Translate this page into:
Subungual Glomus Tumour Excision with Transungual Approach with Partial Proximal Nail Avulsion
Address for correspondence: Dr. Binod Kumar Thakur, Department of Dermatology and STD, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong - 793 018, Meghalaya, India. E-mail: binod.k.thakur@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor
Glomus tumour is a benign vascular hamartoma containing neuromyoarterial cells of normal glomus apparatus first described by Barre and Masson in 1924.[1] The knowledge of this entity and surgical skill is necessary to prevent delay in diagnoses and the treatment. We report a case of subungual glomus tumour successfully excised with transungual approach with partial nail avulsion.
A 58-year-old female presented with pain on the left thumb for 12 years which was gradually increasing in the last 3 years. The pain was worse with exposure to cold water or when she bumped the thumb. There was no other significant medical history.
The general and systemic physical examination was within normal limit. On local examination, there was a violaceous spot on the lunula and longitudinal ridging on the nail plate [Figure 1a]. The love test (applying pressure to the suspected area with a pinhead, which elicits exquisite localised pain) was positive. The posterior-anterior and lateral view of X-ray left hand was normal [Figure 1c]. Magnetic resonance imaging of the left thumb revealed T1 hypointense, T2/T2-FS hyperintense spherical mass showing intense enhancement on the post-contrast study of distal phalanx suggestive of glomus tumour [Figure 1d].

- (a) Violaceous spot suggesting location of glomus tumour with longitudinal ridging, (b) excised glomus tumour kept on the nail plate, (C) X-ray of the left hand, (d) magnetic resonance imaging of the left thumb
The glomus tumour was excised with distal digital block as anaesthesia. The nail plate was marked with a surgical marker at the location of the tumour. Proximal nail avulsion was done to expose the nail bed tumour. The nail bed was sectioned longitudinally over the tumour. The tumour was very meticulously dissected from the surrounding tissue with blunt curved scissors [Figure 1b]. The incision was closed with 4-0 vicryl suture. The nail plate was put back in place as a physiological covering and secured to lateral and proximal nail folds. The tumour was sent for histopathology which showed glomus tumour [Figure 2]. There is no pain or recurrence at 2 years follow-up.
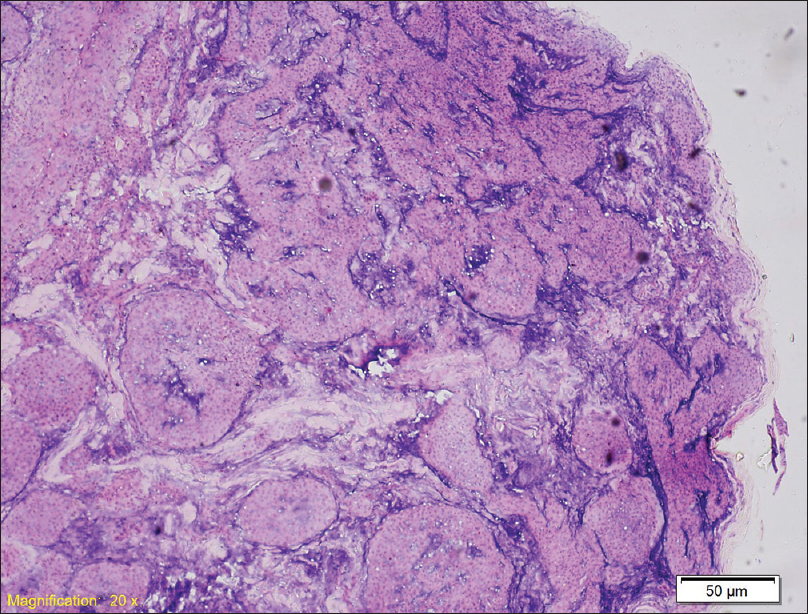
- Histopathology showing features of glomus tumour (H and E, ×100)
The classic triad of symptoms of subungual glomus tumour are severe pain, pinpoint tenderness and temperature sensitivity. With the classical triad of symptoms, glomus tumour can be diagnosed clinically. However, the mean duration of symptoms until diagnosis was 4.6 years (range 1 month to 20 years)[2] and 4.5 years (range, 6 months to 10 years).[3] In our patient, it took 12 years for proper diagnosis after visiting many different speciality clinics. Bhaskaranand and Navadgi in their study of 18 patients revealed that the cold sensitivity test was 100% sensitive, specific and accurate; Hildreth's test was 71.4% sensitive, 100% specific and 78% accurate; and the love pin test was 100% sensitive and 78% accurate.[4]
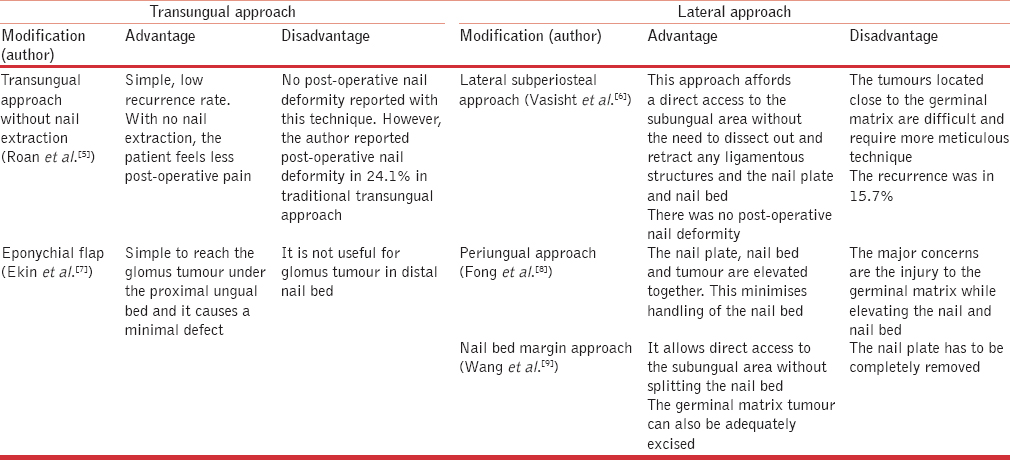
The only effective treatment of subungual glomus tumour is complete surgical excision. Many surgical approaches have been reported to excise the tumour.[23] The standard approach is a direct transungual excision. The different surgical approach for excision of glomus tumour is illustrated in Table 1. Van Geertruyden et al.[10] performed transungual resection in 30 subungual tumours. They reported 6.6% recurrence and a post-operative incidence of nail deformity of 3.3%. Traditionally, a complete nail avulsion is done to expose the tumour. However, in our patient, we did partial nail avulsion to excise the tumour. The transungual approach with partial nail plate removal helps in less post-operative pain and faster healing as the area of surgery is less. It also helps in proper growth of nail as there are no chances of distal nail embedding in the case of proximal nail avulsion as in our case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Anatomy-clinical study of certain painful sub-ungualtumors (tumors of neuromyo-arterial glomus of the extremities) Bull Soc Dermatol Syphiligr. 1924;31:148-59.
- [Google Scholar]
- Surgical treatment of subungual glomus tumor: A unique and simple method. Dermatol Surg. 2009;35:786-91.
- [Google Scholar]
- Subungual glomus tumours: Diagnosis and microsurgical excision through a lateral subperiosteal approach. J Plast Reconstr Aesthet Surg. 2014;67:373-6.
- [Google Scholar]
- Surgical technique innovation for the excision of subungual glomus tumors. Dermatol Surg. 2011;37:259-62.
- [Google Scholar]
- Digital glomus tumors: A 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004;114:1486-9.
- [Google Scholar]
- Subungual glomus tumours: a different approach to diagnosis and treatment. J Hand Surg Br. 1997;22:228-9.
- [Google Scholar]
- A modified periungual approach for treatment of subungual glomus tumour. Hand Surg. 2007;12:217-21.
- [Google Scholar]
- Treatment of subungual glomus tumors using the nail bed margin approach. Dermatol Surg. 2013;39:1689-94.
- [Google Scholar]
- Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21:257-60.
- [Google Scholar]





