Translate this page into:
Glove Puncture During Liposuction: A Report of Two Cases
Address for correspondence: Dr. S S Shirol, Cosmetic & Plastic Surgeon, Sampige Superspeciality Clinic, 1st floor Diwate Complex, Opposite Vasan Eye Care, Near Court Circle, Hubli 580028, Karnataka, India. E-mail: ssshirol@yahoo.co.uk
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Gloves are to surgeons what shields are to soldiers. Glove injuries are known to occur commonly in any surgical procedure, ranging from major surgeries to minor surgical procedures. The incidence of glove injury ranges from 10% in ophthalmologic surgeries to as high as 50% in general surgery.[1] Among the plastic surgery procedures, the incidence of glove perforation was found to be 1.02% after minor surgery and 21.40% after major surgery. The most common location of perforations was found to be the palmar surface of the left hand in both groups.[2]
But there has been no published report of glove perforation occurring during liposuction till date. Hence, we report two cases of glove perforation occurring during liposuction for gynecomastia, with probable mechanism of injury and possible methods of prevention.
CASE 1
A 29-year-old male with bilateral gynecomastia was treated with liposuction and surgical excision of the gland. Liposuction was done using the tumescent technique with a 3 mm cannula. As the liposuction proceeded toward the subareolar/subglandular area, there was accidental glove puncture on the left index finger (nondominant hand) [Figure 1a and b].

- (a) The technique of guiding the cannula that may cause injury to the nondominant index finger (b) The glove puncture on index finger
CASE 2
A 25-year-old male with gynecomastia was treated with liposuction and surgical excision of the gland. In this case, we modified the technique of liposuction to stabilize the liposuction cannula with the left hand [Figure 2a] to avoid glove injury to the left index finger. This time, liposuction of the subareolar area caused injury to the thenar aspect of the left (nondominant) hand [Figure 2b].
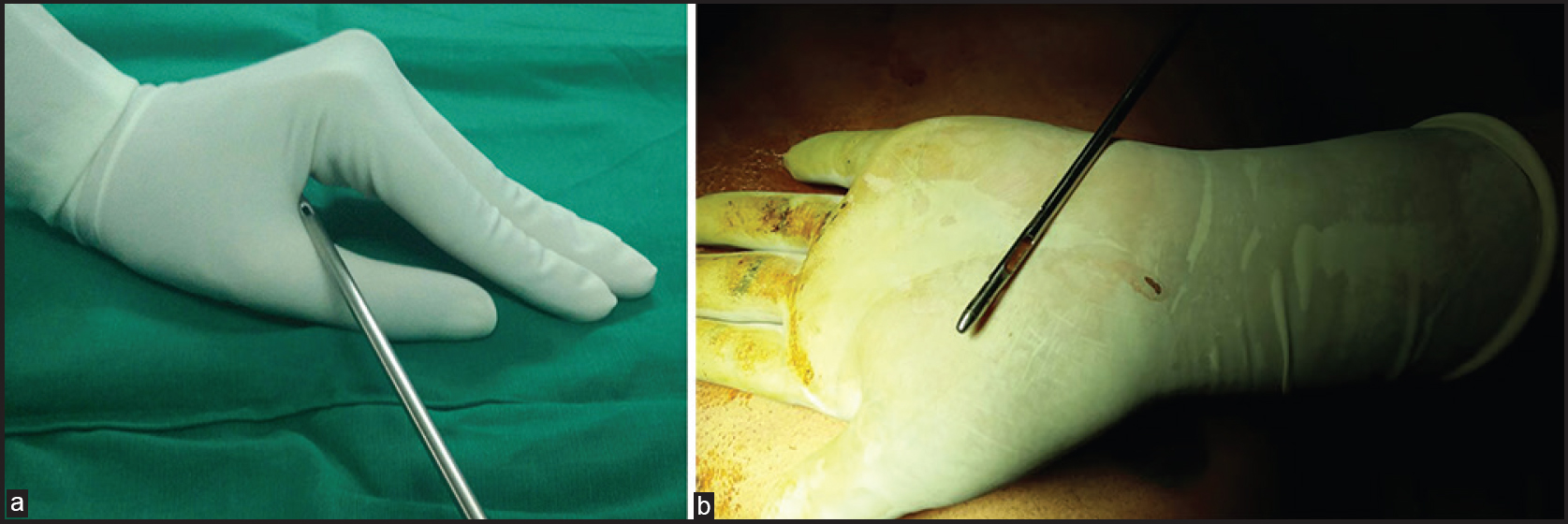
- (a) The technique of guiding the cannula that seems to cause puncture on the thenar aspect of the nondominant hand (b) Glove injury on the thenar aspect of the nondominant hand
The mechanism of glove puncture during liposuction seems different and is instrument and technique-related.
In suction-assisted liposuction (SAL) blunt-tipped hollow cannula of various designs with variations in size and location of the holes are used [Figure 3]. Liposuction for gynecomastia is performed by placing the nondominant hand over the breast tissue to guide the cannula, while the cannula is held in the dominant hand and moved in a forward and backward motion.

- Various sizes and number of holes at the tip of liposuction cannula
As the liposuction proceeds close to the incision site, the holes in the cannula are likely to come in close proximity to the surface of the glove over the index finger of the supporting left hand and the negative suction pressure is likely to act on the surface of the glove causing accidental puncture in the glove. Another likely mechanism contributing to the glove puncture is the thermal injury caused by the friction developed between the gloved finger and the cannula during continuous to-and-fro movements. Both these mechanisms are likely to act independently or in combination to cause a glove perforation.
The incidence of glove perforation is, in addition, related to the duration of wear during surgery. It has been found that wearing gloves for 90 min or less caused glove punctures in 15.4% of gloves, whereas the use of gloves for 91-150 min caused glove injuries in 18.1% of gloves, and wearing gloves for more than 150 min resulted in perforations in 23.7% of gloves.[3]
We recommend a change in the design of the standard liposuction cannula, wherein a single hole closer to the tip of the cannula would prevent the glove coming in contact with the negative pressure of the cannula. This cannula can be selectively used during subareolar liposuction in gynecomastia and liposuction around the incision site in other cases.
Anterior axillary incision for liposuction of subglandular liposuction would prevent accidental exit of the holes in the cannula and, hence, avoid glove puncture.
Another simple way of prevention is the use of double gloves during the procedure. It decreases the tactile sensations of the operating surgeon and it has an important role in any plastic surgical procedure. Cole et al. report that the use of double gloves reduces the incidence of glove perforation from 21.5% to 9% during plastic surgical procedures.[4] Bertolin et al. recommend that plastic surgeons must balance the improved security of double gloving with possible discomfort or reduced sensitivity.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Glove punctures in major and minor orthopaedic surgery with double gloving. Acta Orthop Belg. 2007;73:760-4.
- [Google Scholar]
- Risk of glove perforation in minor and major plastic surgery procedures. Aesthetic Plast Surg. 2003;27:481-4.
- [Google Scholar]
- Incidence of microperforation for surgical gloves depends on duration of wear. Infect Control Hosp Epidemiol. 2009;30:409-14.
- [Google Scholar]
- Does double gloving protect surgical staff from skin contamination during plastic surgery? Plast Reconstr Surg. 1997;99:956-60.
- [Google Scholar]





