Translate this page into:
Utility of Gel Nails in Improving the Appearance of Cosmetically Disfigured Nails: Experience with 25 Cases
Address for correspondence: Dr. Chander Grover, 420-B, Pocket 2, Mayur Vihar, Phase-1, Delhi - 110 091, India. E-mail: chandergroverkubba@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Gel nails are a commonly used cosmetic procedure, though their use by dermatologists has not been evaluated. These can be used to improve the appearance of cosmetically disfigured nails where other treatment options have failed; the condition is self-limiting or irreversible; or to camouflage the dystrophy until healing.
Materials and Methods:
A prospective, uncontrolled, open-label study on 25 participants presenting with cosmetically disfigured nails was undertaken. Mycologically negative, consenting patients with various nail plate surface abnormalities like trachyonychia (n =8); superficial pitting (n =6); onychorrhexis (n =4); superficial pitting with onychoschizia (n =3); Beau's lines (n =3) and pterygium (n =1) were included. The patients received gel nail application using Ranara gel nail kit®. Extra care was taken to avoid any damage to cuticle. Standard pre- and post-treatment photographs were taken to assess improvement. Patient satisfaction score (1-10); Global assessment score of improvement (no improvement to excellent improvement) and any side effects reported were recorded.
Results:
The average age of treated patients was 30.44±11.39 years (range 18-60 years). A total of 69 nails were treated (average of 2.76 per patient). Post-procedure, the average patient satisfaction score was 9.08 ± 0.86 (range 7-10). The Global assessment showed excellent improvement (40% cases); good improvement (56% cases) and mild improvement in the single case of pterygium treated.
Conclusions:
The use of Gel nails in patients with cosmetically disfiguring nail plate surface abnormalities (like trachyonychia, onychoschizia, pitting, etc.) was found to produce good to excellent improvement in most of the cases. The patient satisfaction with the procedure was rated as high. This, coupled with absence of side effects, make gel nails a valuable tool in improving cosmesis and satisfaction among patients presenting with nail plate surface abnormalities. Further studies with larger number of patients are required to assess the impact these prostheses can have.
Keywords
Abnormal nails
acetone
cosmetics
pitting
pterygium
trachyonychia
uv cured
INTRODUCTION
Gel nails are artificial nails used widely for aesthetic purposes, predominantly by manicurists and salons. In 1985, Wilde Cosmetics, USA, introduced their product Light Cured Nails (LCN); also known as gel nails. The basic constituents of these prostheses are ethyl cyanoacrylate and polymethyl-methacrylate monomers.[1] Although, their cosmetic use is increasing with each passing day, they have also been reported to be useful in conditions like nail biting, brittle nails and ingrown toe nails.[123] Gel nails are also used by musicians playing string instruments; however, their use as a therapeutic option in cosmetically disfigured nails has not been explored till now.
The present study was conducted to evaluate the utility of gel nails in patients seeking treatment for cosmetically disfigured nails, where a suitable treatment option was either not available or the severity of the disease did not justify its use.
MATERIALS AND METHODS
A prospective, uncontrolled, open-label study was conducted on dermatology out-patients, seeking treatment for cosmetically disfigured nails, during the period November 2012 to April 2013.
Study group
It included 18- to 60-year-old patients, seeking treatment for nail-plate surface abnormalities (ranging from mild pitting to more severe trachyonychia). Consenting patients, in whom intramatricial steroids or oral therapy were either contraindicated or refused by the patient themselves, were included in the study. Any patients with nail bed or fold abnormalities; active nail infection (in the form of onychomycosis, chronic or acute paronychia or nail warts); or those with isolated longitudinal melanonychia were excluded from the study. All participants were pre-evaluated with a mycological examination (with 10% potassium hydroxide mounts), which was required to be negative. Any previous history of allergic reactions to nail cosmetics or artificial nails was ruled out. The patients were explained regarding the procedure of application and possible side effects and were sensitised to the need for repeat applications.
Procedure
Baseline clinical photograph, using standard positioning and lighting was taken. The nail to be treated as well as the surrounding area was cleaned aseptically, followed by minimal buffing of the nail plate surface (just enough to make nail plate surface even) with a disposable nail file. Although pushing back the cuticle or nipping any extra cuticle is recommended and practiced in salons, we totally avoided any tampering with the cuticle.
We used Ranara® gel nail kit. This kit contains Primer solution, Natural gel, Nail cleaner, Nail file and Gel nail brush [Figure 1] [other popular companies providing these products include Shellac, Axxium, Gellish, Gelac and Gellez]. A drop of Primer solution® (methacrylic acid as the main constituent, 70% solvents and 10-30% adhesive agent) was applied on the prepared nail surface, allowed to spread on its own to cover the entire nail plate and dry for 1 min. Primer acts as double-sticking tape by forming covalent bonds between the nail plate on one side and nail gel, which was applied as the next layer. A single coat of Natural gel nail® was then uniformly applied, carefully avoiding contact with the cuticle or surrounding skin and was cured under a specialised portable UV lamp unit (Ranara®) for a standard duration of 2 min [Figure 2]. Post-curing, a cleaning solution (Ranara Eurocleaner® composed of a mixture of ethyl acetate, isopropyl alcohol and isobutyl acetate) was used to remove any excess gel or remnants and a post-procedure photograph was taken.
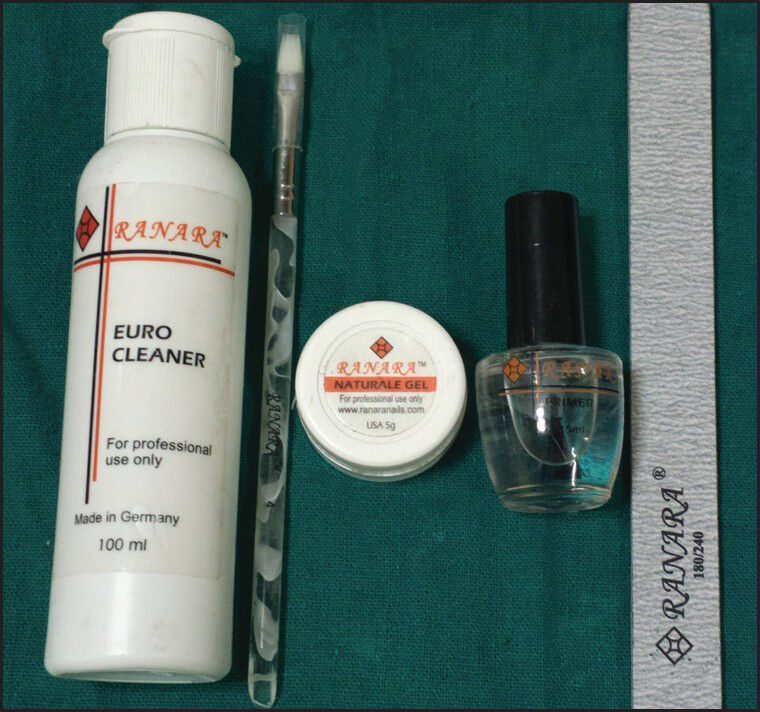
- Gel nail kit showing the key ingredients (left to right Nail cleaner, Nail brush, Gel, Primer solution and nail file)
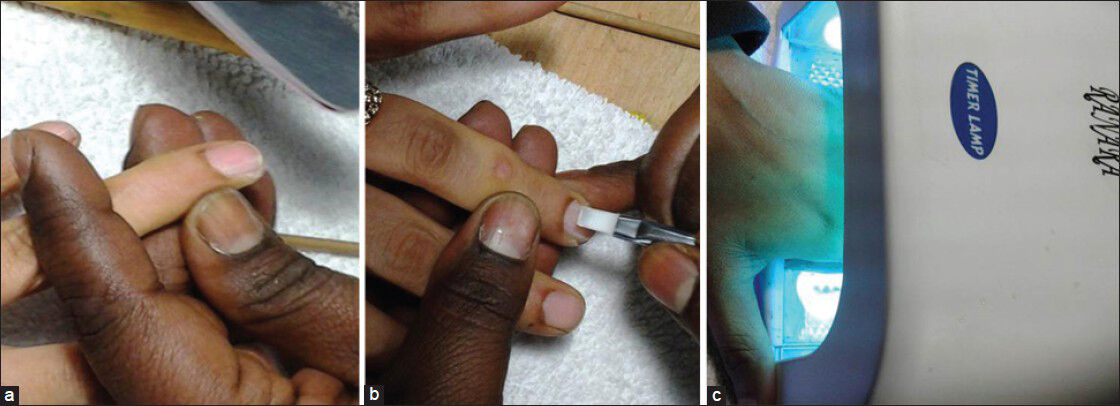
- The essential steps in applying gel nails. (a) Buffing of the nail plate surface with a nail file (b) Applying the gel nail (c) Curing the gel application in the specialised UV Lamp
Following the procedure, the patients could continue with their daily normal activities. They were advised to report back in case of any breaks or any pain or swelling in the paronychium. They were advised against acetone-based nail polish removers. Keeping the nails and nail folds well moisturised with bland emollients was a standard precaution, advised both during the 4 week period and thereafter. Any side effects to therapy reported during the 4 week period or thereafter, were recorded.
As per protocol, the gel nail was removed after 4 weeks. Normally, gel nail can be allowed to grow out if the cosmetic appearance is acceptable, but we removed it for study participants to examine the studied nail completely. Removal was done with commonly available, acetone based, nail polish remover, applied liberally with a cotton ball, and kept covered with kitchen foil for 10 min, helping the exothermic reaction. Subsequently, the gel nail was seen to loosen off and could be easily removed. The procedure was done in a well-ventilated room. Unlike acrylic nails, no infills were planned as the average thickness of gel nails (single coat) is very less and would not give a uniform appearance. The slight rough appearance of nail plate, seen in some patients, immediately after gel nail removal improved with use of moisturisers. Patients were advised to report back to the clinic after 1 week to evaluate the condition of the nail and discuss reapplication. Any discomfort or pain felt post procedure was to be reported immediately. For desirous patients, re-application was done after one week.
The response to the procedure (pre- and post-photographs) and patient's satisfaction with the results (at the end of 4 week period, prior to removal of gel nail) were rated on a visual analogue scale (scale of 0-10 with 10 being the highest satisfaction). A Global Assessment of the degree of improvement with gel nail, as assessed by independent physician, on the basis of standard photographs, was also recorded on a 4 point scale (Grade 0 = no improvement or worsening, Grade 1 = mild improvement, Grade 3 = good improvement and Grade 4 = excellent improvement).
RESULTS
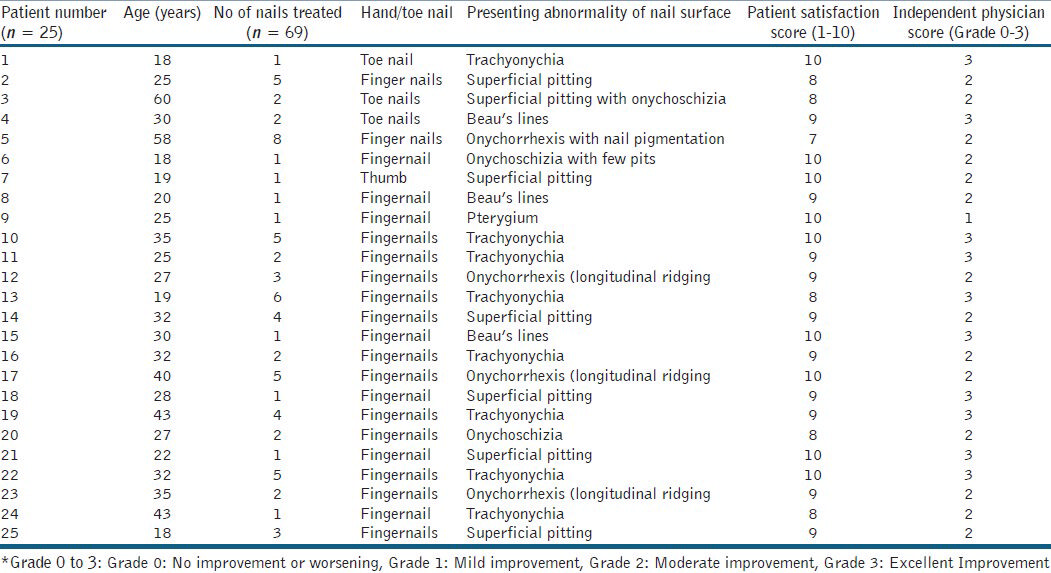
A total of 25 patients (23 females and 2 males) in the age range of 18-60 years were included in the study (average age 30.44 ± 11.39 years). Their details are summarised in Table 1. The degree of involvement varied from single nail involvement to ten nail involvement. The total numbers of nails treated were 69 (average of 2.76 nails treated per patient; range 1-8 nails). Majority of the patients had involvement of finger nails, with only three patients seeking treatment for their toe nails. Morphological presentations included were trachyonychia or sand papered nails (8 cases); superficial nail pitting (6 cases) [Figure 3]; onychorrhexis (4 cases) [Figure 4]; superficial pitting with onychoschizia (3 cases) [Figure 5]; Beau's lines (3 cases) [Figure 6] and pterygium (1 case).

- Nail pitting in a case with alopecia areata improved in appearance after application of gel nail.

- Onychorrhexis of unknown aetiology showing excellent improvement. Patient satisfaction score was 10.

- A case of psoriasis with onychoschizia and nail pitting in an isolated nail.

- Beau's lines in a 19-year-old girl who was very disturbed by their appearance. Marked improvement seen with gel nail application.
Post-procedure, the average patient satisfaction score was 9.08 ± 0.86 (range 7-10). The global assessment done by two independent physicians on the basis of serial photographs showed excellent improvement in 40% cases (n = 10); good improvement in 56% cases (n = 14) and mild improvement in the single case of pterygium treated.
DISCUSSION
Nails serve important functions in humans. They have a significant role to play in ensuring protection of digital tip; improving fine touch; serving as defence; in addition to being important for the patient's cosmesis. The importance of good looking nails for an individual's self-esteem is known to one and all. Many recent studies have shown that nail diseases significantly affect the employability, self-esteem and the overall quality of life (QoL) of the patients.[456] Hence, the importance of treating the patient's nail condition cannot be ignored.
Treatment options depend on the aetiological factors for nail disease and include topical corticosteroids, intralesional (intramatricial therapies) and, if extensive, then systemic drugs. Grover et al. evaluated the efficacy of intramatricial triamcinolone injections in various acquired nail dystrophies. Although the treatment efficacy was good, significant side effects included pain, subungual haematoma formation, proximal nail fold hypopigmentation and atrophy.[7] The use of systemic cytotoxic drugs with their attendant side effects may not be justified for limited and superficial nail involvement. In such a case scenario, denying any kind of treatment to the patient is also not very acceptable. Additionally, not much can be done for end stage nail conditions like a pterygium. However, the use of gel nails can offer cosmetically appreciable improvement, hence we evaluated this modality.
Artificial nails have been widely used in the cosmetic industry;[123] however, in the medical field, anecdotal reports exist of their usefulness in cases with nail biting (onychotillomania), brittle nails or camouflaging small or disfigured nails. Artificial nails are mostly done at nail salons and not at a dermatologist's office. Gel nails have been shunned by dermatologists because of the reported side effects, including dryness of nails, contact allergic dermatitis of surrounding skin, paronychia, brittleness, masking of underlying nail disorders and reported cases of non-melanoma skin cancer possibly associated with their use.[891011] On analysis, however, it can be seen that most of these side effects are technique dependent. A judicious use of these commonly available nail products proves to be very effective in management of this trivial yet troublesome issue.
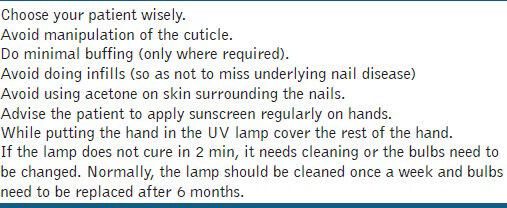
To avoid any untoward outcome, we incorporated some crucial precautions [Table 2]. We avoided manipulating the cuticle at all, thus decreasing the chances of paronychia. Buffing of nail plate was done only where required and that too to a minimal extent, hence avoiding thinning of the nail plate. We used a single layer of gel nail and hence, subsequent removal was also very simple. In normal salon practice, the nails are removed by dipping hands in pure acetone for 30 min, which is mostly responsible for the acquired brittleness of nails and contact dermatitis of surrounding skin. Also, the standard time of exposure in the UV lamp was maintained at 2 min (roughly equivalent to an extra sun exposure of 26 s/day for 5 days/week).[12] We also advised the patient to apply sunscreen on hands and covered rest of the hand with white towel to avoid photodamage, whatsoever minimal, to hand skin. Salons are known to resort to 2-3 cycles of UV curing. We used only single cycle as we applied a single coat. For all the patients, complete gel nail were removed after 1 month and the patient was again followed-up at 1 week. This helped us re-assess the condition of the nail and the surrounding skin before reapplying gel nail, if requested by the patient. Also the risk that any underlying nail disease would be camouflaged was eliminated.
It was also observed that the use of gel nails on cosmetically disfigured nails could be more rewarding as compared with their use over apparently normal nails. This is because the rate of growth of dermatologically compromised nails is relatively slower; hence, gel nail lasts longer (i.e. around 4 weeks as opposed to 2 weeks in normal nails). Additionally, the nail plate in most of these cases is already not smooth; hence, minimal, if any, buffing is required. Last, but not the least, it is a lot easier to manage patient's expectation as even mild improvement in their nail condition is very gratifying to them. The psychological impact of nail diseases is profound due to the high visibility of the disfigurement, especially the fingernails.[13] Studies evaluating the QoL in patients with psoriasis have shown that majority of the patients are bothered about the cosmetic appearance of the nails, of these only around 35% seek treatment of which only about 35% are happy with the results.[14] In spite of the vast number of treatment options currently available, there is still a need for more options. As dermatologist, it becomes our duty to offer a solution for all nail-related issues of our patients, which could be as trivial as mild pitting, longitudinal ridging or brittleness of nails. A detailed knowledge of the available cosmetic treatments for nails could provide us with an option for our patients where we have no satisfactory medical solution is available or palliative treatment till the time medical effect becomes evident.
Although, side effects have been attributed to gel nails[891516] the exact figures are not forthcoming. Millions of gel nails are being done every single day and in proportion to that, the number of side effects reported is miniscule. In expert hands, further care can be taken to minimise any possible complications in dermatologically compromised nails. A guided use of these prostheses could significantly improve the satisfaction and QoL of our nail patients, where we may not have much else to do.
CONCLUSIONS
It can be concluded that gel nails if used wisely, by specialists, could prove to be a very valuable tool in the dermatologist's armamentarium, to improve cosmesis and increase satisfaction. They can be good for camouflaging the superficial nail plate abnormalities like superficial pitting, trachyonychia, onychoschizia, etc., where other treatments may not be useful or required. A proper attention and few modifications to the application procedure can prevent the adverse effects reported with this procedure. Further studies with larger number of patients are required to assess the impact these prostheses can have on our nail patients.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Quality of life in toenail onychomycosis. In: Preedy VR, Watson RR, eds. Handbook of disease burdens and quality of life measures. New York: Springer; 2010. p. :3837-50.
- [Google Scholar]
- Psoriatic nail disease: Quality of life and treatment. J Cutan Med Surg. 2009;13:S102-6.
- [Google Scholar]
- Dermatology Life Quality Index (DLQI) - a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-6.
- [Google Scholar]
- Efficacy of triamcinolone acetonide in various acquired nail dystrophies. J Dermatol. 2005;32:963-8.
- [Google Scholar]
- Adverse contact reaction to sculptured acrylic nails: 4 case reports and a literature review. Contact Dermatitis. 1995;33:381-5.
- [Google Scholar]
- Adverse nail reactions and paresthesias from “photoblonded acrylate ‘sculptured’ nails”. Cutis. 1990;45:293-4.
- [Google Scholar]
- Permanent paresthesia to sculptured nails. A distressing problem Dermatol Clin. 1990;8:139-41.
- [Google Scholar]
- Occurrence of nonmelanoma skin cancers on the hands after UV nail light exposure. Arch Dermatol. 2009;145:447-9.
- [Google Scholar]
- Risk of skin cancer associated with the use of UV nail lamp. J Invest Dermatol. 2013;133:1097-9.
- [Google Scholar]
- NailQoL: A quality-of-life instrument for onychomycosis. Int J Dermatol. 2007;46:1279-86.
- [Google Scholar]
- Development and validation of nail psoriasis quality of life scale (NPQ10) J Eur Acad Dermatol Venereol. 2010;24:22-7.
- [Google Scholar]
- Allergic contact dermatitis to artificial finger nails prepared from UV light cured acrylates. J Am Acad Dermatol. 1996;35:377-80.
- [Google Scholar]






