient guidance is necessary. It is often self-limiting and may respond to topical tacrolimus.
Authors’ Contributions
All the authors contributed to the research study. Akshay Meena: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Anubha Dev: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Adhyatm Bhandari: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Muthu Sendhil Kumaran: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
References
- Linear leucoderma following intralesional steroid: A report of three cases. J Cutan Aesthet Surg. 2015;8:117.
- [CrossRef] [PubMed] [Google Scholar]
- Delineating injectable triamcinolone-induced cutaneous atrophy and therapeutic options in 24 patients: A retrospective study. Indian Dermatol Online J. 2022;13:199-206.
- [CrossRef] [PubMed] [Google Scholar]
- Branching hypopigmentation following intralesional corticosteroid injection: Case report and review of the literature. Pediatr Dermatol. 2020;37:235-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hypopigmentation after triamcinolone injection for De Quervain tenosynovitis. Am J Phys Med Rehabil. 2013;92:639.
- [CrossRef] [PubMed] [Google Scholar]
- Perilesional linear atrophy and hypopigmentation after intralesional corticosteroid therapy. J Am Acad Dermatol. 1988;19:537-41.
- [CrossRef] [PubMed] [Google Scholar]
- Linear hypopigmentation and cutaneous atrophy following intra-articular steroid injections for De Quervain's tendonitis. J Drugs Dermatol. 2009;8:492-3.
- [Google Scholar]
- Perilymphatic atrophy of the skin: A side effect of topical corticosteroid injection therapy. Arch Dermatol [Internet]. 1974;109:558-9.
- [CrossRef] [PubMed] [Google Scholar]
- Linear hypopigmentation after triamcinolone injection: A rare complication of a common procedure. Aesthetic Plast Surg. 2006;30:118-9.
- [CrossRef] [PubMed] [Google Scholar]
- Stellate hypopigmentation in a pediatric patient after treatment with intralesionally-injected corticosteroid. Am J Case Rep. 2022;23:21-4.
- [CrossRef] [PubMed] [Google Scholar]






