Translate this page into:
Blepharoplasty Basics for the Dermatologist
Address for correspondence: Dr. Naresh Joshi, Department of Oculoplastics, Chelsea and Westminster Hospital, London, United Kingdom. E-mail: eyelidman@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Blepharoplasty is amongst the more frequently performed aesthetic procedures with surgery performed by physicians and surgeons across a variety of sub-specialities. This paper, aimed at a dermatology audience, describes patient selection, eyelid anatomy, clinical examination and surgical steps to achieve successful upper and lower lid blepharoplasty outcomes. Recommendations for minimising complications are made and photographs used to illustrate important clinical and surgical features.
Keywords
Aesthetic
blepharoplasty
cosmetic Surgery
Eyelid
oculoplastic
INTRODUCTION
Blepharoplasty may be performed on the upper or lower eyelids. In the upper eyelid can be both for functional as well as aesthetic reasons. The American Society of Aesthetic Surgeons reported approximately 165,000 blepharoplasty surgeries were performed in 2014, making it the fourth most common aesthetic procedure in the USA.[1] Before considering blepharoplasty, potential contraindications to surgery should be elucidated; these include patients with psychological issues, dry eyes, active inflammatory cicatrising skin conditions such as eczema and psoriasis and multi-revision surgeries.
CLINICAL EVALUATION
The upper lid and brow may be regarded as an aesthetic continuum, so the assessment for upper lid blepharoplasty should not only include the amount of redundant skin (dermatochalasis) and fat prolapse, but also an evaluation of the brow and lid margin position.[2]
Upper eyelid margin position is usually recorded as the distance in millimetres from the mid pupil position to the upper lid margin, known as the marginal reflex distance-1 (MRD-1).
Although no definitive numeric definition exists an eyelid with an MRD-1 of ≤2 mm may be considered ptotic.[3] Failure to exclude and address concurrent eye ptosis when performing upper lid blepharoplasty may result in disappointed patients.
Similarly, the brow position will influence apparent upper lid skin redundancy with an underlying brow ptosis exacerbating a patient's complaint of ‘eyelid hooding.’
Evidence for lateral brow descent following blepharoplasty reinforces the importance of recognising and managing an underlying brow ptosis. A patient undergoing upper lid blepharoplasty surgery can be pre-operatively counselled accordingly, and if necessary the brow ptosis addressed through a variety of surgical techniques, or non-surgical methods, such as botulinum toxin injection.[4] Brow ptosis correction is discussed in detail elsewhere in this issue.
UPPER LID SKIN MARKING
Fastidious pre-operative skin marking is crucial for successful outcomes. Our preference is to mark the skin crease and skin for excision in both the sitting and supine position.[4] The skin is cleaned with an alcohol wipe, dried and using a fine tipped marker the eyelid crease is marked sitting and supine. The crease is typically 9–11 mm above the lash line in females, 7–9 in men and may be 4–6 mm in Asian patients [Figure 1].[5]

- Demonstrates the upper lid skin crease, which may vary with gender, ethnicity and age. The lid crease is measured from the lid margin to the first skin fold
The marked lid creases should be measured and recorded ensuring symmetry between both sides. Fine non-toothed forceps grasp redundant skin above the crease to determine the upper incision line. This is repeated at three to four points along the eyelid crease to determine the optimum quantity and shape of skin excision. The lid margin position is carefully observed for stability during the pinch test. This protects against excessive skin excision post-operative lagophthalmos [Figure 2].

- Lid crease marking and ‘Pinch test’ to assess excess upper eyelid skin for excision. Note that there is no eyelash eversion or lagophthalmos
The upper lid possesses two fat pads, medial and central. If lateral fullness is noted, is likely to be related to lacrimal gland prolapse, and this can be treated with lacrimal gland repositioning.
There has been a temporal trend in aesthetic surgery literature towards greater fat and volume preservation.[6] In our practice targeted sculpting, principally of the medial orbital fat, can be aided by the pre-operative marking of the overlying skin. This is performed before anaesthetic infiltration to avoid subsequent tissue contour distortion. The medial fat pad has been shown to become more prominent relative its neighbouring central fat with advancing age, this may be secondary to their different embryological origins?[11]
SURGICAL TECHNIQUE UPPER LID BLEPHAROPLASTY
We utilise a rubber corneal shield in all eyelid procedures to avoid the risk of inadvertent cornea damage. Skin incisions are made using a Colorado microdissection needle (Stryker, Michigan, USA). The skin is first dissected off the underlying orbicularis muscle maintaining absolute haemostasis [Figure 3a]. Next, a strip of orbicularis, 30–50% of the skin excision height, is removed using the Colorado needle [Figure 3b]. The exception to this is in younger patients undergoing blepharoplasty, where little to no orbicularis excision is required. If lateral brow elevation is required, a broad, lateral wedge of orbicularis muscle is removed to weaken the lateral brow depressive forces.[7]
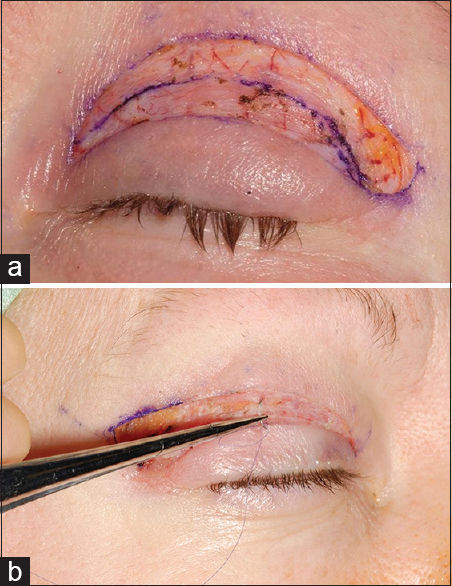
- (a) Demonstrates shape of blepharoplasty skin excision and the excision of selected orbicularis. Note the broader excision of orbicularis laterally with relative orbicularis preservation inferior – medially. (b) Closure of the upper lid skin incision demonstrating tissue bite through the levator aponeurosis to reform the lid crease
If fat removal is desired, which is typically only medially, a small incision is made through the septum, entering the medial eyelid compartment. The fat is gently teased out, avoiding excessive posterior traction to minimise the chance of an orbital haemorrhage. Small segments of fat are individually grasped in an artery clamp, cut and the residual base carefully cauterised. The skin incision is closed with interrupted 6-0 prolene sutures. If a firmer skin crease is necessary, the sutures should incorporate the subcutaneous aponeurotic/septal tissue [Figure 4].

- (a and b) Upper lid blepharoplasty. Pre- and post-operative images
LOWER LID BLEPHAROPLASTY
Clinical examination
Lower lid rejuvenation is a controversial topic with multiple surgical and non-surgical treatment options. Lower lid blepharoplasty may represent one technique in a physician's armamentarium for aesthetic enhancement of the lower lid. There are two principal surgical approaches to a lower lid blepharoplasty: Transcutaneous and transconjunctival.[58] Our typical preference is the transcutaneous approach and hence the surgical steps are described in greater detail in this review. The transconjunctival conjunctival approach is employed for younger patients with good skin quality, patients without skin excess and those with a negative orbital vector. The surgical aim in both is to restore a more youth full appearance with a smooth lower lid and blur the transition between the lower lid and the cheek. Lower lid blepharoplasty may also be combined with mid-face surgery. In considering a lower lid blepharoplasty an assessment should make of the excess skin, fat prolapse, lid-cheek junction, the orbital vector and whether any concurrent lower lid laxity is present.
Lid laxity
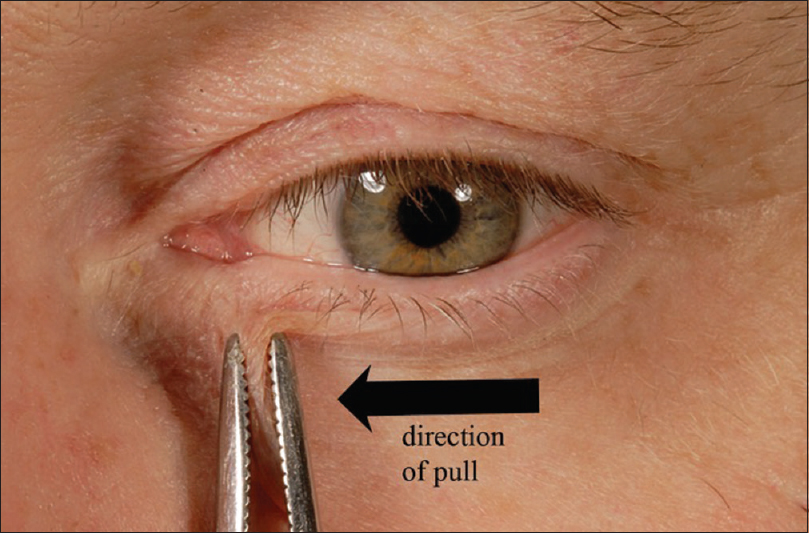
Generalised lid laxity is assessed via the snap-back test and distraction test. If the lower eyelid can be distracted more than 6 mm from the globe, horizontal laxity exists.[9] The snap-back test involves pinching the lower lid and distracting the lid from the globe, if the lid does not snap back against the globe immediately within the time it takes to blink, lid laxity is present [Figure 5]. Specific laxity of the medial and lateral canthal tendon should also be evaluated. Medial canthal tendon laxity is assessed by distracting the lower lid laterally and measuring the punctual excursion distance. If the punctum can be drawn beyond the medial limbus significant medial canthal tendon laxity is present, potentially warranting surgical correction [Figure 6].[10]
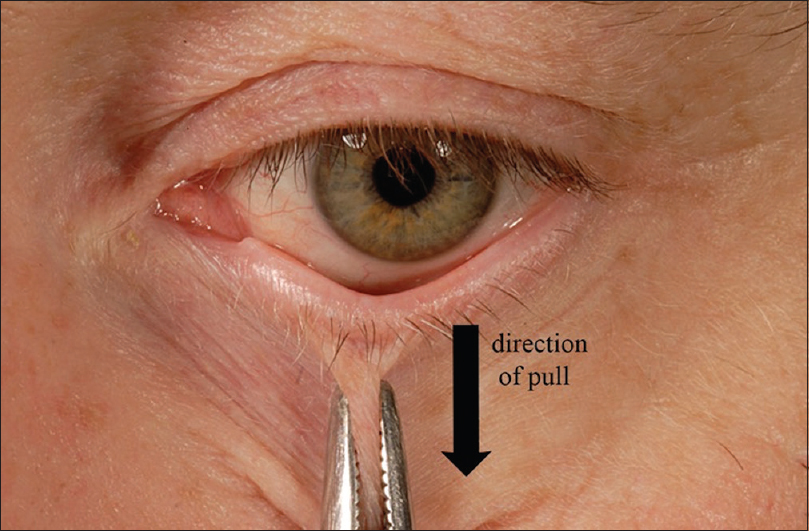
- Image demonstrates the assessment for generalised lid laxity. The snap-back and lid distraction test. NB: This is typically performed in the clinic setting using the physician's thumb and index finger rather than forceps
- Demonstrates assessment for medial canthal tendon laxity. Lateral traction is applied and the punctum excursion is observed
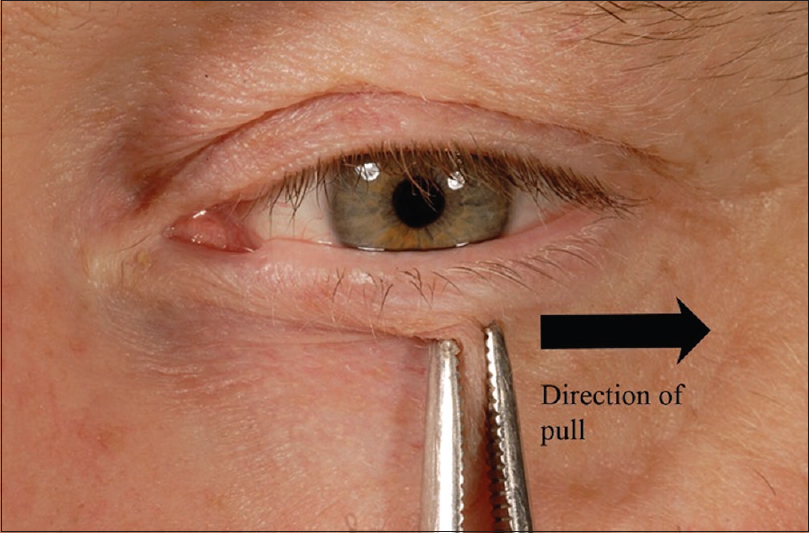
Lateral canthal tendon laxity is assessed by the distraction of the lid medially with the distraction of lateral commissure ≤2 mm considered normal [Figure 7].
- Demonstrates the assessment for lateral canthal tendon laxity
Fat prolapse or attenuation
The lower lid has three fat pads: Medial, central and lateral. The medial and central fat pads are separated by the muscle belly of the inferior oblique, an important structure to be cognisant of to avoid complications [Figures 8 and 9]. The central and lateral fat pads are separated by the arcuate expansion of inferior oblique.[11] The fat pads are best assessed with the patient in the upright position and will typically become more prominent in up gaze.[8] If fat attenuation predominates, volume augmentation techniques may be considered to optimise outcomes.

- Transconjunctival approach to the fat pads via the pre-septal plane
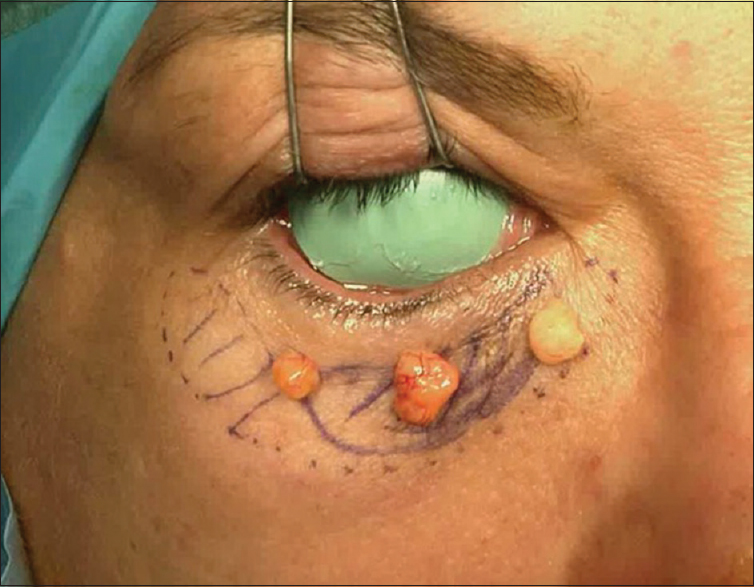
- Image demonstrates pre-operative marking of the three lower lid fat pads and subsequent fat excision using a transconjunctival approach. We use a protective corneal shield in all blepharoplasty surgery procedures
Skin
The quantity of redundant lower lid skin can be assessed by asking patients to open their mouth or look up; both these manoeuvres will stretch the skin, giving an indication of the amount that can be safely excised. Festoons and malar oedema should be noted and discussed with the patient as these will typically not be addressed via standard blepharoplasty techniques.[812]
Surgical technique lower lid blepharoplasty
Transcutaneous lower lid blepharoplasty
Proxymetacaine drops are instilled and a corneal protector placed. A subciliary incision line is marked 2 mm from the lid margin, which extends 5–10 mm beyond the lateral commissure, hidden within a lateral canthal rhytid. A prolene traction suture in placed in the lower lid grey-line. The skin incision is made with a Colorado microdissector needle and a 3–4 mm skin-only flap raised initially. Dissection is continued in a pre-septal plane to maintain strict haemostasis. Close to the level of the orbital rim, the orbital septum is selectively opened in pockets to allow access to the orbital fat pads. The orbital fat can be excised or as a pedicle re-draped medially and centrally to soften a prominent nasojugal fold/tear trough deformity. Our preference is selective fat excision followed by closure of the orbital septum using a 7-0 vicryl suture and thermal septoplasty with the bipolar cautery. A lateral canthopexy using a double-armed 5-0 or 6-0 prolene can be used to support and tighten the lower lid. Excess lower lid skin is marked and excised with typically a broader skin excision laterally tapering medially. Care must be taken not to excise excessive skin, especially medially. An orbicularis flap is created laterally using the monopolar cautery and sutured to the lateral orbital rim or superior limb of the lateral canthal tendon with 6-0 vicryl suture. The subcilary skin incision is then closed with 6-0 prolene suture [Figure 10].
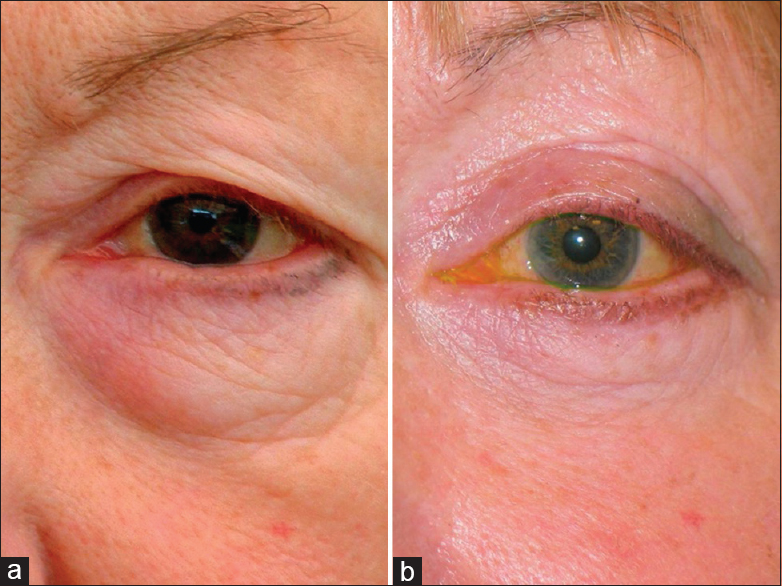
- (a and b) Lower lid transcutaneous lower lid blepharoplasty and upper lid blepharoplasty. Pre- and post-operative photographs demonstrating removal of herniated orbital fat and blending the of the lid cheek junction
MODIFICATION FOR THE TRANSCONJUNCTIVAL APPROACH
Tranconjunctival blepharoplasty may be preferred in younger patients without qualitative age-related skin changes or lid laxity. The eye is initially prepared in the same way as the transcutaneous approach and aprolene traction suture in placed in the grey-line of the lower lid. A conjunctival incision is made inferior to the tarsal border and a pre-septal dissection plane is followed until the orbital rim is reached; the orbital fat pad reduction step is then performed. In this situation, neither the septum nor the conjunctiva is sutured.
LOCAL ANAESTHESIA INFILTRATION
Our local anaesthetic (LA) mixture comprises a 2:2:1 ratio of Lignospan (Novocol Pharmaceutical of Canada; 2% lignocaine with 1:80,000 adrenaline), 0.5% bupivacaine, and 4 mg/ml dexamethasone. This is injected subcutaneously with a 30 g needle using a pinch and roll technique. The skin is pinched and rolled to separate the orbicularis creating a subcutaneous, relatively avascular plane for injection. Typically, two to three millilitres of this LA mixture are required for each eyelid.
POST-OPERATIVE CARE
Preservative free ocular lubricants are prescribed 4 times per day for 2 weeks. Chloramphenicol ointment is used topically on the eyelid incision and in the eye for 2 weeks at night. The skin sutures are removed at 10 days.
COMPLICATIONS
Complications of upper lid and lower lid blepharoplasty include lagophthalmos and eyelid retraction related to excessive skin excision. Untreated this can result in exposure keratopathy with associated persistent discomfort and potential for visual impairment. Sight-threatening orbital haemorrhage is a rare complication but may occur blepharoplasty, especially during retroseptal fat excision. Other complications include infection, transient dry eye, asymmetry of the lid crease or residual upper or lower eyelid skin. Patients should be counselled with regard to these complications and the potential for revision surgery. Pre- and post-operative photographs are recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cosmetic surgery national data bank statistics. Aesthet Surg J. 2015;35(Suppl 2):1-24.
- [Google Scholar]
- The measurement and definition of ptosis. Ophthal Plast Reconstr Surg. 1989;5:171-5.
- [Google Scholar]
- The “bespoke” upper eyelid blepharoplasty and brow rejuvenation. Facial Plast Surg. 2013;29:264-72.
- [Google Scholar]
- Upper blepharoplasty with lateral segmental orbicularis excision. Ann Plast Surg. 2003;50:471-4.
- [Google Scholar]
- Expert Techniques in Ophthalmic Surgery. New Delhi, India: Jaypee; 2015.
- Oculoplastic Surgery. London, UK: Informa Healthcare; 2011.
- Colour Atlas of Ophthalmic Plastic Surgery (2nd ed). Oxford, UK: Butterworth-Heinemann; 2001.
- Surgical anatomy of the forehead, eyelids, and midface for the aesthetic surgeon. In: Master techniques in blepharoplasty and periorbital rejuvenation. New York: Springer; 2011.
- [Google Scholar]
- Malar mounds and festoons: Review of current management. Aesthet Surg J. 2014;34:235-48.
- [Google Scholar]






