Translate this page into:
Treatment of Postinflammatory Pigmentation Due to Acne with Q-Switched Neodymium-Doped Yttrium Aluminum Garnet In 78 Indian Cases
Address for correspondence: Dr. Vijay P. Zawar, 21 Shreeram Sankul, Opposite Hotel Panchavati, Vakilwadi, Nashik - 422 001, Maharashtra, India. E-mail: vijayzawar@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Postinflammatory hyperpigmentation (PIH) is a common sequela seen in the Indian population following affliction by acne. It is psychologically extremely disturbing for the patients and can severely affect the quality of life. Very few therapeutic modalities have proved to be really efficacious in this condition.
Aims:
The aim was to review our experience with 1,064-nm Q-switched neodymium-doped yttrium aluminum garnet (QSNY) laser in the treatment of PIH.
Materials and Methods:
Seventy-eight patients with postacne hyperpigmentation were included in the study. They were treated with six sessions at two weekly intervals using a 1,064-nm QSNY laser. Patient and physician scores were assessed at 1 month and 3 months after the last treatment. Clinical photographs also were reviewed to determine the efficacy. Adverse effects were noted.
Results:
Seventy percent of the patients reported significant improvement in hyperpigmentation as compared to the baseline. The majority of the adverse events were limited to mild, brief erythema.
Conclusion:
The 1,064-nm QSNY laser is an effective modality for the treatment of PIH caused by acne.
Keywords
Acne
hyperpigmentation
Q-switched neodymium-doped yttrium aluminum garnet (QSNY) laser
INTRODUCTION
Acne is a very common dermatological problem, especially in teenagers and also quite frequently in adults. Scarring and postinflammatory hyperpigmentation (PIH) are the two main complications of acne and are also the prominent reasons, which principally bring patients to a dermatologist. PIH occurs with higher frequency in Fitzpatrick skin types III-VI and though not life-threatening, it may cause significant distress to the patient.[1] Dermal hyperpigmentation can take years to fade to normal, while the epidermal variant can take up to 6-9 months. PIH is generally clinically apparent a few weeks after erythema from acne subsides. In severe cases, the patient may withdraw from group settings owing to the social stigma attached to this cosmetically displeasing condition.[2]
Many topical medications have been used for PIH, including keratolytics, retinoids, corticosteroids, and depigmenting agents. Although individual agents can be used with some success, the most significant improvement may be achieved with a combination therapy of topical medications and adjunctive dermatosurgical or cosmetological procedures. A few of the procedures available are chemical peeling with glycolic acid, salicylic acid, and trichloroacetic acid and laser modalities such as Q-switched (QS) ruby laser, Q-switched alexandrite laser, and Q-switched neodymium-doped yttrium aluminum garnet (QSNY) laser.
We wish to share our experience with the 1,064-nm QSNY laser in the treatment of acne-induced PIH.
MATERIALS AND METHODS
Seventy-eight patients, 65 females and 13 males aged between 18 years and 27 years and with Fitzpatrick skin types IV-VI were considered for the study. Inclusion criteria were all cases of persistent (unresponsive to various topical medications and lasting for 3 months or more) acne-induced PIH who were willing to undergo the procedure. Patients with pregnancy or planning for pregnancy, those with systemic diseases or other facial skin disorders, those who were lactating, had active acne lesions, on topical medications for the preceding 2 weeks, and on oral isotretinoin for the preceding 6 months were excluded from the study. A pretreatment history of the onset, duration of the condition, and response to previous medications was elicited. A detailed examination of postinflammatory pigmentation was carried out. Baseline pigmentation was assessed by photography and by patient and physician scores. Written consent was taken from all patients and they were explained about the risks, benefits, and potential complications of the laser therapy.
Topical anesthetic (lidocaine 2.5% and prilocaine 2.5%) was applied only in cases of anxious or pain-sensitive patients. Six treatments at two weekly intervals were administered to all patients using 1,064 Q-switched mode with 1.5-mm spot size, 2-Hz repetition rate, pulse width of 6 ns, and a fluence of 450 mJ in all sessions (Coherent medical system portable model, 2012, (Precise Co; Shanghai; supplied by Coherent, Mumbai, India)). Prilesional erythema with whitening of fine hair was considered as the end point. Immediately after the procedure, a combination of betamethasone and fucidic acid cream was applied to the irradiated areas for up to 3 days. Patients were advised to avoid direct sunlight and use sunscreen at least thrice a day. The immediate transient effects observed were stinging, erythema, edema, and punctate bleeding, which settled down in 1-2 days. In very few cases, mild crusting was noticed after 2-5 days, which cleared without any sequelae.
A blinded evaluator assessed the changes in the severity of pigmentation and the same evaluator was used at each session for a given patient. Improvement of PIH was graded on the following scale:
Score 1: None (0% improvement)
Score 2: Poor (1-24% improvement)
Score 3: Fair (25-49% improvement)
Score 4: Good (50-74% improvement)
Score 5: Excellent (75-100% improvement)
One and 3 months after the last treatment, participants and physicians were asked to rate the improvement in the same categories using the same scale. Clinical photographs were also reviewed to determine the efficacy. The Student's t-test (paired samples) was used to analyze the data.
RESULTS
A total of 78 patients participated in the study. There were 13 male (17%) and 65 female (83%) patients, with a mean age of 23 years (age range of 18-27 years). Out of 78 patients, five patients dropped out of the study after four sessions and the remaining completed all six sessions done twice weekly. The sessions were tolerated well by all the patients. Only one female patient exhibited transient confetti-like hypopigmentation, which recovered spontaneously within 10 days without any active intervention. There were no long-term adverse effects. The immediate cutaneous response was mild to moderate erythema and edema in all of the patients, which subsided in a couple of hours. Serial follow up photographs of a few patients are depicted in the pictures [Figures 1–3].

- (a) Before treatment of hyperpigmentation on the forehead of a male patient (b) Treatment with QSNY laser (c) Edema and erythema after 10 min (d) Significant lightening of pigmentation after three sittings (e) Complete resolution after six sittings

- (a) Before treatment of hyperpigmentation on the forehead of a female patient (b) Treatment with QSNY laser (c) Good reduction of pigmentation after three sittings (d) Significant lightening after six sittings
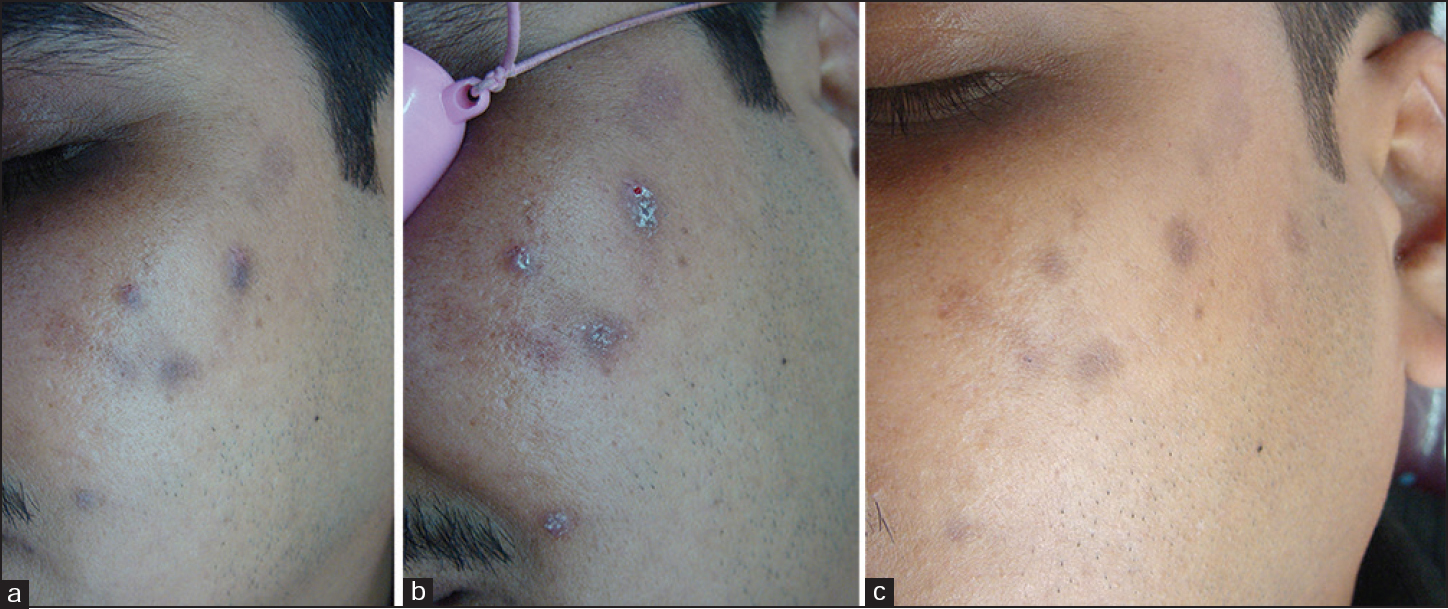
- (a) Before treatment of hyperpigmentation on the left malar area of a male patient (b) Immediately after treatment (c) Good reduction in pigmentation after three sittings
Assessment of blinded evaluator and pre- and postphotography revealed significant improvement in PIH [Tables 1 and 2].
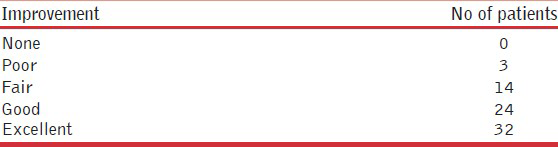
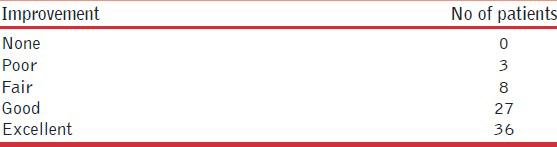
Patient satisfaction scores revealed that 56/73 (76.7%) patients had noticed good to excellent improvement. Only 3/73 (4.1%) patients felt that there was hardly any or poor improvement. The blinded evaluator scores revealed that 63/73 (86.7%) patients had good to excellent improvement while only 3/73 (4.1%) patients had hardly any or poor improvement. These values were found to be highly significant by paired t-test (P < 0.001).
DISCUSSION
PIH is a very common sequela of various inflammatory dermatoses and tends to affect darker skinned patients with greater frequency and severity. Acne is probably the most common cause of PIH in a skin of color.[3] Two major processes are involved in PIH. The first is pigment incontinence, which occurs after the basal cell layer in the inflamed skin is destroyed leading to accumulation of melanophages containing a large amount of melanin in the upper dermis. The other process involves an epidermal inflammatory response, resulting in the release and oxidation of arachidonic acid to prostaglandins and leukotrienes. These mediators stimulate increase in the synthesis of melanin in melanocytes and transfer of pigment to the surrounding keratinocytes.[4]
Epidermal hypermelanosis usually appears as tan, brown, or dark brown while dermal pigmentation has a blue-gray appearance. Most cases improve spontaneously; some take months or years to resolve and some remain permanent. Treatment may be prolonged, lasting for 6-12 months or longer for adequate restoration of normal pigmentation.
The primary treatment of acne is important in preventing any further hyperpigmentation or scarring. Photoprotection, including sunscreens, sun-protective clothing and hats, and sun avoidance, also helps to prevent any further increase in melanin production. Effective treatment strategies for acne PIH include using topical depigmenting agents for 3 months as first-line treatment. This can be followed by laser treatments such as 595-nm long-pulsed dye laser (LPDL) that targets any vascular inflammatory component. For recalcitrant dermal pigmentation, a longer wavelength pigment laser such as the 1,064-nm QSNY can be used.
First-line management of PIH includes topical tyrosinase inhibitors such as hydroquinone, kojic acid, azelaic acid, arbutin, licorice extracts, and others such as retinoid, ascorbic acid, niacinamide, and soy, along with a number of emerging therapies.
The role of laser treatment in PIH is usually reserved for lesions that remain refractory after several months of topical therapy. Lasers that have been mainly tried in PIH include Q-switched ruby laser, pulse dye laser, fractional CO2, QSNY, and the intense pulsed light. QSNY has been used in PIH previously with unsatisfactory results.[5]
The green (510-nm, 532-nm), red (694-nm), or near-infrared (755-nm, 1,064-nm) lasers are those which are pigment-specific and can selectively target intracellular melanosomes.[6] The problem with the pigmentary laser is that due to the wide absorption spectrum of melanin (250-1200 nm), laser energy that is intended for deeper targets can also be absorbed by the pigment in the pigmented epidermis, which can lead to complications such as dyschromia, blistering, and scars.
The 595-nm LPDL has been previously used in the treatment of acne-induced PIH. It probably works by treating the vascular component of inflammation.[7]
Nonablative fractional resurfacing has shown inconsistent results for the treatment of PIH. A previous study demonstrated transepidermal elimination of dermal component through incorporation into microscopic epidermal necrotic debris. The expulsion of dermal pigment in conjunction with the affected microthermal zones (MTZs) is the most likely mechanism of action when treating PIH. However, PIH itself is the most common adverse effect following this treatment.
Traditionally, the QSNY laser delivers pulses with durations in the nanosecond range, which are thought to generate acoustic waves within the biological tissue. With a longer wavelength, the 1,064-nm QSNY is used to target any dermal pigment, which may be too deep for topical agents to penetrate.
Cho et al. reported a good improvement in three patients of PIH treated with 1,064-nm QSNY laser at fluences of 1.9-2.6 J/cm2 and five sessions.[8] Ho et al. found good results with 1,064-nm QSNY (MedLite C3 or C6) where energy was 13-2.5 J/cm2, frequency was 10-Hz, and spot size was 6-8 mm in nine patients.[9]
Laser toning using low fluence, large spot size, multiple passes of 1,064-nm QSNY laser has also recently gained popularity in the treatment of PIH.[1011] Here, multiple passes of low-fluence (1.6-3.5 J /cm2) are delivered through a large spot size (6-8 mm) to optimize energy delivery and achieve mild erythema as the clinical endpoint. Daily usage or treatments at weekly, twice in a week, or monthly intervals with a wide variation in the total number of treatment is recommended.[12] In our study, we used 1,064 mode with 1.5-mm spot size, 2-Hz repetition rate, pulse width of 6 ns, and a fluence of 450 mJ in all sessions.
It was been proposed that 1064-nm QSNY laser can be used in PIH treatment at a low-fluence setting. Kim and Cho demonstrated effective treatment by full-face low-fluence 1,064-nm QSNY laser in acne PIH in skin photo types, fitzpatrick (SPTs) IV-VI patients.[13] In this study 1,064-nm QSNY laser treatment was found to be effective at treating PIH with statistical significance. The above studies have however, been conducted in smaller populations. Our study is one of the initial studies, which have demonstrated the efficacy of QSNY laser in acne PIH in a larger number of patients. In our study, 76% patients felt that they had good to excellent improvement while physician evaluation revealed that 86% patients had good to excellent improvement. These values suggest a significant improvement in PIH by using QSNY laser both statistically and clinically.
Confetti-like or spotty hypopigmented macules or punctate leukoderma and rebound hyperpigmentation are common side effects associated with low-fluence 1,064-nm QSNY laser. In our study, we did come across only one patient of transient hypopigmentation after sessions with QSNY laser, which recovered without any active treatment within 10 days.
Limitations
There was no control group as all our patients wanted some form of therapy. Therefore, further studies involving the control subjects are required to study the efficacy and safety of QSNY laser in PIH.
CONCLUSION
Management of long-lasting PIH due to acne is a psychological and cosmetic morbidity and it remains a challenge, especially in dark-skinned individuals. Although many treatment options are available for PIH, it takes months for PIH to resolve, even with an adequate therapy.
The advantages of QSNY are minimal downtime and absence of adverse effects such as bleeding and crust formation. Also, 1,064 nm being a longer wavelength penetrates deeper, thus leading to less paradoxical PIH with the treatment itself. More randomized controlled clinical studies in large numbers of PIH patients would be helpful in providing standardized measurable outcomes for this indication.
There is a sparse data in the Indian literature for treatment of acne PIH with QSNY laser and we did not find any recent literature in the Indian published reports. The authors found the QSNY laser to be a feasible, economic modality of treatment, which can be used optimally for the darker skin type with minimal adverse effects. We believe that QSNY may be considered as a viable option in cases of persistent PIH due to acne.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Common dermatologic disorders in skin of color: A comparative practice survey. Cutis. 2007;80:387-94.
- [Google Scholar]
- Postinflammatory hyperpigmentation: A common but troubling condition. Int J Dermatol. 2004;43:362-5.
- [Google Scholar]
- Managment of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg. 2009;28:77-85.
- [Google Scholar]
- Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J Dermatol Surg Oncol. 1994;20:592-7.
- [Google Scholar]
- Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63:274-83.
- [Google Scholar]
- Treatment of post-inflammatory hyperpigmentation using 1064-nm Q-switched Nd: YAG laser with low fluence: Report of three cases. J Eur Acad Dermatol Venereol. 2009;23:1026-7.
- [Google Scholar]
- A retrospective analysis of the management of acne post-inflammatory hyperpigmentation using topical treatment, laser treatment, or combination topical and laser treatments in oriental patients. Lasers Surg Med. 2011;43:1-7.
- [Google Scholar]
- Melasma treatment in Korean women using a 1064-nm Q-switched Nd:YAG laser with low pulse energy. Clin Exp Dermatol. 2009;34:e847-50.
- [Google Scholar]
- Low-fluence Q-switched neodymium-doped yttrium aluminum garnet laser for melasma with pre- or post-treatment triple combination cream. Dermatol Surg. 2010;36:909-18.
- [Google Scholar]
- A case series of facial depigmentation associated with low fluence Q-switched 1,064 nm Nd: YAG laser for skin rejuvenation and melasma. Lasers Surg Med. 2010;42:712-9.
- [Google Scholar]
- Treatment of facial postinflammatory hyperpigmentation with facial acne in Asian patients using a Q-switched neodymium-doped yttrium aluminum garnet laser. Dermatol Surg. 2010;36:1374-80.
- [Google Scholar]






