Translate this page into:
Primary Bilateral Extramammary Paget's Disease of the Axillae: Another Case of this Strange Disease
Address for correspondence: Dr. Giuseppe Del Torto, Division of Plastic, Reconstructive and Aesthetic Surgery, University of the Study of Perugia, via R. Leoncavallo 806132 Perugia, Italy. E-mail: g.deltorto@yahoo.it
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary extramammary Paget's disease of the axilla is a rare variant with the capability of mimicking other more common conditions. We present a case of a 65-year-old woman with inflammatory skin lesions of both axillae clinically unresponsive to long-term conventional topical therapy. We decided to excise and reconstruct the resulting soft tissue defect of the major lesion by using a thoraco-dorsal artery perforator-based Limberg's flap. The histopathological examination showed intracellular mucin, signet cells, and glandular structures, the typical pattern of the EMPD. This was a very interesting case of a per se rare condition.
Keywords
Axillary Paget's disease
bilateral axillary Paget's disease
extramammary Paget's
INTRODUCTION
Mammary Paget's disease (PD) of the nipple was first described by Sir James Paget in 1874. Extramammary PD (EMPD) was first recognised and reported as a distinct clinical entity by Radcliffe Crocker in 1889.[1] EMPD is morphologically and histologically identical to mammary PD of the nipple, the primary difference being the anatomical location. Unlike the mammary Paget's disease, the extramammary type is less well known and much rarer, representing just 6.5% of all Paget's disease and is more common among women over 50-years of age.
Approximately 25% of EMPD (range 9-32%) are associated with an underlying in situ or invasive neoplasm. In all patients, the neoplasm most likely to be associated with EMPD is an adnexal apocrine carcinoma.[2]
This report describes a very rare case of primary bilateral axillary EMPD treated by wide local excision. The reconstruction of the resulting soft tissue defect was successfully achieved by using a thoraco-dorsal artery perforator-based Limberg's flap.
CASE REPORT
A 65-year-old woman was referred to the Plastic and Reconstructive Department of the University of Perugia in May 2012 for the management of an inflammatory skin disease of both axillae clinically unresponsive to long-term conventional topical therapy. Symptoms included pruritus, burning paraesthesia and pain.
The patient was initially treated with a combination of topical corticosteroids and antibiotics for two weeks without improvement. This was followed by topical imiquimod 5% cream for about 4 weeks with out benefit.
On physical examination, the lesion in the left axilla measured 4 × 4 cm and the other side one was much bigger, measuring 12 × 10 cm. Both of them appeared as pink erythematous patches with irregular borders and with localised desquamated erosions together with leukokeratotic foci [Figure 1].

- Clinical presentation of the well-demarked pink erythematous patch in the left axilla
Bilateral breast examination revealed normal breast consistency without any nodules, nipple modification, excoriation or discharge; mammograms showed a normal breast parenchyma confirming the nodules absence. An 18-FDG Pet-Tc was also performed without showing any internal malignancy.
The patient underwent operation under general anaesthesia: in the right side we were able to repair the secondary skin defect by an intradermal suture, due to its moderate dimension. For the left lesion the patient was positioned on the contralateral side; left arm was abducted in 90°. After excising the skin lesion with an apparent tumour-free margin of 2 cm, we provided the skin defect reconstruction using a thoraco-dorsal perforator flap, according to Limberg's design [Figures 2 and 3].

- Pre-operative planning of the Limber's flap
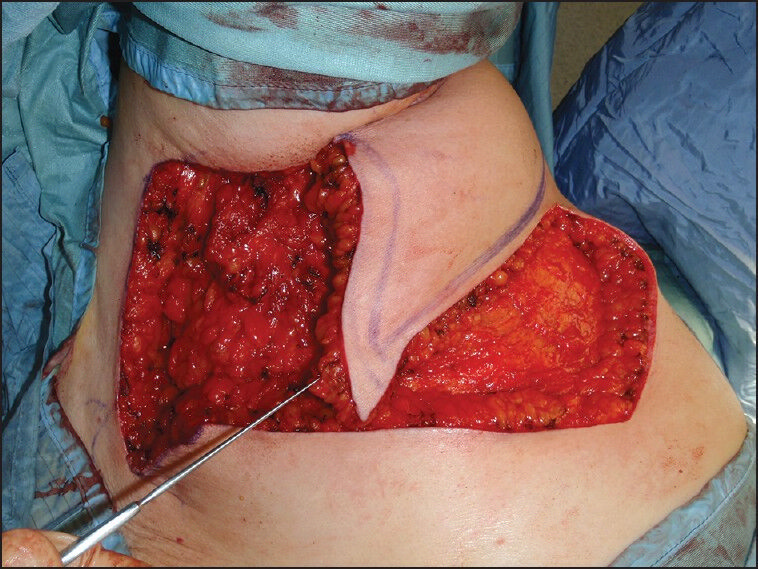
- Intra-operatory view showing the resulting wide skin defect and the arch of rotation of the Limberg's flap previously designed
During the operation we removed two lymph nodes appearing lightly enlarged and of increased consistency: Histopathological examination revealed no tumour invasion but just signs of reactive histiocytosis secondary to sovra-infections of the lesion.
The excision specimen of the cutaneous lesion was sent for histopathological examination: There were nests of atypical cells with melanin pigmentation within their cytoplasm showing pagetoid involvement of the epidermis together with cells with abundant basophilic cytoplasm, with signet ring forms. These cells stained positively with Alcian Blue and PAS-diastase stains, confirming the presence of mucin. On immunohistochemistry, the pagetoid cells stained strongly positively for cytokeratin 7 (CK7), cytokeratin 20 (CK20), carcinoembryonic antigen (CEA), EMA and CGDFP-15. These cells also stained positively for melanocytic markers S-100, Melan-A, condition quite rare with very few cases described in the literature.
The presence of positivity for CK 7 and negativity for CK 5/6 (an excellent marker of squamous differentiation, characteristically expressed strongly and diffusely by either squamous carcinomas or benign squamous epithelium) allowed us to rule out, together with the specimen histopathological features (intracellular mucin, signet cells and glandular structures), the hypothesis of Bowen's disease.
The acinar formation, the intracellular mucin and the positivity of the anti-EMA and anti-CEA antibodies (usually not labelled by melanocytes) were strongly indicative for Paget's disease rather than melanoma.[3]
The flap survived completely preserving a complete range of motion of the upper limb and the aesthetic result after 24 months was good. No further adjuvant treatments were given after the excision [Figure 4].

- View of the flap 5 weeks after the operation. It survived totally, with complete wound healing. Both functional and aesthetic results are satisfactory
The perineal area was also evaluated but was free from any pathological signs such as redness, swelling, dryness, and the patient denied any discomfort or itching in that area.
The patient is currently alive without any sign/symptoms of recurrence after 15 months: she continues to be under follow-up.
DISCUSSION
Axillary location of EMPD is very rare. A review of the literature revealed only 23 cases reported so far, the majority in Japanese population. Out of these, 10 cases had isolated axillary involvement while 13 demonstrated simultaneous axillary and genital disease (so called triple EMPD). Presence of an underlying carcinoma in axillary EMPD has been reported in eight of the 23 cases (35%).[4] Bilateral axillary presentation of primary EMPD is extremely rare and infrequent.
The genesis of the Paget's cell is controversial. There are four different theories that explain the four different patterns of presentation. One theory proposes that stem cells present in the basal cell layer of the epidermis change into Paget cells as a result of faulty development of these cells in their attempt to mature into an apocrine structure. The second theory hypothesises that epidermal Paget cells originate from cells that have migrated from an adjacent malignant region–either an adnexal sweat gland or anorectal mucosa or from another contiguous structure. A third theory suggests that Paget's cells may represent a form of metastasis, but not in extramammary Paget's disease.[5] Some authors suggest that P53 may play a role in the progression of vulvar Paget's disease and may be a terminal event in some cases, especially those associated with invasive disease. A novel tumour marker RCAS1 has been identified in cases of extramammary Paget's disease and has the potential of becoming a biomarker for monitoring therapeutic efficacy.[6]
The contemporary expression of CK20, S100 and melan-A in the tumour cells makes this case interesting. These atypical findings may be compatible with the presence of a pigmented area and may be referred as a "locally" pigmented Extramammary Paget's disease.
Patients commonly present with hyper- or hypopigmented pruritic patches or plaques with a non-specific clinical appearance, thus leading to a significant delay between initial presentation and diagnosis. They may be associated with a palpable mass in the subcutaneous tissue but are often limited to the skin.[3]
Differential diagnosis includes malignant melanoma, Bowen's disease, mycosis fungoides and Langherans cells hystiocytosis.[4]
Prognosis of the axillary Paget's disease is better than other localisations because of the clear anatomy of the axillary region and the possibility to perform a wide excision thanks to the great numbers of reconstructive approaches using either local fasciocutaneous or muscolocutaneous flaps. One study showed a mortality of 18% for patients without associated carcinoma and 46% for those with underlying carcinoma.[7] A long-term follow-up is strongly recommended.
The perineal examination was done in order to evaluate the, although very rare, co-existence of a perineal EMPD in what is so called Triple or Quadruple EMPD. We decided not to perform any perianal skin biopsy motivated by the high rarity of this co-existence, counting less than 30 cases described in the literature and the majority among Asian men[8], the absolute absence of any signs and symptoms.
Although the gold standard of treatment of EMPD is Mohs micrographic surgery (MMS) providing margin control in tumour known to have diffuse spread beyond the clinically apparent margins, in cases in which MMS is not available, a wide local excision with margins of 1-5 cm have been quoted to have excellent results.[9]
CONCLUSION
The management of primary extramammary Paget's disease of the axilla was based on a locally wide excision but now the treatment ofchoice for EMPD is Mohs micrographic surgery (MMS) providing margin control. The role of sentinel lymph node evaluation is still unclear and the role of adjuvant therapy is controversial. However, because of the multifocal nature of this disease, recurrence rates are quite high.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- On disease of the mammary areola preceding cancer of the mammary gland. St. Barth Hospital Rep. 1874;10:87-9.
- [Google Scholar]
- Immunohistology is valuable in distinguishing between Paget's disease, Bowen's disease and superficial spreading malignant melanoma. Histopathology. 1990;16:583-8.
- [Google Scholar]
- Extramammary Paget's disease of the axilla: An anusual case. Breast J. 2007;13:291-3.
- [Google Scholar]
- The role of HER-2/neu oncogene and vimentin filaments in the production of the Paget's phenotype. Breast J. 2003;9:485-90.
- [Google Scholar]
- A novel tumor marker RCAS1 in case of extramammary Paget's disease. Clin Exp Dermatol. 2003;28:211-3.
- [Google Scholar]
- Extramammary Paget's disease of the unilateral axilla: A review of seven cases in a 20-year experience. Int J Dermatol. 2011;50:157-60.
- [Google Scholar]
- Ectopic extramammary Paget's disease: Case report and literature review. Acta Derm Venereol. 2010;90:502-5.
- [Google Scholar]
- Extramammary Paget's disease of the genitalia with clinically clear margins can be adequately resected with 1 cm margin. Eur J Dermatol. 2005;15:168-70.
- [Google Scholar]






