Translate this page into:
Evaluation of Various Therapeutic Measures in Striae Rubra
Address for correspondence: Dr. Bela Bhemabhai Padhiar, Plot No. 255/A, Sector-20, Gandhinagar, Gujarat, India. E-mail: drbelapadhiar@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Striae are linear atrophic depressions that form in areas of dermal damage in the skin. As on date, no consensus or protocol exists for the treatment of stria rubra. Topical retinoids, chemical peels, microdermabrasion, radiofrequency, photothermolysis, intense pulsed light and lasers are some of the modalities used.
Aims and Objective:
To compare the efficacy of various therapeutic modalities in striae rubra.
Methods:
This prospective cohort study comprised of a total of fifty patients from August-2012 to October-2013 in a tertiary care center in Western India, Gujarat having striae rubra. They were randomly divided into five groups of ten patients each. Patients were evaluated on the basis of visual assessment, both by doctor as well as the patient. Group I was given topical tretinoin (0.1% w/w) gel applied once at night, Group II-microdermabrasion (MDA) combined with trichloroacetic acid (TCA) (30%) peel, Group III-mesotherapy, Group IV-Q-switched Nd: YAG laser, and Group V-combination treatment of microdermabrasion, salicylic acid peel and retinol (yellow) peel. Patients were treated at an interval of 15 days for 2 months and then at monthly intervals. Objective assessment was done at 2nd month, 6th month, and at the end of 1st year.
Results:
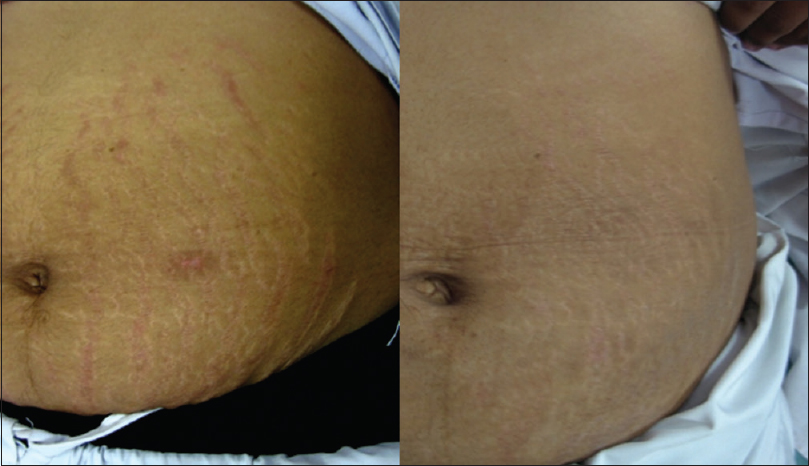
Patients in Group I treated with topical tretinoin showed the least response with 80% (8) of them showing minimal clinical improvement (0–25%) as compared to patients in Group V in which 60% (6) patients showed moderate clinical improvement (50–75%). While majority of the patients in Group II, III, and IV showed mild clinical improvement (25–50%).
Conclusions:
Striae rubra is a common cause of concern for adolescent population. Combination treatment with microdermabrasion, salicylic acid and retinol yellow peel gave superior results as compared to other therapeutic options. Mild to moderate improvement was seen with Nd: YAG laser, mesotherapy and MDA + TCA whereas minimal improvement were seen with topical tretinoin.
Keywords
Mesotherapy
microdermabrasion
Q-switched Nd: YAG laser
striae rubra
topical tretinoin
retinol yellow peel
INTRODUCTION
Dermatology has always been to some extent a blend of disease and desire treatment. Moreover, with the increasing concerns for scars and blemishes, we cannot overlook the importance of striae.
Striae are linear atrophic depressions of the skin that form in areas of dermal damage produced by stretching of the skin. Etiopathogenesis of stria is poorly understood, though it is frequently associated with various physiologic states, including puberty, pregnancy, growth spurts, rapid weight gain, or loss and obesity.[1]
They can also be seen as cutaneous manifestation of Cushing's syndrome, Marfan's syndrome and as adverse effect of oral and topical corticosteroids.[23]
As on date, no consensus or protocol exists for the treatment of stria rubra. The available modalities are moisturizing oil with Vitamin E and C, topical retinoids, chemical peel like trichloroacetic acid (TCA), salicylic acid peel, microdermabrasion (MDA), radiofrequency, photothermolysis, intense pulsed light and lasers such as 585 nm pulsed dye laser, Q-switched Nd: YAG laser and fractional lasers.[4] But still it remains an important area of research. Therefore, the aim of this study was to compare the efficacy of various therapeutic modalities in striae rubra.
Epidemiology
Striae affect women more commonly than men. Approximately, 90% of pregnant women, 70% of adolescent females, and 40% of adolescent males (many of whom participate in sports) have stretch marks. They affect persons of all races. Striae are usually a cosmetic problem; however, if extensive, they may tear and ulcerate when an accident or excessive stretching occurs.
METHODS
This prospective cohort study was conducted in the department of dermatology for 1 year from August 2012 to October 2013. Fifty volunteers (Fitzpatrick skin types IV–VI) aged between 20 and 40 years with striae rubra were enrolled and written informed consent to participate in the trial was obtained from each patient. This study was approved by Institutional Ethics Committee. The duration of striae ranged from 4 months to 12 years. Lesions were located on the abdomen, shoulders, and buttocks.
Exclusion criteria included a history of keloidal tendency, herpes labialis, and koebnerization, pregnancy, patients with unrealistic expectations and patients not willing to give written informed consent.
These fifty patients were randomly and equally divided into five groups. Group I was treated with topical tretinoin (0.1% w/w) gel applied once at night.
Group II included patients who were treated with aluminum oxide crystal microdermabrasion. Erythema was considered as the end point of the procedure followed by application of 35% trichloroacetic acid peel followed by cold saline application after the appearance of frosting.
Patients in group III were treated with mesotherapy where in meso HSR (Hyaluronic acid skin rejuvenating) solution was introduced using a mesogun.
In Group IV patients were treated with Q- Switched ND-YAG Laser 1064 nm (MedLite C6) with a spot size of 4 mm, fluences between 2 -9 J/cm2, frequency of 2.00 HZ. Fluence was increased at every sitting as per patient tolerance. 1064 nm.
Patients in Group V were treated with combination therapy of MDA followed by 30% salicylic acid peel, till pseudofrosting appeared followed by massage with combination cream containing 4% retinol, 1% retinyl, 10% ascorbic acid, 5% niacinamide, and kept under occlusion for 8 h.
Patients were followed up fortnightly for 3 months and then monthly for a year. The response was documented through sequential digital photography obtained at baseline, pre- and post-each treatment session. Two blinded dermatologists then made clinical assessments by evaluating the photographs according to evaluation scale. Efficacy of treatment was graded on a quartile grading scale based on Physician's Global Assessment with <25% being graded as poor response, 25–50% as mild improvement, 50–75% as moderate improvement and >75% improvement labeled as excellent response.
RESULTS
Most of the patients included in the study were of age group 20–40 years and majority of them were females.
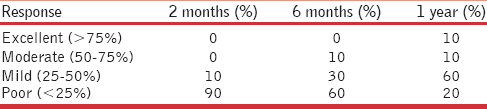
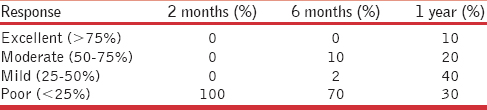
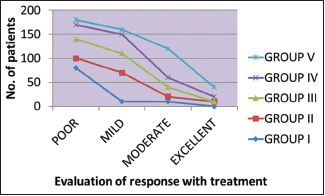
In Group I treated with topical tretinoin, 80% (n = 8) of patients showed poor response at the end of 1 year whereas 10% (n = 1) had mild and moderate response [Table 1 and Figure 1].

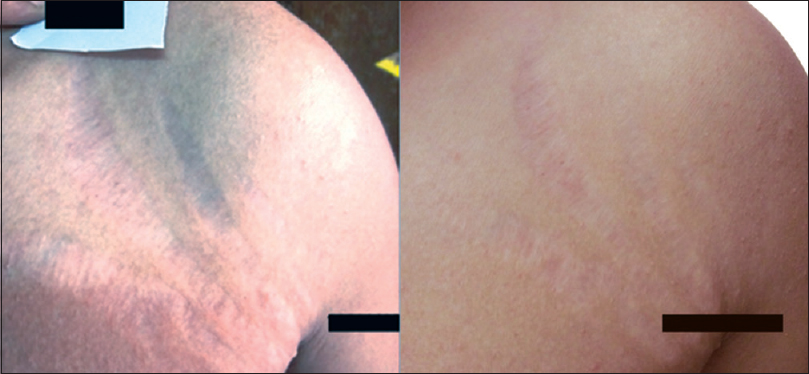
- Pre- and post-treatment photograph of a patient treated with topical tretinoin (0.1%)
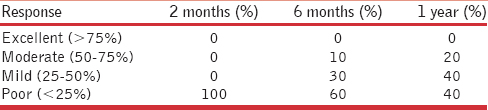
In Group II treated with MDA and TCA peel 60% (n = 6) patient showed mild improvement whereas 10% (n = 1) showed moderate and excellent response [Table 2 and Figure 2].
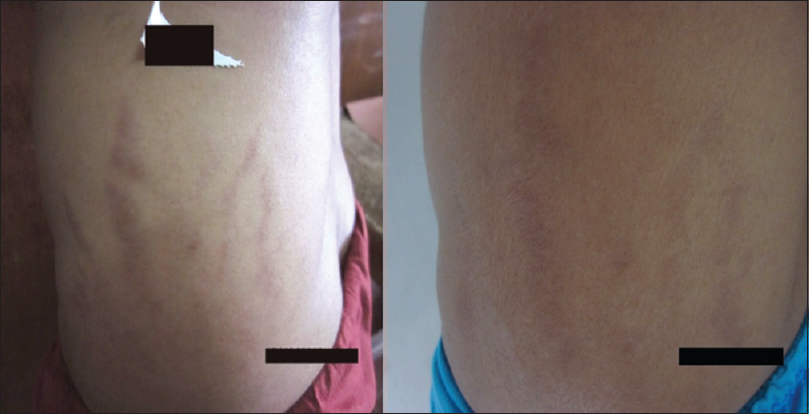
- Pre- and post-treatment photograph of a patient treated with microdermabrasion and trichloroacetic acid peel 35%
In patients in Group III who were treated with mesotherapy 25–50% improvement was seen in 40% of patients at the end of 1 year [Table 3 and Figure 3].

- Pre- and post-treatment photograph of a patient treated with intradermal mesotherapy hyaluronic acid solution
In group IV treated with laser, 40% patient had 25–50% improvement whereas 20% showed moderate response [Table 4 and Figure 4].

- Pre- and post-treatment photograph of a patient treated with laser Q-switched Nd: YAG laser 1064 nm
In group V, patients treated with combination therapy, 20% of patients had >75% improvement with 60% of patient showing 50–75% improvement in stria with only 10% showing a mild and poor response at the end of 1 year [Table 5 and Figure 5].
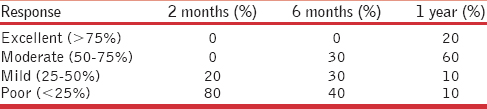
- Pre- and post-treatment photograph of a patient treated with combination therapy in group V
No side effects were observed with various therapeutic modalities in striae rubra in the present study [Graph 1].
- Overview of response with all modalities of treatment
DISCUSSION
Striae are a very common condition in all age groups. They commonly develop during puberty, with an overall incidence of 25–35%,[5] or during pregnancy, with an incidence of approximately 75%.[6] Striae distensae are a reflection of “breaks” in the connective tissue that lead to dermal atrophy. The exact etiology still remains controversial, and this is partly due to the variability in the clinical situations in which striae arise. A genetic predisposition is presumed, striae distensae have been reported in monozygotic twins. There is decreased expression of collagen and fibronectin genes in affected tissue.
All-trans-retinol is the natural alcohol form of Vitamin A. Tretinoin has been shown to improve the clinical appearance of stretch marks during the active stage (striae rubra), although with not much effect during the mature stage (striae alba). There are data to suggest that medical therapy may be useful in early cases[7] tretinoin 0.1%, silicone gels, cocoa butter, and Centella asiatica have some data to recommend their use.[8]
Al-Himdani et al., in a recent publication, correctly identified that no high-quality, randomized controlled trials evaluating treatments for striae distensae exist.[8]
Topical application of tretinoin has been shown to significantly improve the clinical appearance of early striae distensae (striae rubra).[910] One of the most pronounced effects of all-trans retinoic acid treatment on the skin is on epidermal hyperplasia. For thin, atrophic or photodamaged epidermis, the effect of retinoid is to cause epidermal thickening or hyperplasia. In hypertrophic skin such as in actinic keratoses, the net effect is normalization of epidermal thickness. Hyaluronic acid production is also stimulated by it. There is increased production of an epidermal ground substance which binds water leading to increased epidermal hydration.
Aluminum oxide resurfacing has become a popular method of resurfacing. MDA is effective in many skin conditions such as acne scars, mottled pigmentation, and fine wrinkles. It has been established too that MDA induces epidermal signal transduction pathways that are associated with remodeling of the dermal matrix. It produces epidermal and dermal changes through superficial wounding.
Mesotherapy refers to a minimally invasive intradermal technique which consists of the use of intra- or subcutaneous injections containing mixture of compounds to treat local medical and cosmetic conditions. It involves injecting micro quantities of hyaluronic acid intraepidermally, at dermoepidermal junction or into deep dermis. Bruising and edema can occur due to inflammatory response provoked by some of the chemicals used in mesotherapy. Of the many modalities used to ameliorate and improve stretch marks, lasers have recently become a popular therapeutic alternative. The Q-switched 1064 nm lasers employ an optomechanical shutter allowing for nanosecond delivery of laser pulses at 1064 nm wavelength. The mechanism for dermal remodeling of stretch marks is a combination of photoacoustic effects and absorption by water leading to dermal collagen remodeling. This is the safest laser in darker skin tones and does not require contact cooling. Lower fluencies are indicated for stretch marks and scarring. Five to seven treatment sessions spaced 4–6 weeks apart are necessary. In another study involving the use of a 1064-nm long-pulsed Nd: YAG laser, the authors reported subjective data (55% of patients reported excellent improvement), and objective photographic findings (40% of evaluating physicians reported excellent improvement). Minimal adverse effects were reported.[11]
TCA (10–35%) has been used for many years and is safe to use at low concentrations. At higher concentration (e.g., >50%), TCA has a tendency to scar. Some authors have had good success using low concentrations (15–20%) of TCA[12] and performing repetitive papillary dermis level chemexfoliation repeated at monthly interval with reported improvement in texture and color of stretch marks.
Yellow peel procedure can be used as a peeling agent for medium depth peels. It uses salicylic acid, retinol, retinyl palmitate, lactic acid, ascorbyl glucoside, and niacinamide. Ten percent ascorbyl glucoside is a form of Vitamin C combined with glucose. It is essential cofactor for lysyl and prolyl hydroxylase required for posttranslational processing in collagen (type I and III) biosynthesis. Niacinamide leads to increase in dermal matrix content via elevated collagen synthesis and other matrix proteins. Lactic acid is an alpha hydroxyl acid and has a role in hydration of skin.
CONCLUSION
From this study, we can conclude that stria rubra is a common cause of concern for the adolescent population. Minimal improvement was seen with topical tretinoin. Mild to moderate improvement was seen with Nd: YAG laser, mesotherapy, and MDA + TCA. None of the treatment modalities used alone gave a good response, so we tried combination therapy which gave superior results.
Combining the disease and desire aspects will require integration on many levels and so the therapy for stria still remains elusive.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The cause of striae distensae. Acta Derm Venereol (Stockh). 1979;59(Suppl 85):161-9.
- [Google Scholar]
- Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet. 1996;62:417-26.
- [Google Scholar]
- Striae distensae (stretch marks) and different modalities of therapy: An update. Dermatol Surg. 2009;35:563-73.
- [Google Scholar]
- Physiologic skin changes during pregnancy: A study of 140 cases. Int J Dermatol. 1998;37:429-31.
- [Google Scholar]
- Striae. In: Lebwohl MG, Warren RH, Berth-Hones J, Coulson I, eds. Treatment of Skin Disease Comprehensive Therapeutic Strategies (4th ed). United States: Saunders, Elsevier Limited; 2014.
- [Google Scholar]
- Striae distensae: A comprehensive review and evidence-based evaluation of prophylaxis and treatment. Br J Dermatol. 2014;170:527-47.
- [Google Scholar]
- Topical tretinoin (retinoic acid) improves early stretch marks. Arch Dermatol. 1996;132:519-26.
- [Google Scholar]
- Stretch marks: Treatment using the 1,064-nm Nd: YAG laser. Dermatol Surg. 2008;34:686-91.
- [Google Scholar]
- TCA-based blue peel: A standardized procedure with depth control. Dermatol Surg. 1999;25:773-80.
- [Google Scholar]






