Translate this page into:
Efficacy and Safety of Fractional CO2 Laser Resurfacing in Non-hypertrophic Traumatic and Burn Scars
Address for correspondence: Dr. Imran Majid, G30, Green Lane SA Colony, Hyderpora Srinagar, Kashmir, India. E-mail: imran54@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Fractional photothermolysis is one of the most effective treatment options used to resurface scars of different aetiologies.
Aim:
To assess the efficacy and safety of fractional CO2 laser resurfacing treatment in the management of non-hypertrophic traumatic and burn scars.
Materials and Methods:
Twenty-five patients affected by non-hypertrophic traumatic and burn scars were treated with four sessions of fractional CO2 laser resurfacing treatment at 6-weekly intervals. Patients were photographed at each visit and finally, 3 months after the end of treatment schedule. Response to treatment was assessed clinically as well as by comparing the initial photograph of the patient with the one taken at the last follow-up visit 3-months after the final treatment session. Changes in skin texture, surface irregularity and pigmentation were assessed on a quartile grading scale and scored individually from 0 to 4. A mean of the three individual scores was calculated and the response was labelled as ‘excellent’ if the mean score achieved was >2. A score of 1-2 was labeled as good response while a score below 1 was labeled as ‘poor’ response. The subjective satisfaction of each patient with the treatment offered was also assessed at the last follow-up visit.
Results:
The commonest site of scarring treated was the face followed by hands. Response to treatment was rated as excellent in 60% (15/25) patients while 24% (6/25) and 16% (4/25) patients were labeled as good and poor responders, respectively. Skin texture showed better response than other variables with average score of 2.44. Linear post-traumatic scars were seen to respond less than other morphological types. Majority of the patients (19 out of 25) were highly satisfied with the treatment offered. No long-term adverse effects were noted in any patient.
Conclusions:
Fractional photothermolysis with a fractional CO2 laser gives excellent results in patients with post-burn scars with minimal adverse effects.
Limitations:
Lack of a control group and small sample size are limitations of this study.
Keywords
Burn scars
fractional laser resurfacing
scars
traumatic scars
treatment
INTRODUCTION
Scarring is the most important long-term complication of burn injuries or trauma on the skin. Treatment options for managing such scars are limited to surgical correction, dermabrasion or laser resurfacing techniques. Lasers employed for resurfacing of scars are divided into ablative and nonablative lasers. Laser resurfacing is supposed to work by stimulating collagen production in the dermis and by dermal remodeling of collagen fibers.[1234]
Carbon dioxide (CO2) laser is an ablative laser device that produces energy in the far-infrared region at a wavelength of 10,600 nm. Resurfacing with CO2 laser is highly effective in treating scars and ageing skin. However, a really long down-time and high incidence of adverse effects has limited its use in routine dermatology practice.[5] Some long-term adverse effects can also occur including permanent hypopigmentation, hyperpigmentation and permanent scarring.[67]
Fractional photothermolysis (FP) circumvents many of the above-mentioned disadvantages of laser resurfacing.[89] With FP, only a fraction of the whole skin is treated in a pixelated pattern while the intervening skin remains intact. Treatment with FP leads to formation of longitudinal microthermal zones (MTZs) in the skin which are separated by healthy, untreated skin with an intact epidermis. This allows the treating physicians to go for much deeper treatment than with traditional laser resurfacing. Additionally, the adverse effects encountered with FP are transient and less severe than with full skin resurfacing.[1011] Fractional CO2 laser resurfacing has been successfully used in the treatment of atrophic acne scars and for skin rejuvenation.[121314151617] There are also some reports of its usefulness in hypertrophic as well as burn scars.[18192021222324252627] The fractional CO2 laser device used in this patient series was Qray-FRXR system manufactured by Dosis, Korea that provides an output ranging from 1 to 30 J/cm2 and a variable spot size of 1 to 20 cm2.
MATERIALS AND METHODS
Over a period of 1-year from August 2012 to July 2013, 25 patients suffering from non-hypertrophic post-burn and post-traumatic scars were treated with multiple sessions of FP with ablative CO2 laser. Patients with keloidal tendency, patients with connective tissue disorders or hypersensitivity to lidocaine and pregnant females were excluded. Treatments were carried out at 4-6 week intervals and a total of four sessions were performed. A single physician (author 2) performed all the laser sessions while another observer (author 1) assessed the response to treatment.
After an informed written consent for laser resurfacing, a baseline photograph of the scar to be treated was taken using standard camera angle and light settings. The scar to be treated was assessed for its texture, pigmentation and surface distortion as per Table 1. Prior to treatment, a topical anaesthetic cream containing a combination of topical tetracaine and lignocaine in a cream base (TetralidR cream) was applied for 1 hour on and around the scar area. After satisfactory anesthesia was achieved, the treatment area was cleaned with a mild cleanser followed by 70% ethanol solution. Fractional CO2 laser treatment was then delivered to whole of the scar area. Fluence ranging from 20 to 28 J/cm2 were used at densities of 150-200 MTZ/cm2, thus providing about 45-50 mJ of energy at each spot. A double pass was used at each treatment session, stacking the pulses one upon another. The shape of the treatment spot was varied according to the shape of the scar to be treated and ‘random’ pattern of laser delivery was chosen for treatment. A topical antibiotic in cream formulation was prescribed after the procedure for a period of 4-5 days. No oral antibiotics were used and oral acyclovir was prescribed only to those patients who had a history of recurrent herpes simplex infections.
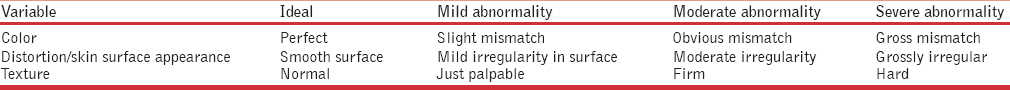
Laser sessions were repeated at 4-6 week intervals and a total of four sessions were performed in each patient. The laser parameters were kept identical at each visit and care was taken to treat the whole scar including the margins in a uniform manner. At each follow-up visit the scar was photographed and examined for any change in skin texture, appearance (distortion) and pigmentation from baseline [Table 1]. Response to treatment was finally assessed at the last follow-up visit, 3-months after the final laser session. A quartile grading scale was used to assess the improvement in each variable individually and a score of 0, 1, 2, 3 and 4 was given if the improvement was 0%, 25%, 50%, 75% and 100%, respectively. The final score was calculated by finding an average/mean of the three individual scores obtained in skin texture, distortion and pigmentation. Response to treatment was termed as excellent if the final score (average of individual scores) was >2 and good if the score obtained was between 1and 2. Patients getting a score of <1 were termed as ‘poor’ responders. Adverse effects, if any, were also monitored at each follow-up visit.
In addition to the photographic and clinical assessment, the patients themselves assessed the effect of treatment offered as well. Patients recoded their assessment as ‘highly satisfied’, ‘somewhat satisfied’ and ‘not satisfied’ and this subjective assessment was also carried out at the last follow-up visit.
RESULTS
There were 14 females and 11 males in the study group and age ranged from 14 years to 35 years with a mean of 22.1 years. Majority of patients belonged to Fitzpatrick Skin type 3 and we had 3, 15 and 7 patients with skin types 2, 3 and 4, respectively.
All the 25 patients completed four sessions of fractional laser treatment and there were no drop outs. Patients tolerated the procedure well and only mild pain was felt during the procedure. Adverse effects seen were transient and included post-treatment erythema and crusting for 2-4 days and post-inflammatory pigmentation in two cases who were treated for linear scars on the face. The post-inflammatory pigmentation persisted for a few months after the treatment and resolved afterwards with the use of topical creams.
At the time of final assessment, the individual scores for the three variables in each of the patients are given in Table 2.
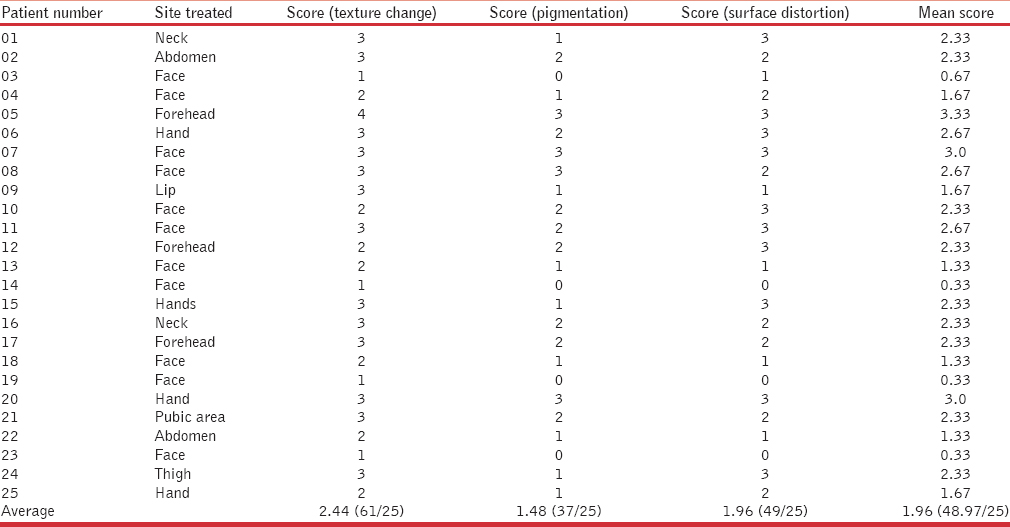
The commonest site treated was the face (in 16 patients) followed by hands (four patients). Other areas treated were neck, abdomen and pubic area [Table 2].
The age of scars that were treated ranged from 8 months to 15 years with a mean of 6.72 ± 3.38 years. Majority of the patients (12 out of 25) had scars of 5-10-year duration [Table 3].
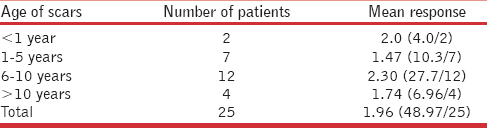
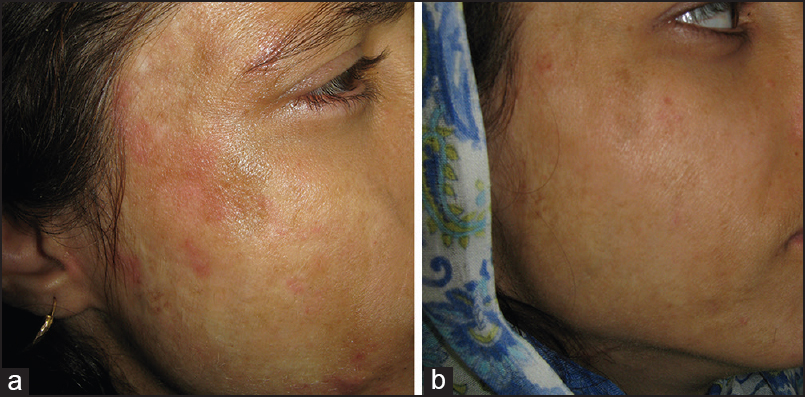
A positive response to treatment was observed in 84% (21/25) patients. Of these 60% (15/25) patients achieved excellent response [Figure 1a and b] with a mean score of >2 at the final assessment while 24% (6/25) patients showed good response with mean score of 1-2. Three patients (12%) were able to achieve ≥75% improvement with a total score of ≥3.0. Only four patients (16%) failed to achieve a significant improvement in their scars with a mean score of <1.0. All of these four patients had linear post-traumatic scars on the face [Table 2].
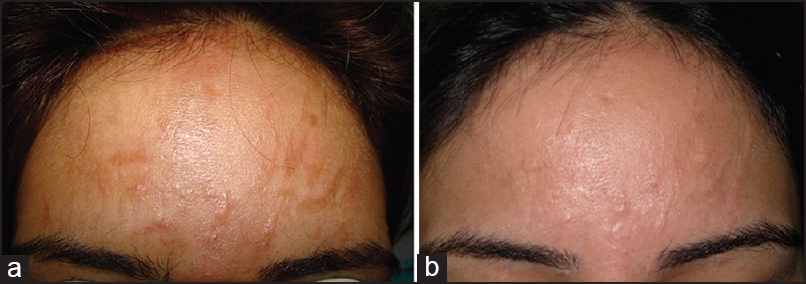
- (a) Post-traumatic scars from a road traffic accident (b) After treatment with four sessions of fractional laser resurfacing
Among the three variables assessed, skin texture showed the best response with an average score of 2.44 when calculated for the whole group. In addition to showing the best response, skin texture was also the earliest to respond to treatment. A positive change in skin texture was noticed even after the first session of fractional laser resurfacing.
We could not correlate the response achieved with the site of the scar as the number of patients in different groups was too small.
More than the site, it was the morphology of the scar that had an effect on the final response. Diffuse scarring, either post-trauma or post-burn, responded significantly better [Figure 2a and b] than linear traumatic scars [Figure 3a and b].

- (a) Post-traumatic atrophic scars on face (b) After four sessions of fractional CO2 treatment
- (a) Post-burn scars on face (b) After four sessions of fractional laser treatment
Subjective assessment by the patients was also carried out at the last follow-up visit. Majority of the patients were satisfied with the treatment offered with 76% (19/25) rating their response as ‘highly satisfied’ while six patients were ‘not satisfied’ with the treatment results. Four out of these six patients had poor results to FP on objective assessment.
DISCUSSION
Treatment options for post-traumatic or post-burn atrophic scars are limited and none of these options guarantee a perfect outcome. Even if the scar is amenable to surgical excision or scar revision, the final cosmetic result is still not expected to be ‘perfect’ as some residual scarring remains even after a scar is surgically treated. Fractional laser resurfacing has been used with success in treatment of post-acne atrophic scars of varied morphology.[121314151617] Similar therapeutic benefit can be expected in post-traumatic and post-burn scarring because the process underlying all these aetiological types of scars is fundamentally the same. A number of ablative as well as non-ablative fractional laser devices have been employed in the treatment of burn scars with varying degree of success. In one of the earliest studies on fractional lasers in burn scars, a mature scar was shown to improve considerably after 5 monthly sessions with a fractional Er:YAG device.[24] The authors reported improvement in the scar appearance as well as contracture. Another study on non-ablative Er:YAG laser documented a significant improvement is skin texture after 3 monthly sessions in a randomized controlled trial.[19]
Fractional CO2 laser has been shown to be effective for burn scars even in patients with dark skin types. Additionally no permanent dyschromia has been noted in these clinical studies after the use of fractional CO2 devices.[2526] Studies have documented histopathological evidence of a significant increase in Type 3 collagen and decrease in Type 1 collagen after fractional CO2 laser resurfacing on a burn scar.[27]
Scars resulting from burns are usually hypertrophic in nature and this type of scarring is considered to be more difficult to treat. To assess the severity of burn scars and their response to treatment many scoring systems have been utilized like the Visual analogue scale (VAS), Vancouver scar scale (VSS), Manchester scar scale (MSS) and Patient and observer scar assessment scale (POSAS).[28293031] All of these scoring systems are useful mainly in assessing the severity of hypertrophic and keloidal burn scars. Clinical studies have employed these scoring systems in assessing the scar severity as well as response to treatment. We used the same variables as mentioned in MSS scoring while assessing our results but we omitted the two variables of ‘scar contour’ and ‘matte vs shiny’ in our scoring scale.[25] This was done because the study was confined to treatment of atrophic/non-hypertrophic scars and, therefore, flattening of scars (effect on contour) was not applicable in assessing the therapeutic response.
Physician-based assessment included three variables of skin texture, distortion and pigmentation of the scars. We noticed improvement in all of these variables but skin texture improved the most after fractional laser resurfacing. Improvement in skin texture was appreciated by a soft and more uniform appearance as well as feel of the scarred skin [Figure 4 and b]. Skin texture was also the first to show an appreciable response with patients as well as investigators noticing improvement even after the initial session of laser resurfacing [Figure 5a and b]. Pigmentation over the scars also improved gradually and this also contributed to the change in overall appearance of the scar. However, totally depigmented scars did not show any repigmentation with fractional laser resurfacing and needed additional treatment modalities like skin grafting to take care of this abnormality.
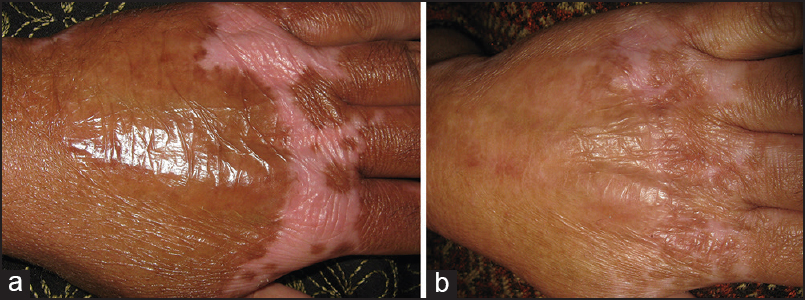
- (a) Post-burn scars on hand (b) Significant clinical response after fractional CO2 laser treatment
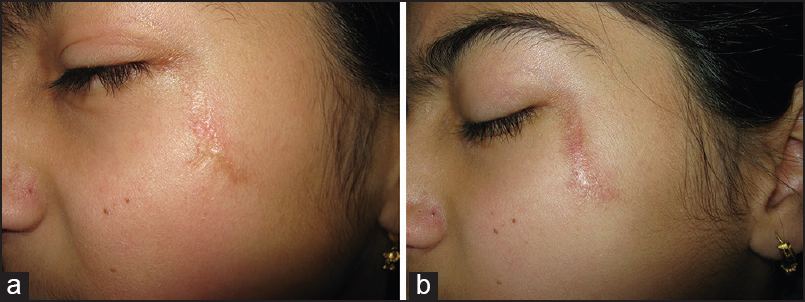
- (a) Linear post-traumatic scar (b) Minimal response to treatment
To quantify the response in each patient, the mean of all the scores achieved in the three variables was calculated to get the final score. This was done to give due importance to all the different aspects of scar appearance. Even when one variable like skin depigmentation did not respond the patients did notice a positive result in other variables like skin texture and surface irregularity. Data from our study suggests that fractional laser resurfacing with CO2 laser is a safe and effective treatment option in post-burn and post-traumatic scars. Scars anywhere on the body are expected to respond to this treatment modality with moderately good to excellent results. We used four sessions of fractional laser resurfacing at 4-6 weekly intervals in all our patients and treated scars at almost all the different sites on the body. Both the investigators as well as patients noted improvement in scar appearance at the last follow-up visit. Additionally, there was a good correlation between the investigator and patient-based assessment with four out of the six unsatisfied patients reporting poor results on objective assessment as well.
Clinical improvement in scar appearance is a complex issue as it depends upon many factors like the uniformity of the skin surface, wrinkling, pigmentation and volume of scarring. While all of these variables respond positively, the extent of improvement is not uniform over this spectrum. Thus, the scar volume or pigmentation may not show the same amount of improvement as the wrinkling or non-uniformity of the scar surface. This makes it important to employ a score that takes into account all of these variables individually. It also means that assessing just the volume change in a scar by objective tools is not sufficient enough to gauge the response to fractional laser resurfacing or any other treatment option for scars.
Another important variable that should ideally be included while assessing the therapeutic response to laser resurfacing is the improvement in function that the treatment offers. We did find a good evidence of functional improvement when the scars treated were around joints or on mobile areas of the body. As an example, the treated patients did notice an improved movement of the neck when scars were treated on the neck or mandibular area. Similarly, some of our patients with scars on hands or wrists noticed an improvement in hand movement after treatment with fractional laser resurfacing. Any scoring system that addresses the issue of response assessment should ideally include this important variable as well wherever applicable.
CONCLUSIONS
Fractional laser resurfacing with CO2 laser offers a well-tolerated and effective treatment option in non-hypertrophic burn and traumatic scars. Scoring systems should be devised for assessing the therapeutic response in such scars which should ideally take into account all the variables of scar appearance and function.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Skin resurfacing of fine to deep rhytides using a char-free carbon dioxide laser in 47 patients. Dermatol Surg. 1995;21:940-6.
- [Google Scholar]
- Skin resurfacing with the Ultrapulse carbon dioxide laser: Observations on 100 patients. Dermatol Surg. 1995;21:1025-9.
- [Google Scholar]
- Treatment of facial rhytids with a nonablative laser: A clinical and histologic study. Dermatol Surg. 1999;25:440-4.
- [Google Scholar]
- Complications of carbon dioxide laser resurfacing: An evaluation of 500 patients. Dermatol Surg. 1998;24:315-20.
- [Google Scholar]
- The short- and long-term side effects of carbon dioxide laser resurfacing. Dermatol Surg. 1997;23:519-25.
- [Google Scholar]
- Single-pass CO2 laser skin resurfacing of light and dark skin: Extended experience with 52 patients. J Cosmet Laser Ther. 2003;5:39-42.
- [Google Scholar]
- Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-38.
- [Google Scholar]
- Fractional photothermolysis: A novel aesthetic laser surgery modality. Dermatol Surg. 2007;33:525-34.
- [Google Scholar]
- Side effects and complications of fractional laser photothermolysis: Experience with 961 treatments. Dermatol Surg. 2008;34:301-7.
- [Google Scholar]
- The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33:295-9.
- [Google Scholar]
- Clinical evaluation of the SmartSkin fractional laser for the treatment of photodamage and acne scars. J Drugs Dermatol. 2009;8(Suppl):s4-8.
- [Google Scholar]
- Fractional resurfacing for the treatment of atrophic facial acne scars in Asian skin. Dermatol Surg. 2009;35:826-32.
- [Google Scholar]
- Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40:381-6.
- [Google Scholar]
- Evaluation of a novel fractional resurfacing device for treatment of acne scarring. Lasers Surg Med. 2009;41:122-7.
- [Google Scholar]
- Fractional CO2 laser resurfacing as monotherapy in the treatment of atrophic acne scars. J Cutan Aesthet Surg. 2014;7:87-92.
- [Google Scholar]
- Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: Quantitative volumetric scar improvement. Arch Dermatol. 2010;146:133-40.
- [Google Scholar]
- Fractional nonablative 1540 nm laser resurfacing for thermal burn scars: A randomized controlled trial. Laser Surg Med. 2009;41:189-95.
- [Google Scholar]
- Fractional photothermolysis for the treatment of hypertrophic scars: Clinical experience of eight cases. Dermatol Surg. 2009;35:773-8.
- [Google Scholar]
- Non-ablative fractional resurfacing of surgical and post-traumatic scars. J Drugs Dermatol. 2009;8:998-1005.
- [Google Scholar]
- Ultrapulsed fractional CO2 laser for the treatment of post-traumatic and pathological scars. J Drugs Dermatol. 2010;9:1328-31.
- [Google Scholar]
- Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: Consensus report. JAMA Dermatol. 2014;150:187-93.
- [Google Scholar]
- Treatment of burn scar using a carbon dioxide fractional laser. J Drugs Dermatol. 2010;9:173-5.
- [Google Scholar]
- The efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patients. Dermatol Surg. 2009;35:1955-61.
- [Google Scholar]
- Evaluation of clinical results, histological architecture, and collagen expression following treatment of mature burn scars with a fractional carbon dioxide laser. JAMA Dermatol. 2013;149:50-7.
- [Google Scholar]
- Visual analogue scale scoring and ranking: A suitable and sensitive method for assessing scar quality? Plast Reconstr Surg. 2006;118:909-18.
- [Google Scholar]
- The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960-7.
- [Google Scholar]
- A new quantitative scale for clinical scar assessment. Plast Reconstr Surg. 1998;102:1954-61.
- [Google Scholar]
- How to assess postsurgical scars: A review of outcome measures. Disabil Rehabil. 2009;31:2055-63.
- [Google Scholar]






