Translate this page into:
A Retrospective Study of Marjolin's Ulcer Over an Eleven Year Period
Address for correspondence: Dr. Vasu Reddy Challa, Department of Surgical Oncology, Kidwai Memorial Institute of Oncology, Bengaluru - 560 029, Karnataka, India. E-mail: vasureddyc@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Marjolin's ulcer is a rare aggressive cutaneous malignancy occurring in previously occurred wounds. The most common aetiology is a burn wound involving extremities and squamous cell carcinoma is the most common variant.
Materials and Methods:
A retrospective analyses of medical records of patients treated in a single unit with a diagnosis of Marjolin's ulcer was performed.
Results:
During the study period, 14 patients were treated. Four patients had lymph node metastases and one had pulmonary metastases at the time of presentation. Seven patients underwent wide excision with reconstruction and seven underwent amputation or disarticulation because of advanced malignancy. During the follow up two patients developed local recurrence and one developed pulmonary metastases. Both the patients with pulmonary metastases had Marjolin's ulcer of trunk.
Conclusion:
Marjolin's ulcer occurs more commonly in the extremities. Distant metastases occur commonly in patients with ulcers on the of trunk.
Keywords
Chronic ulcers
cutaneous malignancy
Marjolin's ulcer
squamous cell carcinoma
INTRODUCTION
Marjolin's ulcer is a rare cutaneous malignancy. It was first described in 1828 by French surgeon, Jean Nicolas Marjolin.[123] It was recognised as malignancy by Dupuytren and the term ‘Marjolin's ulcer’ was coined by Da Costa in 1903 for malignancies arising from burn wounds.[45] Various hypotheses have been put forth for the pathogenesis in the development of malignancy like repeated reparative process, promoter and carcinogen theory, traumatic implantation of epithelial elements theory, chronic irritation theory.[6] The latency period from the initial injury to the development malignancy varied in various studies with occurrence even after 50 years. Marjolin's ulcer in sub-Saharan Africans occurred earlier and in younger patients.[7] Most common type of malignancy occurring in these wounds is squamous cell carcinoma (SCC) followed by basal cell carcinoma (BCC) and sarcomas. Extremities are the most commonly involved sites followed by head and neck region and trunk.[4]
In a search in Pubmed on 20 December 2013, only 174 (most of them are case reports) published related articles were found implicating the rarity of the clinical condition. Here we would like to present our experience on the clinicopathological features, treatment provided and survival with a brief review of literature on this rare entity.
MATERIALS AND METHODS
We retrospectively analysed medical records of patients who were diagnosed as Marjolin's ulcer from the period Jan 2002-Dec 2012 operated in a single unit in a tertiary care cancer centre. The demographic profile, clinical presentation, treatment provided and survival were analysed.
RESULTS
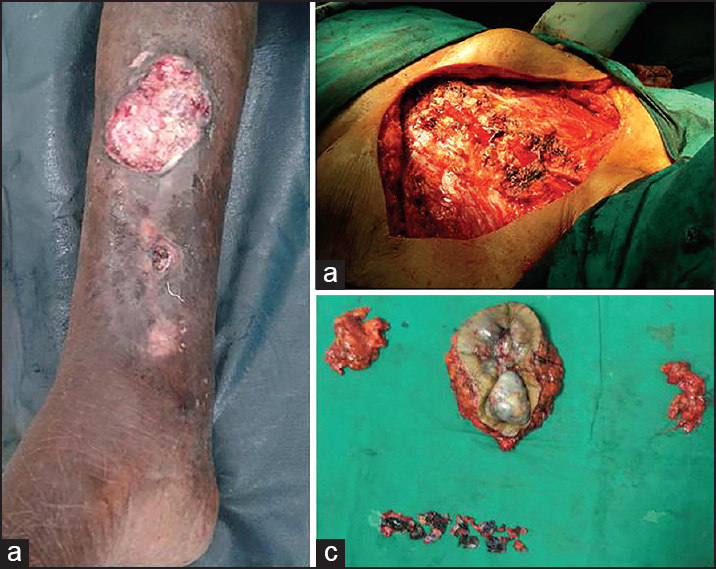
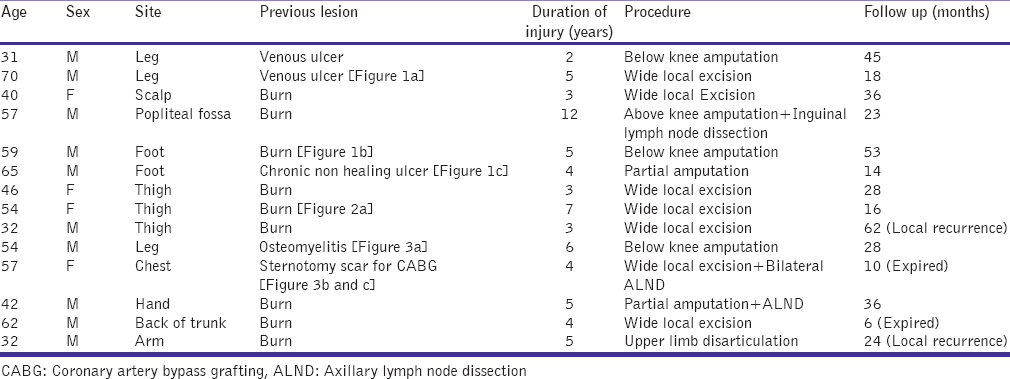
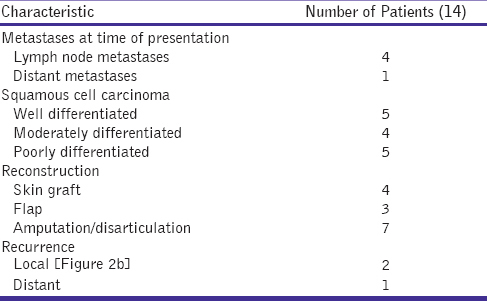
Fourteen patients with Marjolin's ulcer were treated in the above-mentioned study period of which 10 were males and 4 were females. The mean age of presentation was 50.0 ± 4.2 years (range 32-70 years). The duration from the time of insult to the development of cancer varied from 2 to 12 years (mean 4.8 ± 2.3 years). The clinical profile of the patients and the initial insult which had led to the development of cancer were described in Table 1. The lower limb was the most common site of Marjolin's ulcer. Of 14 cases, 2 cases of Marjolin's ulcer developed in chronic venous ulcer [Figures 1a and b], one case in a patient after chronic trauma [Figures 1c], 9 cases after burn injury [Figures 2a and b], 1 case in a chronic osteomyelits scar [Figure 3a] and one case over a scar following coronary artery bypass grafting [Figure 3b]. She developed an ulceronodular growth over the CABG scar which was excised along with the outer table of sternum [Figure 3b and c]. Bilateral axillary lymph node dissection was performed with pectoralis major muscular flap to cover the sternum. The treatment given is described in Table 1.

- (a and b) Photograph showing an ulceroproliferative growth from a chronic venous ulcer. (c) A patient with a chronic traumatic wound who developed Marjolin's ulcer

- (a) Marjolin's ulcer of thigh in a 54 year old female developing 7 years after a burn injury. (b) A recurrent Marjolin's ulcer of left thigh occurring after wide excision and split skin thickness grafting
- (a) Marjolin's ulcer occurring in a 55-year-old male which occurred in a patient with chronic osteomyelitis. (b and c) Marjolin's ulcer in a 57-year-old female occurring in a post CABG (coronary artery bypass grafting) scar
Four patients had lymph node metastases at the time of presentation and they underwent lymph node dissection [Table 2]. One patient with Marjolin's ulcer over the back had lung metastases at the time of presentation but a palliative excision was performed because of bleeding. Wide excision with split skin thickness graft or flap reconstruction was performed in seven patients and seven patients underwent amputation or disarticulation. The mean duration of follow up was 28.5 ± 15.7 months (Range: 6-62 months). During the follow-up period two patients developed local recurrence. One case had recurrence in the stump after an upper limb disarticulation and the other over the thigh after wide excision and SSTG [Figure 2b]. The case with post CABG scar Marjolin's developed pulmonary metastases during the follow-up period after 7 months. Of the two patients with pulmonary metastases, one patient died within 6 months of treatment and the other patient expired 10 months after treatment.
DISCUSSION
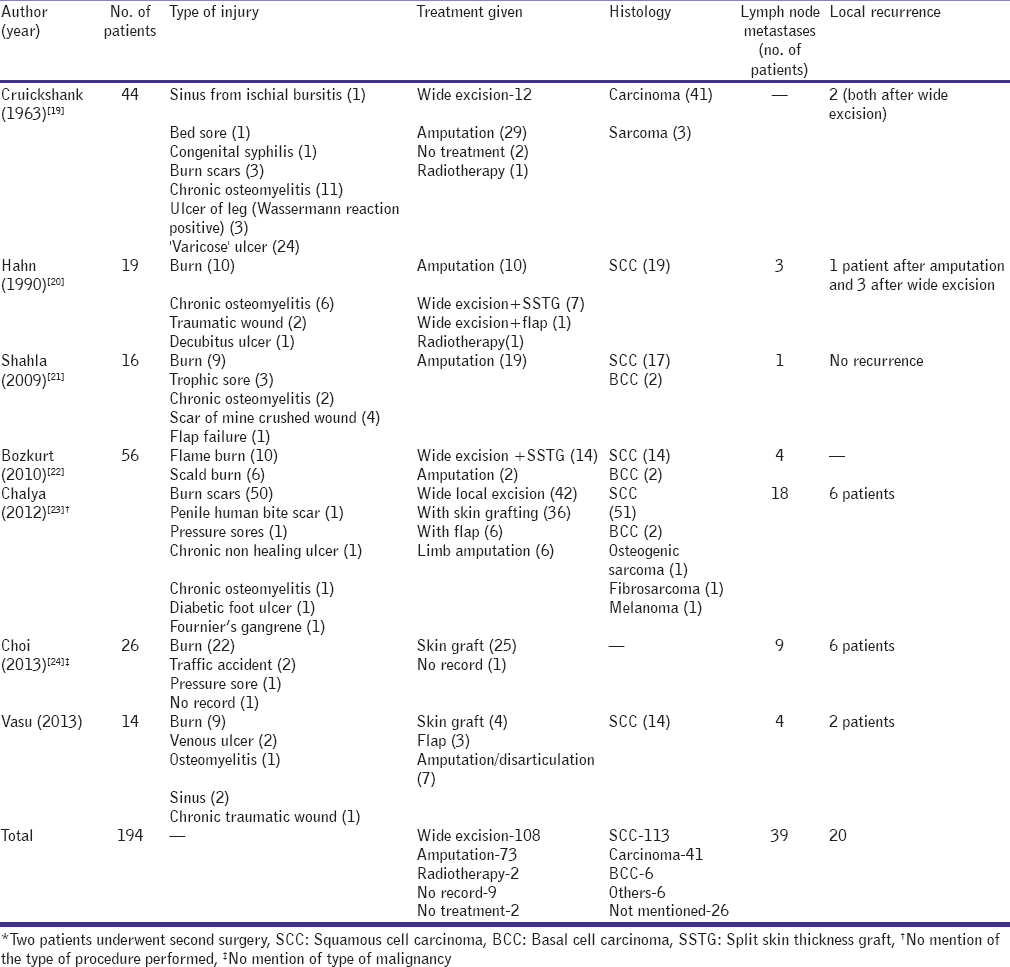
Marjolin's ulcer is a rare type of skin malignancy associated with previous insult. There are various terms used to describe these malignancies like ‘Kangri’ cancer in Kashmir, India, where hot earthen oven over chestwall leads to repeated burn injuries which later progress to cancer. Similarly ‘Kairo burn cancer’ in Japan due to tin ovens worn over abdomen; ‘Kang Ulcer’ in China where due to warming bed with heat leads to ulcers over the buttocks.[8] Various theories had been proposed in the pathogenesis of this malignancy but none of them alone could explain all conditions. Toxin theory which proposes that chronic inflammatory process leading to tissue damage produces toxins which may be carcinogenic.[6] The lower limb was the most common site of Marjolin's ulcer and previous history of burn was the most common predisposing factor. The other various theories proposed where cocarcinogen (Friedwald and Rouse) theory, chronic irritation (Virchows) theory, implantation (Ribet's) theory, immunologically privileged site (Castillo and Goldsmith) theory, toxin (Treves and Pack) theory, environmental and genetic theories.[69] Recent studies had shown association of Marjolin's with HLA DR4 and mutations of Fas and p53 genes.[710111213] Studies had shown decreased reduction or absent Langerhan cells in burn wounds which lead to decreased immunosurveillance.[1415] The development of Marjolin's ulcer can be acute or chronic. Acute Marjolin's occurs within 1 or 2 years which can be best explained by the environmental and genetic mechanisms associated with this individuals.[1617] Earlier studies had venous ulcer and chronic osteomyelitis as a predominant cause for development of Marjolin's ulcer but with antibiotics and better management of varicose veins the incidence of Marjolin's in these patients decreased and burn injury remain as the predominant cause.[18] The various studies describing the type of injury, histology, and other features are described in Table 3. Cruickshank et al.[19] had varicose veins as the predominant cause of Marjolin's ulcer, whereas latest studies show burn scars as the main cause. Various methods to prevent Marjolin's ulcer include early skin grafting for deep burn wounds and excision and grafting for unstable scars which are predisposed to repeated trauma like scars over the joints or mobile areas. Also scars which are thick and hypopigmented need to be excised and grafted. Scars over the scalp should be protected from sunlight by using wigs or clothing.[9]
The risk of transformation of chronic wound to malignancy is 0.1-2.5%.[25] The various signs which indicate malignant transformation is nodule formation, induration and ulceration. Other symptoms and signs which should be looked for are ulceration persisting for more than months with foul smelling discharge, bleeding on touch, exuberant granulation with everted tissue, excessive crusting, rapid increase in size, spread of ulcer to normal appearing skin and new onset of pain.[9] Aggressive treatment with wide excision and reconstruction is the main mode of treatment. Ulcer needs to be excised with 2-5 cm margin or should be considered for Mohs micrographic surgery in areas like face and recurrent lesions.[26] Amputation is needed to be considered for patients where wide excision is not possible due to advanced stage. Reconstruction with skin graft or flap is decided by the site of lesion though most studies advocate skin graft for better follow up to detect recurrence. Lymph node dissection needs to be considered when there are suspicious or involved lymph nodes.
Grossly the appearance of the lesion can be flat, infiltrative of exophytic proliferative growth.[20] The risk of recurrence in different studies ranged from 20% to 50% and the 5 year survival rate was 40-60%.[1927] Choi et al. in their analysis found disturbed wound healing as a risk factor for recurrence.[22] In the present study, two patients had distant metastases one was a case of burn scar over the trunk with pulmonary metastases at the time of presentation and the other a case of post CABG scar Marjolin's who developed pulmonary metastases during follow up. In both the cases the site of lesion was trunk which was considered as a poor prognostic factor. Prognostic factors associated with better survival are latency to malignancy less than 5 years, site of lesion head, neck, upper extremities; cause-burns, chronic osteomyelitis; tumour size less than 2 cm; tumour type exophytic and less than 4 mm thickness.[6]
CONCLUSION
Marjolin's ulcers are rare malignancies with squamous cell carcinoma as the most common histological variant. Burn injury is the most common predisposing factor. Ulcers on the trunk were associated with poor prognosis.
Source of Support: Nil.
Conflict of Interest: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
REFERENCES
- III. Carcinomatous changes in an area of chronic ulceration, or Marjolin's ulcer. Ann Surg. 1903;37:495-502.
- [Google Scholar]
- Marjolin's ulcers: Theories, prognostic factors and their peculiarities in spina bifida patients. World J Surg Oncol. 2010;8:108.
- [Google Scholar]
- Somatic mutations of Fas (Apo-1/CD95) gene in cutaneous squamous cell carcinoma arising from a burn scar. J Invest Dermatol. 2000;114:122-6.
- [Google Scholar]
- A comprehensive review on marjolin's ulcers: Diagnosis and treatment. J Am Col Certif Wound Spec. 2011;3:60-4.
- [Google Scholar]
- Genetic analysis of cutaneous squamous cell carcinomas arising from different areas. Pathol Int. 2003;53:602-7.
- [Google Scholar]
- HLA DR4 is associated with the development of multiple basal cell carcinomas and malignant melanoma. Dermatolgy. 1993;187:16-8.
- [Google Scholar]
- Deletion of the p53 gene in a patient with aggressive burn scar carcinoma. J Trauma. 1997;42:104-7.
- [Google Scholar]
- Marjolin's ulcer: An immunologically privileged tumor? Plast Reconstr Surg. 1975;57:66-9.
- [Google Scholar]
- Is surgery an effective and adequate treatment in advanced Marjolin's ulcer? Burns. 2005;31:421-31.
- [Google Scholar]
- Malignancy and chronic wounds: Marjolin's Ulcer. J Burn Care Rehabil. 1991;12:218-23.
- [Google Scholar]
- An overview of heel Marjolin's ulcers in the orthopedic department of Urmia University of Medical Sciences. Arch Iran Med. 2009;12:405-8.
- [Google Scholar]
- Current concepts in the management of Marjolin's ulcers: Outcomes from a standardized treatment protocol in 16 cases. J Burn Care Res. 2010;31:776-80.
- [Google Scholar]
- Marjolin's ulcers at a university teaching hospital in Northwestern Tanzania: A retrospective review of 56 cases. World J Surg Oncol. 2012;10:38.
- [Google Scholar]
- Impact of disturbed wound healing after surgery on the prognosis of Marjolin's ulcer. Arch Plast Surg. 2013;40:198-202.
- [Google Scholar]
- Marjolin's ulcer of the scalp: Case report and literature review. Ann Burns Fire Disasters. 2001;14:39-42.
- [Google Scholar]
- Marjolin's ulcer of the foot caused by nonburn trauma. South Med J. 1996;89:707-10.
- [Google Scholar]






