Unusual Location of Glomus Tumour on the Right Ring Finger
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Glomus tumour is an uncommon hamartoma arising from glomus bodies which are arteriovenous shunts present mainly in digits and are composed of endothelium lined vascular spaces (Sucquet Hoyer canal) surrounded by glomus cells.[1] It accounts for approximately 1% of all hand tumours.[2] Characteristic triad of temperature sensitivity, severe pain and localised tenderness can be noted in 63-100% of patients.[3] Here we describe a case of glomus tumour at unusual location on the lateral aspect of the right ring finger.
A 42-year-old housewife presented with history of excruciating pain on lateral aspect of distal phalanx of right ring finger since 4 years. The pain was severe, localised to a specific area on the finger and used to aggravate on touching the cold objects, contact with wind and on exposure to cold temperature. The patient had received many anti-inflammatory medications and intra-lesional steroids without any improvement. The area was explored twice under local anaesthesia in past without any specific outcome.
Cutaneous examination revealed an ill-defined area of tenderness present on the lateral aspect of distal phalanx of right ring finger with shiny appearance of overlying skin [Figure 1a]. Nail examination revealed longitudinal beading of the corresponding side of the nail plate [Figure 1b]. Love's test (elicitation of pain by applying pressure to a precise area with the tip of a pencil) was positive while Hildreth's test (disappearance of pain after application of a tourniquet proximally on the arm and raising the pressure to 250 mm of Hg) was negative. Exposure to cold water aggravated the pain indicating cold sensitivity.
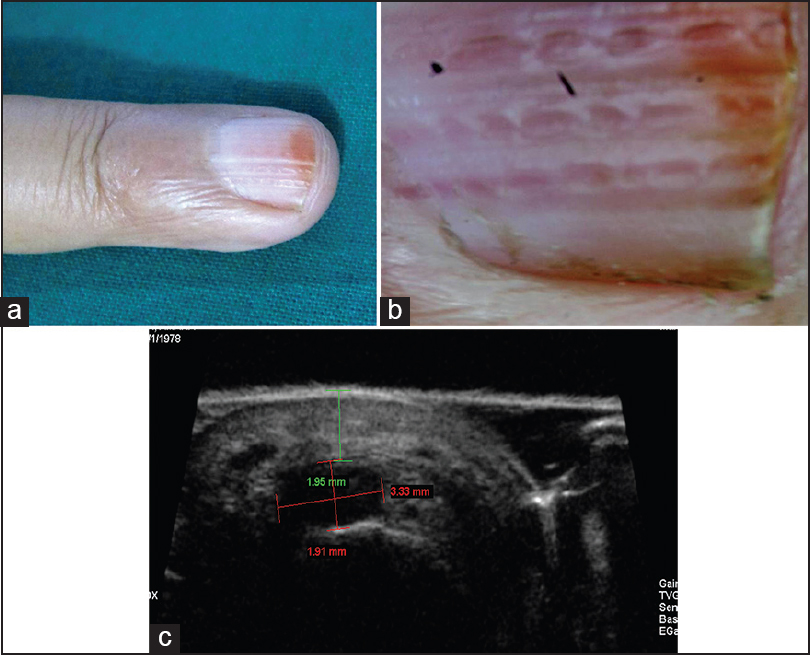
- (a) Cutaneous examination of the right ring finger revealed minimal oedema on the lateral aspect with shiny appearance of overlying skin. (b) Longitudinal beading present on the corresponding side of nail plate of the right ring finger. (c) Ultrasound biomicroscopy in the region of maximum tenderness revealed a well-defined hypoechoic mass lesion measuring 1.91 × 3.33 mm in the subcutaneous tissue. The mass lesion was 1.95 mm from the skin surface. There was mass effect noted on the underlying nail matrix
Ultrasound biomicroscopy (UBM) of tender area revealed a well-defined hypoechoic mass lesion measuring 1.91 × 3.33 mm in the subcutaneous tissue and 1.95 mm from the skin surface. There was mass effect noted on the underlying nail matrix [Figure 1c]. Considering the clinical diagnosis of glomus tumour or neuroma, excision of the tender area was performed under digital nerve block and tourniquet.
Intra-operatively, a semi-translucent mass about 2 × 3 mm was seen lateral to lateral nail fold. [Figure 2a and b] which on histopathology revealed a well-defined tumour in dermis with vascular channels surrounded by solid sheet of uniform rounded tumour cells with eosinophilic cytoplasm and round to oval nuclei thus confirming the diagnosis of glomus tumour [Figure 2c–e].
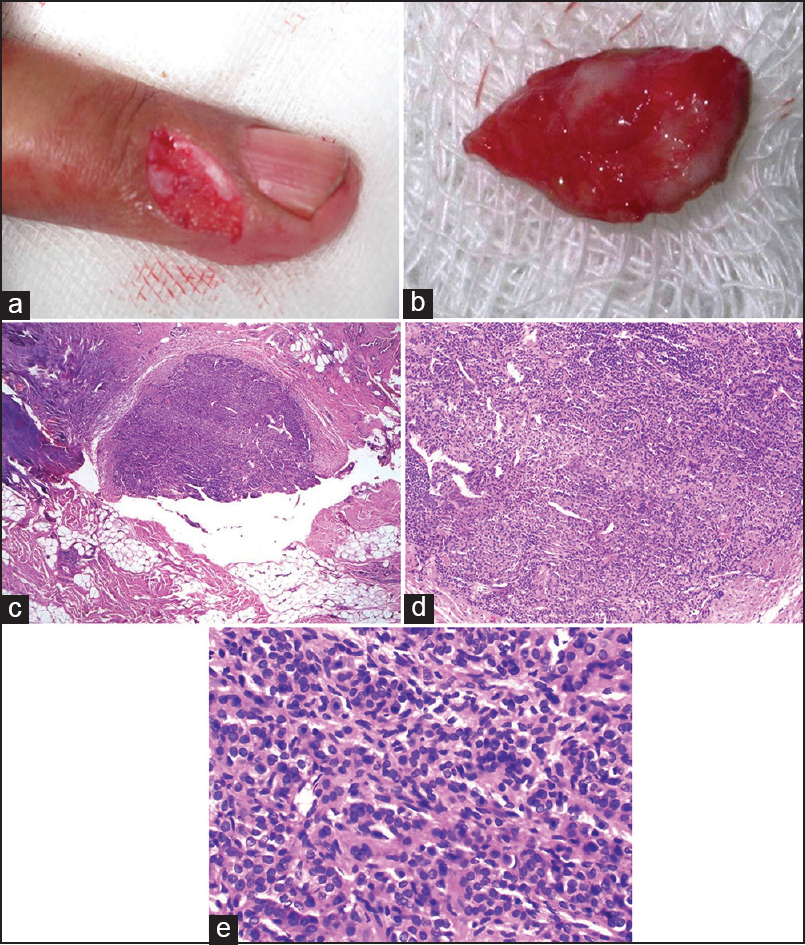
- (a) Elliptical excision of the area of maximum tenderness on the right ring finger. (b) Ventral aspect of the excised tissue revealed semi translucent mass about 2 mm × 3 mm on lateral aspect of lateral nail fold. The excised area was did not reveal any connection to nail apparatus. (c) Histopathology of the resected tissue, H and E stain, 40×: Showed well-defined tumour in dermis with vascular channels. (d) Histopathology, H and E stain, 100×: Tumour composed of vascular channels surrounded by solid sheet of uniform rounded tumour cells with eosinophilic cytoplasm and round to oval nuclei. (e) Histopathology, H and E stain, 400×: Solid sheet of uniform rounded tumour cells with eosinophilic cytoplasm and round to oval nuclei surrounding the vascular channels suggestive of glomus tumour
Post operatively, the wound healed with scaring [Figure 3] and there was complete resolution of the pain.

- Post operatively (after 1 month) the wound healed with scar
Glomus tumour is common between 30 and 50 years of age and occurs spontaneously. It is usually solitary but a multiple glomus tumour syndrome has been described. There is no gender predilection but subungual lesions are more common in women and extra digital glomus tumours are more common in males.[4]
Most glomus tumours occur on the toes and fingertips, particularly beneath the nails. It usually presents as a small, blue-red papule or nodule in the deep dermis or subcutis in acral location (usually subungual or finger pulp). In our case, though the location of the tumour was digital, the patient presented with only symptoms without any obvious mass.[5]
Pain is the most common presenting symptom of glomus tumours and may be spontaneous, often provoked by direct pressure or a change in skin temperature, by gush of wind, and in winter.[2] Tumours beneath the nail are particularly painful, and patients present for treatment while the lesions are still very small and are invisible. The classical triad of severe pain, cold sensitivity and localised tenderness is seen in 63-100% of patients.[3] Cold sensitivity, Hildreth's sign and Love's test are useful in diagnosis of solitary glomus tumours especially painful subungual ones. Cold sensitivity is the most accurate test (100%) aiding in diagnosis of glomus tumour after reviewing different clinical tests.[3]
Nail plate changes depend on the location of the tumour. The affected nail may have a bluish-red flush. Matrix tumours cause splitting and distortion of the nail plate due to compressive effect of the tumour on matrix. Nail bed lesions are most likely to appear as bluish or red foci, 1-5 mm in diameter, beneath the nail. Erythronychia and distal onycholysis may be seen. Dorsal tumours can lead to the nail deformity and bluish discoloration. Our patient had longitudinal beading of nail plate probably due to lateral compression of matrix by the tumour.
The diagnosis is based on clinical symptoms and signs and confirmed by histopathology. Radiographs are of limited usefulness in the diagnosis, while high-resolution MRI is the most sensitive and the primary diagnostic imaging modality of choice. High-resolution USG can detect tumours as small as 3 mm, but small flat subungual lesions can be overlooked.
The treatment of choice for solitary glomus tumour is excision and should be considered in a symptomatic lesion. To prevent nail deformity, periungual approach is preferred for peripheral tumours while transungual approach followed by meticulous repair of the nail bed is preferred for tumours developing in the central region.[1] For lesions that are deep seated proximally, lateral incision through paronychium is recommended.[2]
Recurrence is seen in 20% cases and is mostly due to incomplete excision or local invasion[1] Malignant change is exceedingly rare and account for lt;1% of glomus tumours.
In summary, we report this case for the rare presentation of glomus tumour (severe morbidity with subtle clinical signs). With the strong clinical suspicion and mass lesion on UBM, the area of maximum tenderness was explored. Tumour became apparent on excision of involved area and led to complete resolution of pain. Hence, glomus tumour should be considered in the differential diagnosis of localised excruciating pain over distal extremities without any obvious swelling.
REFERENCES
- Two cases of subungual glomus tumor. Indian J Dermatol Venereol Leprol. 2006;72:47-9.
- [Google Scholar]





