Translate this page into:
Overview of Local Flaps of the Face for Reconstruction of Cutaneous Malignancies: Single Institutional Experience of Seventy Cases
Address for correspondence: Dr. Kaustubh Sharad Shende, F-33 R.D. Hostel, SMS Medical College, Jaipur, Rajasthan, India. E-mail: kaustubh117@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
The most common malignant tumours of the face are basal cell carcinoma, squamous cell carcinoma and melanoma. While the results of skin graft are less than satisfactory for large areas to cover, distant flaps are bulky with a poor colour match. Local fasciocutaneous flaps provide reasonable option for reconstruction of facial defects with good colour and texture match and good success rate.
Aims:
This study aimed to analyse the various modalities of reconstruction after resection of facial malignancies and their advantages and disadvantages.
Settings and Design:
This was a retrospective study.
Materials and Methods:
Of 70 patients, 34 were managed with V-Y advancement flap, 24 with nasolabial flap, 8 with median forehead flap and 4 with standard forehead flap cover. The duration of follow-up ranged from 6 months to 2 years.
Statistical Analysis Used:
Nil.
Results:
Of 34 V-Y advancement flaps, 2 showed suture dehiscence at the apex of triangle which was allowed to heal secondarily with regular dressings. All the 24 nasolabial flaps were healthy without any complication. All patients had satisfactory functional and cosmetic outcomes.
Conclusions:
In our experience, local flaps give the best results and are the first choice for reconstruction of the face. Most defects can be best closed by nasolabial, V-Y advancement and forehead flap. Outstanding functional and cosmetic results can be achieved. Proper execution requires considerable technical skill and experience.
Keywords
Cutaneous malignancies
forehead flap
local flaps of the face
nasolabial flap
V-Y advancement
INTRODUCTION
The most common malignant tumours of the face are basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma.[123]
BCC constitutes more than three quarters of skin cancers of the face and the rest primarily consist of SCC.[4] Risk factors for BCC include fair skin type, sun exposure, ionising radiation, advanced age, immunosuppression and a personal history of non-melanoma skin cancer.[5]
While BCCs and other skin cancers of the face are almost always curable when detected and treated early,[6] various treatment modalities are available for reconstruction after excision of tumour of the face from full-thickness skin graft to local or distant flaps for resurfacing of defect. While the results of skin graft are less than satisfactory for large areas to cover, distant flaps are bulky with a poor colour match. It takes several weeks for skin grafts to stabilise and match with the recipient site. Contracture may develop in the long-term follow-up.[7] Local fasciocutaneous flaps provide reasonable option for reconstruction of facial defects with good colour and texture match and good success rate.
We share our experience of seventy patients operated for BCC over the face and reconstructed with various local fasciocutaneous flaps in the past 2 years.
MATERIALS AND METHODS
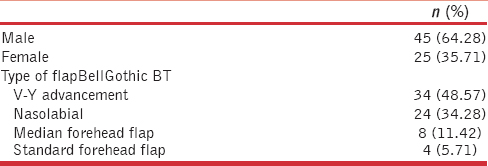
This is a retrospective review of 130 patients who underwent surgical excision of skin malignancy involving the facial region followed by primary reconstruction using local fasciocutaneous flaps. Sixty patients who underwent reconstruction with distant flaps or those managed with primary closure were excluded in this study. There were a total of seventy patients treated with wide excision and local fasciocutaneous flap cover over a period of 2 years (August 2013–July 2015). There were 45 males and 25 females with a mean age of 61 years (range 45–74 years). In all patients, the diagnosis was confirmed by histopathological examination before definitive management. None of the patients had evidence of regional or distant metastasis [Table 1]. The defects following excision ranged from 2 cm × 4 cm to 6 cm × 8cm in size. Of 70 patients, 34 were managed with V-Y advancement flap, 24 with nasolabial flap, 8 with median forehead flap and 4 with standard forehead flap cover. The duration of follow-up ranged from 6 months to 2 years.
Surgical procedure
Nasolabial flap
The flap was designed as an interpolation flap in which the final scar of donor-site closure lies exactly in the nasolabial sulcus. The flap was traced 1 mm larger in all dimensions to allow for post-operative contraction. The inset was thinned distally, leaving only 1–2 mm of subcutaneous tissue in the area of the inset. The donor site was closed by undermining adjacent cheek skin and advancing it, inferiorly and medially. Closure of the donor defect before closure of the primary defect brings the base of the flap closer to the nose, thereby facilitating subsequent closure of the primary defect with minimal wound closure tension. After further 3 weeks, the pedicle was divided. The residual pedicle, which served as a vascular carrier, was discarded, and the cheek was closed by advancement so that the final scar lies exactly in the alar-facial sulcus and nasolabial sulcus. The normal concavity of the nasofacial sulcus can be re-established, using an absorbable suspension suture placed between the undersurface of the dermis of the flap and the periosteum of the nasal bone or maxilla.
V-Y advancement flap
Sliding, subcutaneous V-Y flaps have been gaining in popularity. The advantages of having similar tissue in the same operative field, with an excellent blood supply, make the V-Y flap a common choice. The area of lesion excision and the flap was marked pre-operatively with margin of defect forming base of the triangle for V-Y advancement. Once all margins are known to be clear after tumour excision, the V-Y flap was dissected out and moved anteriorly on a subcutaneous pedicle to repair the defect. However, this flap has limitations as it can be used for relatively smaller defects. Some notching along the alar rim may occur.[8]
Forehead flap
The forehead flap is a two-stage procedure, and patients should be explained this pre-operatively along with their appearance between the two stages of the procedure. The lesion and proposed margin of excision were marked. The proposed reconstruction flap was marked at the same time. In eight cases, the median or paramedian pedicled forehead flap was the method of surgical reconstruction, while in four cases, standard forehead flap was used. For difficult areas such as those involving the medial canthus or the eyelids, mucosal or skin grafts were sutured to the undersurface of the flap to reconstruct the conjunctiva. No cartilage grafts were used (to reconstruct the tarsal plate) because the flaps were “stiff” enough to provide self-support. Whenever possible (especially with defects extending to the nasolabial fold), primary closure of the edge of the defect was done. Lacrimal system reconstruction was not performed in any of the patients. Donor site was closed primarily or with split-thickness skin graft. Forehead flaps were divided 3 weeks later. The pedicles were returned to their donor sites in the forehead after excision of the skin grafts.
It has been our experience that most patients who undergo extensive nasal reconstruction appreciate an overnight admission to aid in wound care and to ensure adequate intravenous hydration. Prescriptions at discharge include a broad-spectrum antibiotic, which is to be taken for 7–10 days. A mild pain reliever, such as diclofenac sodium, and an anti-emetic are often prescribed. Post-operative wound care consists of twice daily cleansing of the suture lines with spirit and application of an antibiotic ointment or petroleum jelly.
RESULTS
All patients tolerated the surgical procedures well with no systemic- or anaesthesia-related complications. There were no infections or haematomas. All flaps survived completely, and there were no instances of graft loss.
Follow-up ranged from 6 months to 2 years (18 months). Tumour recurrence was not seen in any of the patients, during this period. Functionally, whenever the eyelid was involved, there was no ectropion, and the margin was well aligned and stable. Eyelid closure was adequate, and there were no exposure sequelae. However, epiphora was evident since lacrimal system reconstruction was not performed. Cosmetically, there were some colour mismatch and no eyelashes.
Of 34 V-Y advancement flaps, two showed suture dehiscence at the apex of triangle which was allowed to heal secondarily with regular dressings [Figures 1a–c and 2a–c].
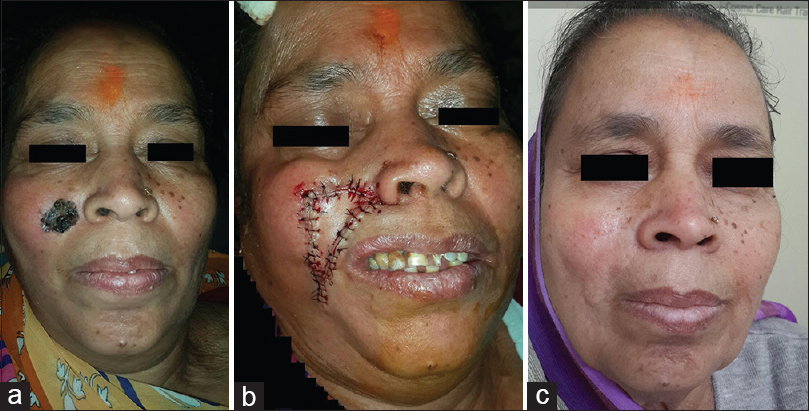
- (a) V-Y advancement patient one - pre-operative photograph, (b) V-Y advancement patient one - immediate post-operative photograph, (c) V-Y advancement patient one - late post-operative photograph

- (a) V-Y advancement patient two - pre-operative photograph, (b) V-Y advancement patient two - immediate post-operative photograph, (c) V-Y advancement patient two - late post-operative photograph
All the 24 nasolabial flaps were healthy without any complication [Figure 3].
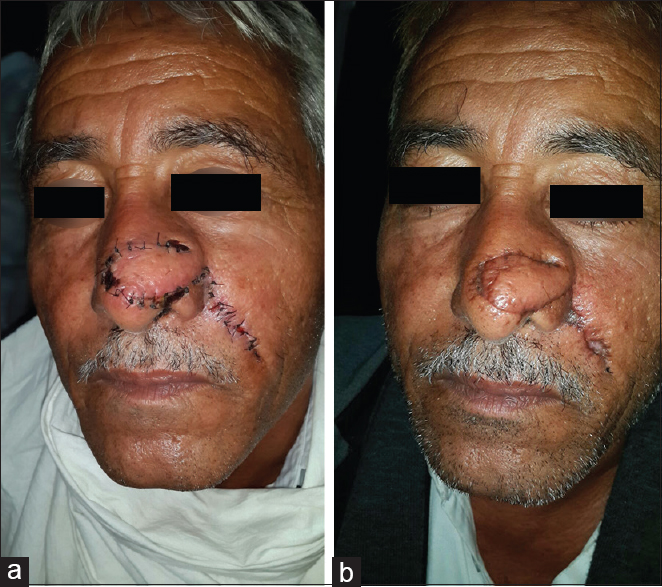
- (a) Nasolabial flap - immediate post-operative photograph, (b) nasolabial flap - post-operative photograph
The donor sites of the forehead flaps were closed primarily in six of eight median forehead flaps. Remaining two median flaps and four standard flaps were covered using split-thickness skin grafts. No graft loss was observed. Eight out of 12 patients treated with forehead flap required debulking of the flaps because of the bulky appearance. Debulking was done 3–6 months following the reconstructive procedures [Figures 4a and b, 5a and b].

- (a) Median forehead flap - pre-operative photograph, (b) median forehead flap - post-operative photograph
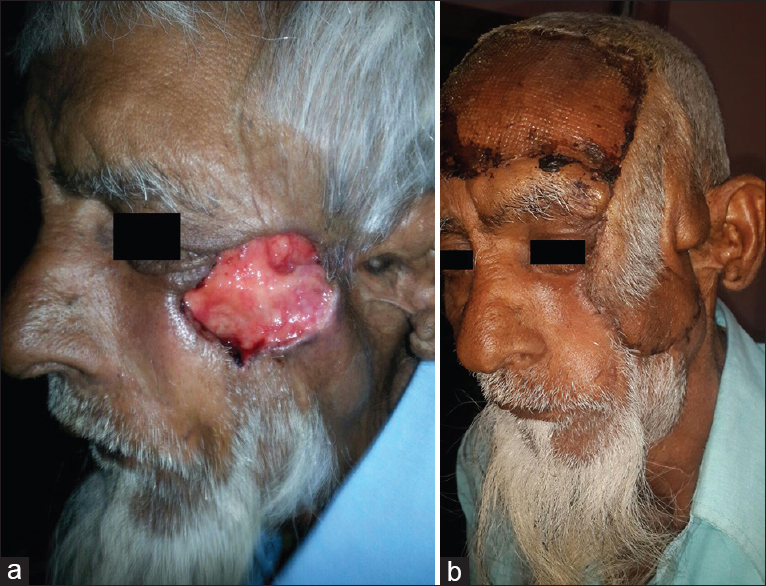
- (a) Standard forehead flap - pre-operative photograph, (b) standard forehead flap - post-operative photograph
All patients had satisfactory functional and cosmetic outcomes.
DISCUSSION
Neoplasm of the skin is found most often on the face. Cosmetically, the face is the most important anatomic area for most patients. Because of this, malignant tumour of the facial skin poses a great challenge in treatment, prohibiting compromises between oncologically responsible surgery and functional plus cosmetic outcome.[9]
BCC is defined by the World Health Organization Committee on the histological typing of skin tumours as “a locally invasive, slowly spreading tumour which rarely metastasise, arising in the epidermis or hair follicles and in which, in particular, the peripheral cells usually simulate the basal cells of the epidermis”.[10] BCC constitutes approximately 75% of non-melanoma skin cancers. It is usually observed in older patients, especially in those frequently and intensively exposed to ultraviolet radiation during their lives. BCC is often observed in the head and neck areas, especially the eyelid and nose. It is more common in males. The tumour grows slowly. BCC may be treated with surgery, cryotherapy, radiotherapy and curettage and electrodessication.[11]
Appropriate follow-up after complete BCC excision has been discussed by several previous studies. Park et al. report only a 1% recurrence rate after complete excision of BCC and suggest no follow-up of these patients is required.[12]
Challenges in periocular reconstruction following the excision of cutaneous malignancy include providing stable eyelid margin, symmetry, smooth internal surfaces, adequate eyelid closure to avoid exposure sequelae, restoring normal tension and providing sufficient horizontal and vertical eyelid dimensions for maximal function.[1314]
Most of nasal skin is of the sebaceous type. Whenever possible, scar lines should be placed along relaxed skin tension lines. Aesthetic units of the nose need consideration. Skin diseases of elderly, such as rosacea and rhinophyma, can interfere with surgical techniques.[15] The skin covering the bony parts is highly movable while the skin over cartilage parts is thicker, tighter and bound to the cartilage. Healing by secondary intention of convex surfaces like the nose tip should be avoided since healing often is delayed and may lead to uneven scars.[16]
For nasal reconstructions, the midline forehead skin flap can serve as a cover for any nasal reconstruction from severe tip and ala loss to a total nasal defect. Using this flap, aesthetic and functional reconstruction can be achieved by creating a nose that blends well with the face. The seagull-shaped flap is based on one of the supratrochlear vessel bundles. Its vertical axis is placed over the midline of the forehead, and the wings are designed to lie in natural transverse creases. The forehead flap is elevated and transposed 180° to cover the nasal defect. The body of the seagull lies along the bridge, the wings curl at the ala and turn into the nostril sills and the seagull head and neck create the tip and columella.[17]
The superiorly based nasolabial flap is useful for defects of the nasal sidewall, ala and tip while the inferiorly based nasolabial flap is useful for defects of the upper and lower lip, nasal floor and columella.[18] The blood supply to flap is from perforating branches of the angular artery which is continuation of facial artery. The colour and texture matches are excellent while the donor-site scar is hidden in the nasolabial sulcus. In the case of defects with diameters between 1.5 cm and 2.0 cm and involving the alar lobules, a nasolabial transposition flap is useful for reconstruction.[192021] The nasolabial fold can supply enough skin to resurface the ala, and the contractility of the nasolabial flap can be used to simulate the round, expected bulge of the normal ala.[2122]
From an aesthetic point of view, the cheek may be divided into three overlapping units: (1) suborbital, (2) preauricular and (3) buccomandibular.[23] Zone 1, the suborbital zone, extends along the lateral border of the nose to the nasolabial fold, across the cheek below the gingival sulcus towards the sideburn, up the anterior sideburn to the lateral crow's-foot line and then along the lower eyelid-cheek junction.[2324] In this location, wounds not amenable to primary or skin graft closure may respond well to rhomboid, circular or bilobed flaps. In addition, cervicofacial flap design or tissue expansion with rotation from a more lateral site is helpful for larger defects. Zone 2, or the preauricular area, extends from the helical junction with the cheek across to the sideburn to overlap with Zone 1 at the malar prominence. This area includes the tissues over the parotid-masseteric fascia and extends inferiorly to the mandibular angle and lower mandibular border. In addition to the local flaps previously listed, regional flaps such as anteriorly based cervicofacial flap, deltopectoral flap and pectoralis major flap may be used for reconstruction at this location. The Zone 3 is buccomandibular area extending from a vertical division at the middle cheek down to the mandibular margin and from the oral commissure back up to a horizontal division line halfway up the cheek. Not only does a majority of the orbicularis oris underlie this area, but also the parotid duct courses through this body of cheek tissue here as well. Reconstruction of this area must take into account important nearby structures, such as the oral commissure, ala and nasolabial fold. Simple flaps, such as the transposition flap, W-plasty or Z-plasty, may be most useful here.
Advancement flap design is relatively simple and can be successfully applied to repair a wide variety of small- or moderate-sized cheek defects. This group of flaps is based on an incision that allows “sliding” movement of the tissue. Because the distal end of the V-Y flap is surgically isolated from the donor site, soft-tissue distortion associated with alternative advancement flaps is minimised.[2526] The advancing tissue can also be based on a neurovascular bundle. The V-Y advancement flap is equally effective for coverage of large cheek wounds and small defects of those approximating the lid or lateral cheek.[26]
CONCLUSION
In our experience, local flaps give the best results and are the first choice for reconstruction of the face. This depends on tissue laxity, vascularity and resulting donor-site distortion. Although many flaps are described, most defects can be best closed by nasolabial, V-Y advancement and forehead flaps. Outstanding functional and cosmetic results can be achieved. Proper execution requires considerable technical skill and experience. Furthermore, a thorough understanding of anatomy and aesthetics is required. With improvements in microsurgical technique and the increased availability of free tissue transfer such as perforator flaps, reconstruction of facial defects has recently undergone rapid evolution. However, the local flaps are still the workhorse for facial reconstruction, placing them at prior step in reconstruction ladder.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Use of a folded forehead flap for reconstruction after a large excision of the full thickness of the cheek. Plast Reconstr Surg. 1975;56:629-32.
- [Google Scholar]
- Bipedal myocutaneous flap for one-stage reconstruction of the cheek after cancer surgery. J Laryngol Otol. 1988;102:601-2.
- [Google Scholar]
- Use of the trapezius and sternomastoid myocutaneous flap in head and neck reconstruction. Plast Reconstr Surg. 1979;63:49-57.
- [Google Scholar]
- Imiquimod 5% cream as adjunctive therapy for primary, solitary, nodular nasal basal cell carcinomas before Mohs micrographic surgery: A randomized, double blind, vehicle-controlled study. Dermatol Surg. 2009;35:24-9.
- [Google Scholar]
- The use of full-thickness skin grafts to repair nonperforating nasal defects. J Am Acad Dermatol. 2000;42:1041-50.
- [Google Scholar]
- Berish S, ed. V-Y flap reconstruction for nasal alae defects. Grabb's Encyclopedia of Flaps. Vol 1. Philadelphia, PA, USA: Lippincott Williams and Wilkins; 2009. p. :101-4.
- Head and neck basal cell carcinoma: Treatment using a 2-mm clinical excision margin. Clin Otolaryngol Allied Sci. 2000;25:370-3.
- [Google Scholar]
- Basal cell carcinomas: Do they need to be followed up? J R Coll Surg Edinb. 1994;39:109-11.
- [Google Scholar]
- Principles of periocular reconstruction following excision of cutaneous malignancy. J Skin Cancer 2012 2012:438502.
- [Google Scholar]
- Reconstructive options for the medial canthus and eyelids following tumor excision. Saudi J Ophthalmol. 2011;25:67-74.
- [Google Scholar]
- Regional variation in wound contraction of Mohs surgery defects allowed to heal by second intention. Dermatol Surg. 2003;29:712-22.
- [Google Scholar]
- Berish S, ed. Midline forehead skin flap. Grabb's Encyclopedia of Flaps. Vol 1. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2009. p. :99-100.
- Reconstruction of nasal cutaneous defects in Asians. Auris Nasus Larynx. 2009;36:560-6.
- [Google Scholar]
- The bilobed flap: A very efficient method in aesthetic reconstruction of small skin defects at the alar and tip regions of the nose. Ann Chir Plast Esthet. 2003;48:211-5.
- [Google Scholar]
- Local Flap in Facial Reconstruction (2nd ed). St. Louis, MO, USA: Mosby; 2007.
- Principlization of Plastic Surgery. Boston, MA: Little, Brown; 1986.
- Combined use of pectoralis major myocutaneous and free radial forearm flaps for reconstruction of through-and-through defects from excision of head and neck cancers. J Otolaryngol. 1999;28:332-6.
- [Google Scholar]
- Improving the donor site of the radial forearm flap. Br J Plast Surg. 1985;38:504-5.
- [Google Scholar]
- Radial forearm flap donor-site complications and morbidity. Plast Reconstr Surg. 1998;101:874-5.
- [Google Scholar]






