Translate this page into:
The Liquid Lift: Looking Natural Without Lumps
Address for correspondence: Dr. Iñigo de Felipe, Calle Provenza 290 ppa 2, Barcelona - 08008, Spain. E-mail: idefelipe@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Hyaluronic acid (HA) is the most common filler used to rejuvenate. Today, a three-dimensional approach prevails over previous techniques in which this material was used in specific areas of the face such as the nasolabial fold, the marionette line, and the eye trough giving a strange appearance that does not look natural. Even with a volumizing purpose, the injection of HA can sometimes produce clinically detectable nodules or lumps where the filler is deposited.
Aims:
To develop a new technique of injecting HA that can provide more natural results and avoid the lumpiness and nodular appearance that sometimes occurs with the injection of HA. To detect whether mixing HA with diluted anesthetic agent modifies its behavior.
Settings and Design:
Prospective, case control, single-center study on a private clinic setting.
Materials and Methods:
Eighty six patients were enrolled in this study. All of them had a previous treatment with nondiluted HA using a needle at least a year before. Patients were injected with 8 mL of reticulated HA (RHA) mixed with 6 mL of saline and 2 mL of anesthetic agent. The mixture was administered through a cannula inserted in the face, one at mid-cheek and another at frontal-temporal point of entry. Owing to the lifting effect of this mixture we called this procedure liquid lift (LL). Patients were evaluated 1 month, 6 months, and a year later and asked to compare the LL with previous experiences in terms of natural look, pain, and appearance of nodules.
Statistical Analysis Used:
Student's t-test.
Results:
One month after the treatment, 83 out of 86 patients (96.5%) thought LL produced a more natural look than the previous treatment with the needle. Sixty two (72%) considered LL less painful than the previous treatment and only eight (9.3%) could detect lumps or nodules 1 month after LL was performed compared with 46 (53.5%) that described this problem with previous needle injections. The incidence of bruising was also clearly lower (7% with LL vs 17.4% with traditional needle).
Conclusions:
Injection of diluted HA with saline and anesthetic agents through a cannula all over the face or LL can provide more natural results and less lumps or nodules, and is less painful than traditional treatments involving needle injection of nondiluted HA.
Keywords
Face
filler
hyaluronic acid (HA)
lifting
rejuvenation
wrinkles
INTRODUCTION
Reticulated hyaluronic acid (RHA) is the most common filler used for rejuvenation of certain areas of the face.[1] According to the American Society of Plastic Surgeons, 1.9 million filler procedures were performed in 2011. Of these, hyaluronic acid (HA) was the most common filler used reaching 1.3 million procedures which represents more than 70%. HA is easy to inject, safe, and relatively cheaper, reasons for which it is so widely used.[2]
Most studies done with this filler evaluate the results of injecting it in certain specific areas such as the wrinkles, the nasolabial fold, or the marionette line.[3456] Some methods recommend specific eight points to inject in the face in order to rejuvenate.[7] Nevertheless the flaccidity and ageing appearance occurs because of the loss of volume affecting the full surface of the face and not just some lines or points as the folds or winkles described before.[8] It is estimated that 90% of the connective tissue or dermis is collagen and most of it is lost throughout life.[9] It is often said and considered that the recovery of part of this volume in some areas of the face such as the cheeks or the infraorbital region induces a “lifting” effect that is used to rejuvenate patients.[1011] Today most injectors are looking for a regular recovery of volume all over the face rather than specific points or wrinkles.[1213]
The combination of both the objectives of “lifting” effect and full face skin thickness recovery has inspired the design of the liquid lift (LL) technique.
Also important when injecting a filler is to be able to deploy the filler without causing irregularities, lumpiness, and over- or undercorrections in order to provide a “natural look.”[6] Many approaches have been used in developing new injection techniques, combining treatments or considering the face as a multilayer structure.[1415] As of today, nevertheless, no study has considered using saline or water as a means of “dissecting” the subcutaneous structures and using “liquid” as a means of transporting and placing RHA homogenously in the correct place.
The use of needles causes bruising and is one of the most common adverse effects of using HA.[16] This adverse effect can be avoided with the use of cannulas. One of the worst adverse events that can occur when injecting RHA is that part of the filler can reach the retinal artery through superficial arteries in the face.[17] Thankfully very infrequent, this may happen when blood flow is reverted and has only been described with the injection of RHA with a needle.[18] This effect has never happened when using cannulas.
Our aim was to develop a method of injecting RHA in the face that meets the following criteria:
-
Reduce the lumpiness and incidence of nodules after the injection.
-
Reduce the incidence of bruising or ecchymosis.
-
Distribute the filler homogenously along the face and not focally in some anatomical landmarks.
-
Minimize trauma and pain.
In order to reduce the incidence of lumps and nodules, we suggest to dilute or mix the RHA with a tumescent anesthetic agent. In our study, we mix equal volumes of RHA with saline and mepivacaine 0.5%. In order to reduce the incidence of bruising, we suggest to use a cannula. In our study, we use 21G 70 mm cannulas. Cannulas also minimize trauma and pain as they are blunt and very seldom traumatize vessels or nerves. In order to distribute RHA homogeneously, we use a central point in the cheek from where it is easier to reach all areas of the face and an additional point in the lateral aspect of the forehead. In order to minimize trauma and pain, we mix RHA with diluted anesthetic agent.
MATERIALS AND METHODS
Patients were reviewed for their medical history with special attention to filler allergies, drug allergies, or medication used. Patients were explained about the procedure and they gave informed consent about the procedure and RHA.
For the LL 8 mL of RHA (Perfectha Subskin, Sinclair Pharma, London, UK) was mixed with 6 mL of saline and 2 mL of mepivacaine 0.5%. To mix this product and to make a 16 mL mixture we used two 10 mL Luer lock syringes connected with a three way key opened in two of its three ways. The product was then transferred to 1 mL Luer lock syringes that were connected to a 21G 70 mm cannula. This cannula was inserted in the subcutaneous tissue of the face prior to cleaning of the area with povidone-iodine solution injected through a mid-cheek entry point (point A) [Figure 1] made by a 21G needle, and an additional entry point in the posterior side of the frontotemporal area (point B). A volume of 8 mL of the product was injected in each side of the face through multiple passes of the cannula to distribute this “liquid” within the subcutaneous tissue in eight different areas as follows:
-
Eye trough and lower eyelid,
-
Anterior aspect of the malar area,
-
Posterior aspect of the malar area,
-
Preauricular and mandible angle,
-
Nasolabial fold,
-
Marionette line,
-
Brow and supraciliar area, and
-
Frontotemporal hollow [Figure 1].

- (a and b) Points of entry with a 21G cannula. Also depicted are areas of injection of the mixture of RHA and saline with anesthesia, (1-8), 1 mL per site
Eighty six patients have been treated in the face between 2013 and 2015. Out of these patients, 81 were females and 5 were males. The average age of the patients was 53 years ranging from 41 years to 69 years. Patients were reported not to have undergone any previous procedure with permanent fillers or any other procedure in the previous year. In order to be able to compare the experience of the LL with other ways of injection, all patients selected had been treated at least a year before by injecting RHA with a needle in their face.
Patients were followed up 1 month, 6 months, and a year after the injection and were asked to rate the results with previous experiences with RHA as:
-
Far better,
-
Better,
-
Similar,
-
Worse, and
-
Far worse in terms of natural look of the results, pain, and appearance of lumps or nodules.
RESULTS
Table 1 and Figure 2 summarize the response of patients at 1-month follow-up. One month after the treatment, 83 out of 86 patients (96.5%) thought that the LL produced a more natural look than the previous treatment with the needle. Sixty two (72%) considered LL less painful than the previous treatment and only 8 (9.3%) could detect lumps or nodules 1 month after the LL was performed compared with 46 (53.5%) who described this problem as a result of the previous needle injections. The incidence of bruising was also clearly lower (7% with LL vs 17.4% with traditional needle).
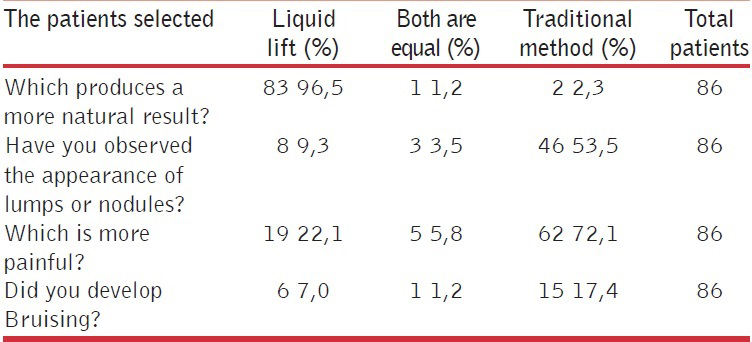
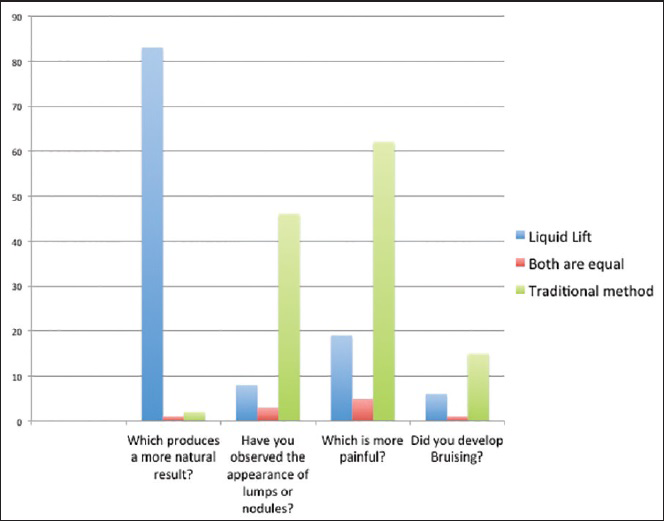
- Responses of patients when comparing LL against traditional needle injection of nondiluted RHA
The LL procedure takes 15 min to finish. Patients look very natural immediately after the injection and are able to resume their regular activities [Figure 3]. At 1-month follow-up, the volume restoration is remarkable and no lumpiness or irregularities was noted [Figures 4 and 5].

- Forty four year old female patient before and after a LL procedure with 8 mL RHA mixed with 8 mL saline and mepivacaine 0.5%. On the mid malar area, it is possible to see a small stich that covers the injection site where the cannula enters to deliver the filler

- Sixty two year old female patient before and 1 month after the LL procedure was performed. The flaccidity over the face as well as the neck area improves as a consequence of the recovery of volume in the upper face areas

- Sixty two year old female patient before and 1 month after the LL procedure was performed. The flaccidity over the face as well as the neck area improves as a consequence of the recovery of volume in the upper face areas
DISCUSSION
Today, RHA is the most widely used filler because it is thought to be safer than other products.[19] This being basically true, there have been reports describing several problems arising from RHA injection.[420] In a recent report of 38 women presenting with filler adverse reactions only 52,6% were due to silicone. Up to 18,4% of the total 38 cases were induced by RHA.[21] Adverse reactions included nodules, plaques, and skin changes indicating that RHA is not completely innocuous.[21] In a recent report it was observed that for a total of 2,089 injectable soft-tissue filler treatments performed, including 1,047 with RHA, 811 with poly-L-lactic acid (PLLA), and 231 with calcium hydroxylapatite, there were 14 complications. The most common of these was nodule or granuloma formation.[22] The treatment with calcium hydroxylapatite had the highest complication rate.
Of particular importance to us is the fact that the use of a needle is not capable of depositing RHA homogeneously in the skin of the face, and more specifically because we humans loose collagen all over the surface of our skin but still injectors treat specific areas such as the nasolabial folds, the lips, or the frontal aspect of the cheeks.[2324]
The LL method is inspired by several facts. First, it is believed that the deposition of the filler should look very naturally distributed and smooth in appearance. This belief contrasts with the very common approach of injecting in special points that act as lifting points or “pillars of a tent,” as described in some works,[25] or wrinkle filling of the skin.[26] If we assume that fillers should induce new collagen as well as restore the volume loss of the face, whatever method used must distribute the filler homogenously all over the face. Such idea inspires fat tissue injection, PLLA treatment, or injection of other “collagen inducers” such as polycaprolactone. We advocate that depositing RHA in small amounts through large surfaces of the skin is also better to induce fibroblasts to synthesize new collagen. It is very clear that RHA can enhance the manufacture of new collagen and it does not seem worse than other products;[242728] One recent study detected that RHA could improve 1.54 points in the Wrinkle Severity Rating Scale in comparison with 2.09 points improved by PLLA. Second, we believe that all HA are composed of particles some of which are “glued” with noncross-linked HA. Therefore, its separation, that will occur naturally once injected into the dermis, should not affect basic properties such as longevity or pH of the skin.
The amount of RHA used might be considered large if taken into account the price of these materials. Nevertheless we have to point out that the fact that each year the skin of our face losses about 2-mL volume of collagen. Therefore, patients treated in this study with 8 mL of RHA, rejuvenate in approximately 4 years. Nevertheless we can make variations of this procedure and inject lesser amounts of filler, adjusting the cost of it to the patients’ budget. In fact, it is far more common to use smaller volume of this solution due to the constraints of price.
In order to reduce pain, we have added the anesthetic agent with the mixture. It is argued that injecting the filler and the anesthetic agent at the same time does not reduce the pain at the time of the injection. This is not true as the cannula crosses the subcutaneous tissue several times in the same areas in order to distribute the filler in very small amounts. Once the cannula passes through one area and delivers part of the anesthetic effect, the tissue is anesthetized and further passes are not painful for the patient. In fact, we have been using a similar method, for example, the tumescent anesthesia of liposuction but the pain was important. Performing tumescent anesthesia before the procedure is not only painful but also deforms the facial skin areas to be later treated with the LL method.
The appearance of lumpiness and nodules when injecting RHA or other fillers is one of the major problems and is not quite often studied in the literature. Patients consider this complication makes results “not look natural” because they can detect where the filler has been injected. In fact, it is referred to as “undercorrection,” “overcorrection,” and “lumpiness” in many papers.[29] We think that these terms describe the incorrect placement of the filler that maybe caused by the failure on the doctors’ part to reproduce the natural distribution of volume in the face. in order to achieve a great result. Fillers should not be detected or discovered where they are but rather mimic the natural anatomy of the patient's face. We think that diluting the filler with saline considerably reduces the risk of lumpiness or nodules. This becomes very obvious in thin skin areas like the infraorbital region. To our knowledge, several protocols have been developed to avoid this problem but none diluting or mixing the RHA as in this study.[30]
The use of a cannula provides several advantages as follows: It diminishes the bruising, causes less pain, provides more accessibility of the filler to more areas in the face, and reduces the risk of developing retinal artery occlusion. This last event has never been described happening with a cannula and we imagine this is due to the difficulty of cannulas penetrating the lumen of an artery.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- Hyaluronic acid gel fillers in the management of facial aging. Clin Interv Aging. 2008;3:153-9.
- [Google Scholar]
- In vivo bio-integration of three hyaluronic acid fillers in human skin: A histological study. Dermatology. 2014;228:47-54.
- [Google Scholar]
- A prospective, randomized, parallel group study analyzing the effect of BTX-A (Botox) and nonanimal sourced hyaluronic acid (NASHA, Restylane) in combination compared with NASHA (Restylane) alone in severe glabellar rhytides in adult female subjects: Treatment of severe glabellar rhytides with a hyaluronic acid derivative compared with the derivative and BTX-A. Dermatol Surg. 2003;29:802-9.
- [Google Scholar]
- Undesirable effects after treatment with dermal fillers. J Drugs Dermatol. 2013;12:e59-62.
- [Google Scholar]
- Efficacy and safety of a new monophasic hyaluronic acid filler in the correction of nasolabial folds: A randomized, evaluator-blinded, split-face study. J Dermatolog Treat. 2014;25:448-52.
- [Google Scholar]
- Rejuvenation effects of hyaluronic acid injection on nasojugal groove: Prospective randomized split face clinical controlled study. J Cosmet Laser Ther. 2014;16:32-6.
- [Google Scholar]
- Full-face rejuvenation using a range of hyaluronic acid fillers: Efficacy, safety, and patient satisfaction over 6 months. Dermatol Surg. 2012;38:1153-61.
- [Google Scholar]
- Looking older: Fibroblast collapse and therapeutic implications. Arch Dermatol. 2008;144:666-72.
- [Google Scholar]
- Under eye infraorbital injection technique: The best value in facial rejuvenation. J Cosmet Dermatol. 2014;13:79-84.
- [Google Scholar]
- Full face rejuvenation in three dimensions: A “face-lifting” for the new millennium. Aesthetic Plast Surg. 2001;25:152-64.
- [Google Scholar]
- Facial assessments: Identifying the suitable pathway to facial rejuvenation. J Eur Acad Dermatol Venereol. 2006;20(Suppl 1):7-11.
- [Google Scholar]
- Contour restoration of the forehead by lipofilling: Our experience. Aesthetic Plast Surg. 2012;36:761-6.
- [Google Scholar]
- A novel, multistep, combination facial rejuvenation procedure for treatment of the whole face with incobotulinumtoxinA, and two dermal fillers- calcium hydroxylapatite and a monophasic, polydensified hyaluronic acid filler. J Drugs Dermatol. 2013;12:978-84.
- [Google Scholar]
- Comparison of two techniques using hyaluronic acid to correct the tear trough deformity. J Drugs Dermatol. 2012;11:e80-4.
- [Google Scholar]
- The evolution of soft tissue fillers in clinical practice. Dermatol Clin. 2005;23:343-63.
- [Google Scholar]
- Panophthalmoplegia and vision loss after cosmetic nasal dorsum injection. J Clin Neurosci. 2014;21:678-80.
- [Google Scholar]
- Bacterial biofilm formation and treatment in soft tissue fillers. Pathog Dis. 2014;70:339-46.
- [Google Scholar]
- Adverse reactions to injectable soft tissue fillers: Memorable cases and their clinico-pathological overview. J Cosmet Laser Ther. 2015;17:102-8.
- [Google Scholar]
- Dermal filler complications: A clinicopathologic study with a spectrum of histologic reaction patterns. Ann Diagn Pathol. 2015;19:10-5.
- [Google Scholar]
- Complications associated with injectable soft-tissue fillers: A 5-year retrospective review. JAMA Facial Plast Surg. 2013;15:226-31.
- [Google Scholar]
- A multicenter, randomized, double-blind clinical study to evaluate the efficacy and safety of PP-501-B in correction of nasolabial folds. Dermatol Surg. 2015;41:113-20.
- [Google Scholar]
- Efficacy and safety of injection with poly-L-lactic acid compared with hyaluronic acid for correction of nasolabial fold: A randomized, evaluator-blinded, comparative study. Clin Exp Dermatol. 2015;40:129-35.
- [Google Scholar]
- Anatomic and mechanical considerations in restoring volume of the face with use of hyaluronic acid fillers with a novel layered technique. Indian J Plast Surg. 2014;47:43-9.
- [Google Scholar]
- Remodeling of periorbital, temporal, glabellar, and crow's feet areas with hyaluronic acid and botulinum toxin. J Cosmet Dermatol. 2014;13:143-50.
- [Google Scholar]
- In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Arch Dermatol. 2007;143:155-63.
- [Google Scholar]
- An experimental study of tissue reaction to hyaluronic acid (Restylane) and polymethylmethacrylate (Metacrill) in the mouse. Am J Dermatopathol. 2012;34:716-22.
- [Google Scholar]
- Hyalurostructure treatment: Superior clinical outcome through a new protocol-a 4-year comparative study of two methods for tear trough treatment. Plast Reconstr Surg. 2013;132:924e-31e.
- [Google Scholar]






