Translate this page into:
Complications of skin biopsy
Address for correspondence: Dr. Kumar Abhishek, Department of Dermatology, Vardhman Mahavir Medical College (VMMC) and Safdarjung Hospital, New Delhi - 110 029, India. E-mail: kumar.abhisek72@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Skin biopsy is the most commonly performed procedure by the dermatologist. Though it is a safe and easy procedure yet complications may arise. Post operative complications like wound infection and bleeding may occur. It is essential to keep the potential complications of skin biopsy in mind and be meticulous in the technique, for better patient outcomes.
Keywords
Anesthesia
bleeding
complications
infection
skin biopsy
INTRODUCTION
Skin biopsy is the most common and also the most essential procedure performed by a dermatologist in day-to-day practice. It is safe and easy, with not only diagnostic purpose, but also has significant therapeutic value. It is performed as an office procedure both on an outpatient and inpatient basis. Though it is one of the simplest procedures to perform, occasionally we come across complications related to skin biopsy. In a study conducted by Wahie, 29% of the patients on whom skin biopsy was performed, developed wound complications.[1] Hence it is important to know the possible risk factors and complications associated with skin biopsy and how to manage them.
CLASSIFICATION
Complications associated with skin biopsy are summarized in: [Table 1]
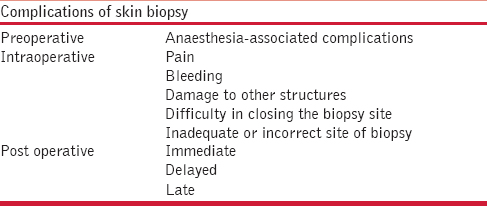
-
Preoperative.
-
Intraoperative.
-
Postoperative — immediate, delayed, late.
Preoperative
Anaesthesia-associated complications
Anaphylaxis: Anaphylaxis can be one of the many possible complications associated with local anesthesia. True type I hypersensitivity reaction to local anesthesia, injectable or topical, particularly to the amide group is very rarely seen. Reaction to the additives often masks the true incidence of hypersensitivity of the anesthetic. For this reason, it is suitable to perform intradermal test prior to performing the biopsy. If topical anesthesia is being used, then patch test can be performed in suspected cases.
Other complications
If a large volume is injected or injected in a blood vessel, complications can occur. Nausea, vomiting, dizziness, mild bruising, irritation, confusion, seizures, and blurred vision are the other complications, though all these are rarely seen. Local anesthetic with adrenaline should be used with caution in patients taking beta blockers, tricyclic antidepressants and monoamine oxidase inhibitors to avoid the risk of severe hypertension. It is advisable to always aspirate before injecting to rule out intravascular location of the needle and inject slowly.
Vasovagal attack is common, particularly in anxious patients and those with unstable autonomic nervous system. It is advisable to ask for any history of syncopal attacks before administering anaesthesia. It can be managed by raising the foot end of the bed. Injection atropine may be used in patients who develop bradycardia.[2]
Intraoperative
Pain
Mild pain is usually experienced during skin biopsy. Severity of pain may vary according to the site where biopsy is being performed. Occasionally pain can be more severe if there is:
-
Inadequate local anesthetic injection.
-
Short time gap between injecting the anesthesia and performing the procedure.
-
Wrong site of application of anesthesia.
-
Inadequate depth of applying anesthesia.
Bleeding
This is the commonest complication during skin biopsy but can rarely be life-threatening in a few circumstances. Usually in a normal individual, hemostasis is achieved soon after performing biopsy on the application of pressure. Co-administration of adrenaline with local anesthetic also helps in minimizing bleeding.[3] But in rare circumstances, it can be severe and pose challenges to the dermatologist in the following circumstances:
-
Underlying bleeding and clotting disorders - low platelet count, low clotting factors (as occurs in liver failure), hemophilia, von Willebrand disease.
-
Intake of drugs such as aspirin, clopidogrel, heparin, and dipyridamole.
-
Use of over-the-counter preparations such as fish oil, garlic, ginko, ginseng, vitamin E, Dong quai, feverfew, resveratrol.
-
Surgical sites such as the genitals, face, and scalp.
How to manage bleeding
Do not panic. Put pressure at least three times the bleeding time of the patient. If the bleeding continues, the vessel should be identified, clamped and then cauterised or ligated. Rarely hemostatic gels are required. It is important to control the bleeding, because it can increase the risk of infection, cause edema and pain and delay wound healing.
Damage to other structures
Damage to other structures such as nerves and vessels are rarely observed complications during skin biopsy. A biopsy in the preauricular area can rarely damage the facial nerve as the branches are very superficial. It can lead to small areas of sensory loss, paraesthesia or burning neuropathic pain.
Postoperative
Immediate
Pain, bleeding, swelling and tenderness may be observed.
Delayed
Wound infection is the most common complication associated with skin biopsy as per the study conducted by Wahie{!}. Out of the 100 diagnostic biopsies performed, 22 wounds demonstrated clinical signs of infection alone, 2 of dehiscence alone, and 5 had signs of both infection and dehiscence. In the 27 cases in which infection was clinically evident, the most common bacterium isolated from the wound swabs was Staphylococcus aureus. Four patients were found to have methicillin-resistant Staphylococcus Aureus (MRSA) positivity in wound swab culture.[1] Sites such as the skin folds, armpit, groin and lower legs are more prone to infection.
Wound dehiscence can be sequelae to wound infection or poor suturing of the wound.
Risk factors for wound infection include:
-
Underlying immunosuppressed state.
-
Diabetes mellitus.
-
Use of unsterile biopsy instruments or sutures.
-
Inadequate or no antibiotic coverage after the procedure.
Late
“Scarring” with or without hypo- or hyperpigmentation is a common complication seen after healing of the skin biopsy site [Figure 1]. Hypopigmented scars are common when biopsies are taken for hyperpigmented lesions. Scars can be atrophic scar or hypertrophic. Occasionally, patients may develop a keloid over the biopsy site. Contact dermatitis due to the antiseptics used such as povidone-iodine or hexidine can occur.

- Persistent hypopigmented scar in the periorbital region following a 3mm punch skin biopsy
Complications of skin biopsy at special sites or special lesions
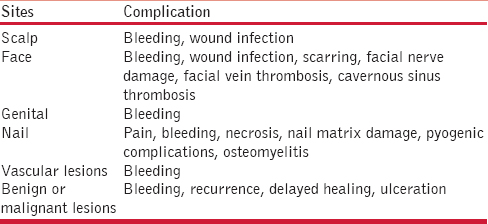
The most common complication of skin biopsy at special sites such as the scalp, face, or nails is bleeding. Pain and wound infections can occur, while, cavernous sinus thrombosis is extremely rare from facial biopsies. [Table 2].
Prevention of complications
In order to prevent or reduce complications it is necessary to take complete history and physical examination before performing a skin biopsy. A detailed history with regard to medications that can cause prolonged bleeding, increase risk of infection or delay healing should be actively sought. The site of biopsy should be properly planned which represents the index lesion and the depth and size of the specimen should be adequate. In an excisional biopsy, the incision should be along the relaxed skin tension lines to give a good cosmetic scar. The biopsy should be done meticulously with strict aseptic precautions. Post operative instructions should be clearly discussed with the patient.
CONCLUSION
Skin biopsy is the most important diagnostic procedure for a dermatologist. However, awareness about the possible complications that can arise due to this small procedure helps in better outcome for the patients and less hassles for the dermatologist.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Wound complications following diagnostic skin biopsies in dermatology inpatients. Arch Dermatol. 2007;143:1267-71.
- [Google Scholar]
- Guidelines for administration of local anaesthesia for dermatosurgery and cosmetic dermatology procedures. Indian J Dermatol Venereol Leprol. 2009;75(Suppl S2):68-75.
- [Google Scholar]
- Techniques of skin biopsy and practical considerations. J Cutan Aesthet Surg. 2008;1:107-11.
- [Google Scholar]






