Translate this page into:
Observations on CO2 Laser Preparation of Recipient Site for Noncultured Cell Suspension Transplantation in Vitiligo
Address for correspondence: Dr. Lisa Komen, The Netherlands Institute for Pigment Disorders, Meibergdreef 9, 1105 AZ, Amsterdam, The Netherlands. E-mail: l.komen@amc.uva.nl
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
With interest, we read the review of Al-Hadidi et al. on the role of recipient site preparation techniques in the surgical management of vitiligo.[1] We agree with the conclusion that lasers are effective and valuable tools in the preparation of recipient sites. However, optimal laser settings and ablation depth are not known. We present two vitiligo patients where we observed that more superficial ablation of the recipient site in combination with noncultured autologous cell suspension transplantation (CST) can also be effective. We treated a 33-year-old woman (patient 1) and a 74-year-old man (patient 2), with stable nonsegmental vitiligo lesions on the legs. The cellular suspension was processed from a 1 cm × 1.5 cm to 0.2–0.3 mm thick split-thickness biopsy using a ReCell® kit[2] (Avita Medical, Cambridge, UK). The recipient site was prepared with a 10,600 nm CO2 laser (Ultrapulse Encore, Active FX scanner, Lumenis, Santa Clara, CA, USA). In both patients, a first treatment site was prepared with 1 pass (200 mJ, 60 W, density 3, estimated depth of 209 microns), and a second treatment site with an additional pass (100 mJ, 60 W, density 3, estimated depth of 300 microns). Table 1 shows erythema, reepithelialization, and repigmentation of the treatment sites. Erythema resolved faster in both patients in the least invasive setting. Reepithelialization was quicker in the least invasive setting in one patient. The different laser settings in combination with CST showed similar repigmentation, i.e., 90% and 75% repigmentation in both patients, respectively, after 6 and 15 months. Patient 1 and 2 [Figures 1 and 2] mentioned pain for 5–14 days after transplantation, without being able to assess a difference in pain between the sites.

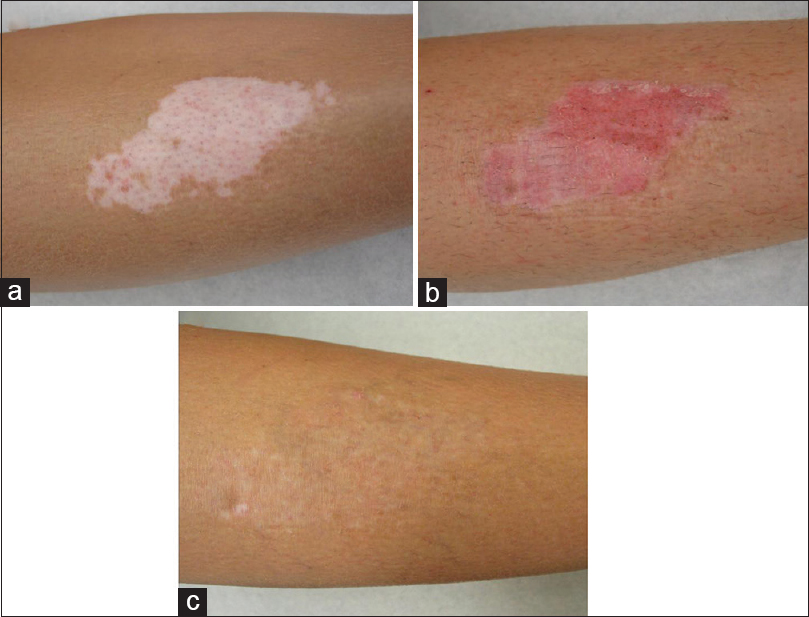
- The photographs show the treated lesion on the right leg in patient 1 before treatment (a), 2 weeks after treatment (b), and 6 months after treatment (c). The lower part of the lesion was treated with 200 mJ, 60 W, density 3 with 1 pass (treatment site I) and the upper part of the lesion with an additional pass with 100 mJ, 60 W, density 3; full ablation (treatment site II). 6 months after treatment (c) the treated lesion was 90% repigmented with color and texture matching the surrounding skin
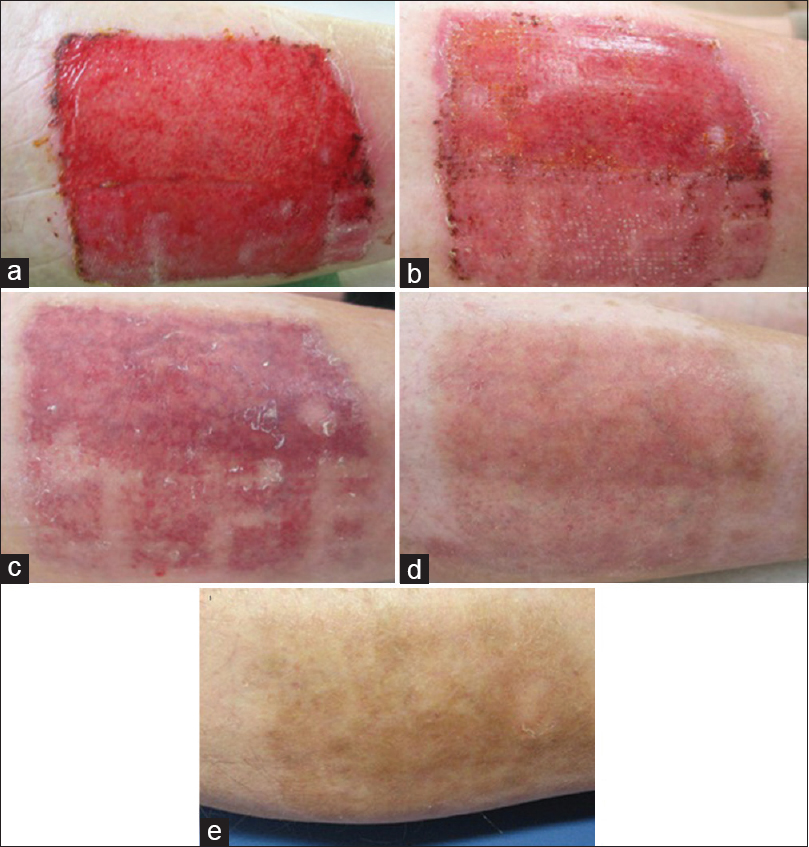
- The photographs show the treated lesion on the right leg in patient 2, 1 week (a), 2 weeks (b), 8 weeks (c), 6 months (d), and 15 months after treatment (e). The lower part of the lesion was treated with 200 mJ 60 W, density 3 with 1 pulse (treatment site I) and the upper part of the lesion with an additional pass with 100 mJ, 60 W, density 3; full ablation (treatment site II). Erythema was long lasting in treatment site II and healing took longer (a and b). After 15 months, both treated lesions are 75% repigmented with hyperpigmentation compared to the surrounding skin. Erythema was no longer seen (e)
On the one hand, laser settings to prepare recipient sites have to be of sufficient depth to make graft take possible. This is hypothesized to be at the papillary dermis and differs per body part.[3] On the other hand, these laser settings should be as less invasive as possible to allow rapid wound healing and prevent side effects. In CO2 laser resurfacing, the safety endpoint is the appearance of a “chamois” yellow skin color, which is seen at the reticular dermis.[4] The occurrence of pinpoint bleeding, seen at the dermoepidermal junction, has been advocated as immediate clinical endpoint in CST when using dermabrasion.[25] This endpoint is affected by many factors and may therefore not be a reliable and reproducible clinical sign to predict the appropriate depth of ablation when using a laser.
In conclusion, these cases suggest that less invasive CO2 laser treatment in combination with CST could be as effective as and potentially safer than more invasive treatment. There is no optimal clinical endpoint for the ablation depth of the recipient site when using a CO2 laser. Further investigations on the laser settings are required before conclusions can be drawn. Furthermore, less invasive laser treatment such as more superficial ablative laser or fractional laser should be studied in combination with CST to obtain optimal treatment results with minimal side effects in the future.
Financial support and sponsorship
The ReCell kits were provided free of charge by Avita Medical.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Role of recipient-site preparation techniques and post-operative wound dressing in the surgical management of vitiligo. J Cutan Aesthet Surg. 2015;8:79-87.
- [Google Scholar]
- Treatment of vitiligo lesions by ReCell vs. conventional melanocyte-keratinocyte transplantation: A pilot study. Br J Dermatol. 2008;158:45-9.
- [Google Scholar]
- Double-blind placebo-controlled study of autologous transplanted epidermal cell suspensions for repigmenting vitiligo. Arch Dermatol. 2004;140:1203-8.
- [Google Scholar]
- Treatment of upper- and lower-extremity vitiligo with epidermal grafts after CO2 laser resurfacing with systemic and topical steroids. Aesthetic Plast Surg. 2010;34:157-66.
- [Google Scholar]
- Long-term follow-up study of segmental and focal vitiligo treated by autologous, noncultured melanocyte-keratinocyte cell transplantation. Arch Dermatol. 2004;140:1211-5.
- [Google Scholar]





