Translate this page into:
Superficial Large Basal Cell Carcinoma Over Face, Reconstructed by V-Y Plasty
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Basal cell carcinoma (BCC) is derived from the non-keratinizing cells originating from the basal layer of the epidermis. BCC generally has a clinical course characterized by slow growth, minimal soft-tissue invasiveness, and a high cure rate. Occasionally, however, BCC behaves aggressively with deep invasion, recurrence, and potential regional and distant metastasis. Several factors, including tumour size, duration, histology, and perineural spread, have been postulated as markers of the aggressive BCC phenotype. Types of BCC are of nodular, pigmented, superficial, morpheaform and fibroepithelioma of Pinkus. Superficial spreading BCC (sBCC) accounts for 16-25% of all BCCs. Superficial BCC commonly occur over limbs and trunk and rarely do they over the face.[1] Surgical techniques such as standard excision, Mohs micrographic surgery, curettage with electrodessication and cryotherapy are employed to prevent recurrences.[2] Herein, we report a case of large sBCC over the face for which reconstructive V-Y plasty was carried out at our centre.
A 66-year-old woman, presented with a single, dark ulcerated plaque over the left temple since 2 years with a history of blood discharge from the lesion since a year. There were no similar complaints in the family. Dermatological examination revealed a large 5 cm × 6 cm single, hyperpigmented, ulcerated plaque with undulating margins and rolled out edges [Figure 1]. Incisional biopsy taken from the lesion revealed small geographic lesion composed of small round, basaloid cells proliferation. The cells showed mild anisonucleosis, atypical mitosis and peripheral palisading consistent with sBCC [Figure 2]. The plaque was subjected to wide local excision with 3 mm margin followed by reconstructive V-Y plasty. The V-Y flap is designed inferiorly over the cheek and one superiorly in the temple area. Inferior flap is mobilised, lower pedicle raised while upper one is brought distally and closed [Figures 3 and 4]. Histopathology of the excised specimen was consistent with sBCC without perineural involvement.

- A large 5 cm × 6 cm single, hyperpigmented, ulcerated plaque with undulating margins and rolled out edges
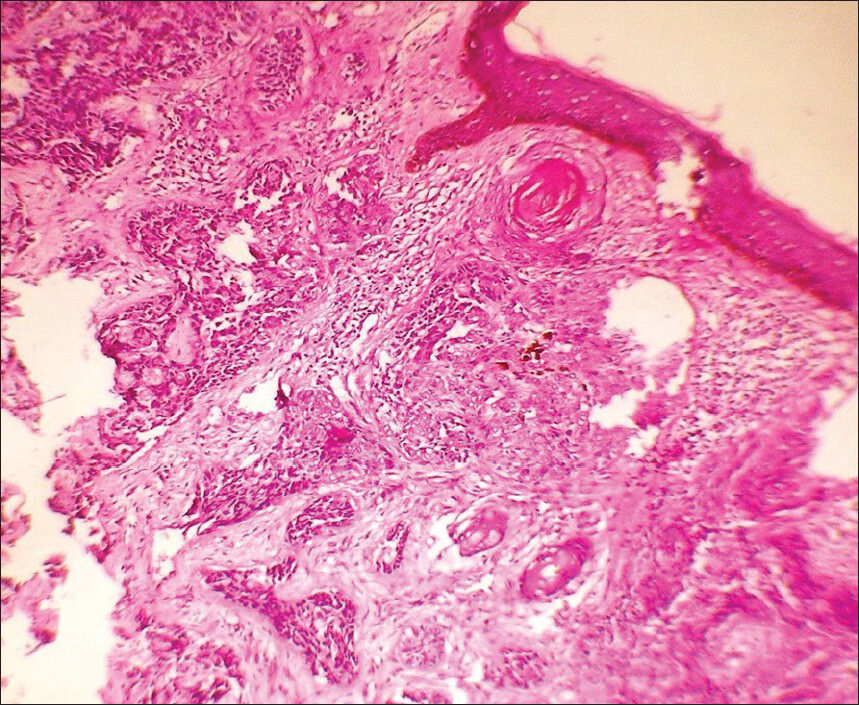
- Small geographic lesion composed of small round, basaloid cells proliferation
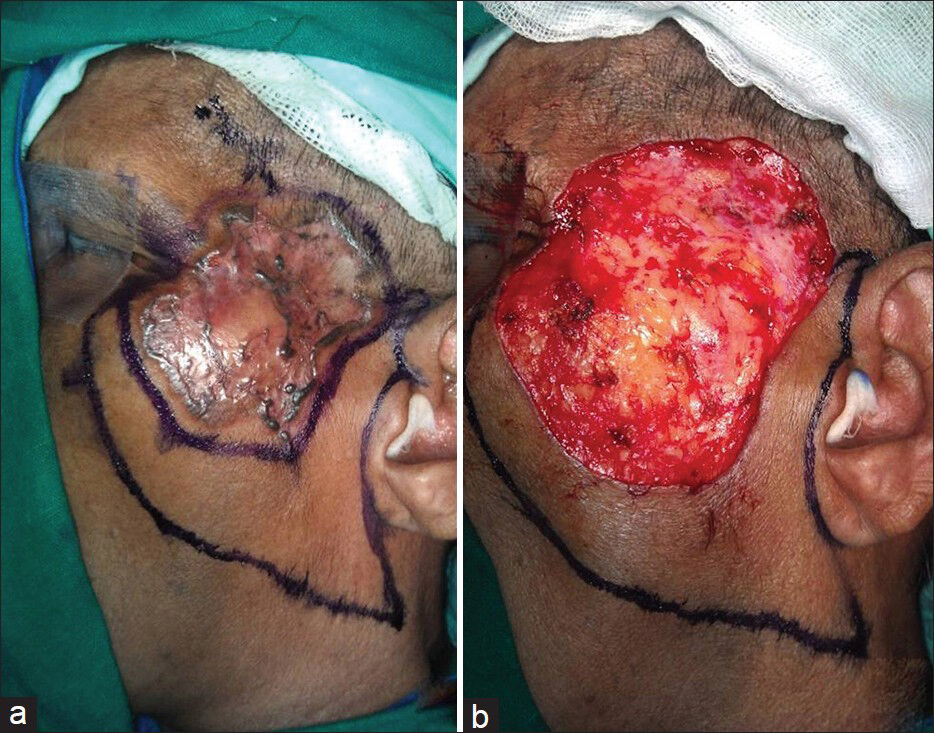
- (a) Wide local excision, (b) Excision of lesion with margins and outline of V-Y advancement flap

- (a) Closure of V-Y advancement flap, (b) Post-operative over 1 week
BCC is the most common skin cancer in white individuals. Similar to other non-melanoma skin cancers, its incidence is rising. Recently, the incidence of BCC has been increasing among Asians, and the overall number of BCC cases has been growing rapidly. The nodular, superficial spreading and infiltrating variants are the three most commonly encountered types of BCC in descending order of prevalence.[3] The clinical characteristics of BCC appear commonly on the head and neck areas, and the most common subtype of BCC is the histopathologically distinct nodular type. sBCC primarily develops on the trunk, in contrast to the other subtypes. It has been suggested that sBCC is a separate group within the clinical entity of BCC, of which intermittent sun exposure may be an important aetiology.
BCC on the face may have a higher degree of subclinical spread than tumours arising elsewhere. In general, the cosmetic outcome for standard surgical excision is felt to be good, but having to remove large lesions with adequate excision margins can be disfiguring as a result of loss of tissue, grafting and subsequent scarring.[4] Special attention must be paid to the location of the BCC on the face as there are many areas of functional and cosmetic importance for example the periocular, perioral, and perinasal areas. In general, standard surgical excision is considered a good treatment option for all BCCs arising on the face with 5-year recurrence rates of anything up to 10% providing adequate margins are taken. A 3-mm margin is recommended for standard surgical excision. While it would seem sensible to take larger margins at the sites where subclinical spread is known to be more extensive, these sites are all of great cosmetic and functional importance and therefore striking the correct balance is necessary.[5] In our case wide local excision with 3 mm margin, was carried out to prevent recurrences. V-Y advancement flap was designed as these flaps have an excellent blood supply from subcutaneous tissue and ideal for use on the face since secondary revisions are rarely required. They are superior to rotation flaps, which may leave dog ears, skin grafts, which are depressed and shiny and primary closure where tension is present. The only complications are loss of edge of flap from too much tension and hair loss over that area.[6]
Herein, we report a case of sBCC occurring on face, an unusual site to occur and reconstructive surgery performed to restore the defect after wide local excision.
REFERENCES
- Management of superficial basal cell carcinoma: Focus on imiquimod. Clin Cosmet Investig Dermatol. 2009;2:65-75.
- [Google Scholar]
- CASE REPORT superficial spreading basal cell carcinoma of the face: A surgical challenge. Eplasty. 2010;10:e46.
- [Google Scholar]
- Large superficial basal cell carcinoma arising in the scalp. Ann Dermatol. 2011;23:S96-9.
- [Google Scholar]
- Grabb's encyclopedia of flaps head and neck. (3rd ed). USA: Lippincott Williams and Wilkins, a Wolter Kluwer business; 2009. p. :263-5.
- [Google Scholar]





