Translate this page into:
Giant Scrotal Lymphoedema
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Massive scrotal lymphoedema or scrotal elephantiasis is an uncommon condition in a temperate climate, causing severe physical limitations and anxiety to patients, leading to disability.[12] It can happen at any age in persons, especially those living in the endemic zones of filaria.[3] Most of the time medical therapy is not effective enough and surgical excision of the involved tissues is performed to treat this unpleasant condition.[4] In this article, we discuss a patient suffering from giant scrotal lymphoedema, who underwent surgical resection.
A 47-year-old man was referred to our centre for gradual enlargement of the scrotum since seven years. Physical examination revealed giant scrotal lymphoedema also involving the right lower extremity with lymphoedema. His penis and both testicles were not palpable and urination was possible through a pit on the scrotum [Figure 1]. The patient had a history of scrotal vesicular lesions in the past, but on physical examination no vesicular lesion was visible. He had no history of travelling to endemic regions with filariasis. No mass or lymphadenopathy was found in the groins, and also, the patient had no history of trauma, radiation or drug injection in his groins. An abdominal computed tomography (CT) scan was normal and blood investigations for filariasis were negative. The patient underwent surgical resection of all the involved tissues weighing about 9 kg [Figure 2]. Fortunately the penile shaft and both the testicles were normal [Figure 3] and the final reconstruction was done in a Y-shaped manner, with the root of the penis in the centre [Figure 4]. Histopathologic evaluation revealed extensive fibrosis in the resected specimen, with no sarcomatous changes noted [Figure 5], and patient had an uneventful post-operative course [Figure 6].

- Giant scrotal lymphoedema

- Removed specimen

- Penis and both testicles were intact after resection

- Final result after reconstruction
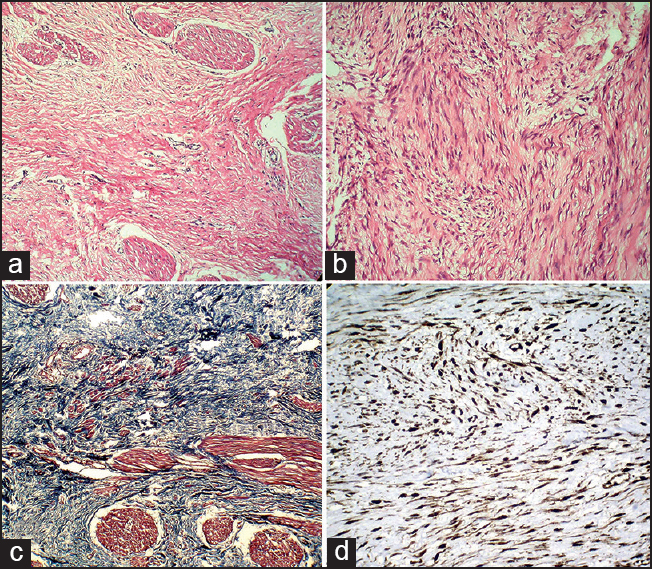
- (a) Spindle myofibroblastic cells spreading between the scrotal muscle fibers and separating them (H and E) (b) Irregular fascicles of the proliferated bland myofibroblastic cells (H and E) (c) Trichrome staining shows abundant stromal collagen (blue fibers) (d) Immunohistochemical staining and Trichrome staining show positive reactivity of the lesional cells with betacatnin

- Post-operative appearance after one year
Any disturbance of the normal lymphatic drainage from the external genitalia, such as, an obstruction or defect in the formation of lymphatic vessels, results in lymphoedema of the scrotum.[56] Dilated lymphatic vessels are seen because of this obstruction. The etiology may be congenital and acquired. The most common acquired aetiology is infection by Wuchereria bancrofti or Chlamydia trachomatis with the other etiologies being radiation, venous thrombosis, malignancy, inflammation, trauma, surgical intervention, drug injections, and so on.[78] At first, the oedema is painless, pitting, and rich in protein, causing features of elephantiasis. Later, fibrosis occurs, making the scrotal skin coarse and indurated.[15] Urogenital manifestations, such as, urinary incontinence and loss of libido, besides recurrent cellulitis, may occur.[9] The treatment approach is based on the aetiology of the oedema. For example, antibiotics and anti-parasite drugs can cure the early stages of the disease caused by infection. However, in advanced disease the mainstay of treatment remains surgery.[10] In our case, on account of lack of other risk factors, the probable aetiology was filariasis, however, we were unable to prove it. There are two types of surgeries. Lymphangioplasty (in the presence of good lymphatic channels), which is performed to restore the drainage of the lymph, and the second, lymphangiectomy, which is excision of all the affected skin and subcutaneous tissue that is a superficial lymphatic network above the Buck`s fascia. Following this, reconstruction of the region of the genitalia by local tissue flaps, such as, the skin of the posterior scrotum (medial thigh flap if scrotal flap is not possible) or skin grafts (not recommended because of altered thermal regulation of testes) is performed.[111] Cosmetic issues must be considered beside preservation of the penis, testes, and spermatic cords, as also resumption of the proper function.[12] The complications of giant scrotal lymphoedema surgery include hemorrhage, hematoma, iatrogenic injury to the urethra, infection, painful erection, decreased sensation, and also recurrence.[1213]
REFERENCES
- Elephantiasis of the penis and scrotum: A review of 350 cases. Am J Surg. 1985;149:686-90.
- [Google Scholar]
- Scrotal and penile lymphoedema: Surgical considerations and management. J Urol. 1983;130:263-5.
- [Google Scholar]
- Overview of treatments for male genital lymphoedema: Critical literature review and anatomical considerations. Plast Reconstr Surg. 2012;129:767e-9e.
- [Google Scholar]
- Giant scrotal elephantiasis of inflammatory aetiology: A case report. J Med Case Rep. 2007;1:23.
- [Google Scholar]
- Localized lymphoedema (elephantiasis): A case series and review of the literature. J Cutan Pathol. 2009;36:1-20.
- [Google Scholar]





