Translate this page into:
Angiolymphoid Hyperplasia with Oeosinophilia Showing Promising Result with Intralesional Radio-frequency Ablation Therapy: A New Cost-effective and Hassle-free Modality of Treatment
Address for correspondence: Dr. Chintaginjala Aruna, Department of DVL, Katuri Medical College and Hospital, Guntur, Andhra Pradesh, India. E-mail: draruna88@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
A 32-year-old female presented with itchy erythematous papules and nodules of varying sizes over the scalp for the past 7 years. Lesions were progressive and bled on manipulation.
Dermatological examination revealed multiple, firm, non-tender, scaly, erythematous papules and nodules, ranging from 0.5 cm × 0.5 cm to 1.5 cm × 2 cm, few of them arranged in clusters on the posterior aspect of the scalp. General physical and systemic examinations were normal. There was no lymphadenopathy [Figure 1a and b].

- (a) Multiple, erythematous, papules and nodules arranged in clusters, (b) close-up view of lesions, (c) histopathology showing numerous blood vessels in the background of inflammatory infiltrate (d) close-up view of vessel lined by plump endothelial cells ‘epitheloid endothelial cells’ (H and E, ×100)
A provisional diagnosis of angiolymphoid hyperplasia with oeosinophilia (ALHE) was considered. Routine blood investigations were normal. Biopsy revealed numerous capillaries with prominent plump endothelial lining with surrounding dense inflammatory infiltrates in the dermis, consistent with ALHE [Figure 1c and d]. She was put on oral steroids (prednisolone 1 mg/kg/day) and topical imiquimod (3 days in a week) for 2 months, with no improvement, which led us to opt for a newer technique, intralesional radio-frequency ablation (RFA). We employed ‘Mega Surg Gold’ high-frequency radiosurgery unit (dermaindia) for the procedure [Figure 2]. After local infiltration with 2% lignocaine, a 22-gauge needle was inserted with its distal 3 mm–0.5 cm (depending on the size of the lesion) inside the lesion. RFA was performed at high power-in coagulation mode by touching the needle at its proximal end [Figure 3] and needle was slightly lifted with help of forceps to avoid thermal damage to the uninvolved epidermis and dermis. With single epidermal entry point, fanning technique was employed, and energy was passed for an average of 15–20 s before the change of direction of the needle. Eight sessions were performed over a period of 4 months (at 2 week interval), treating 4–5 lesions in each session. By the end of the last session, there was remarkable resolution of lesions with minimal scarring at the treated area, which was almost invisible after the growth of surrounding hair [Figure 4]. There was no recurrence of lesions during the follow-up period of 1 year.
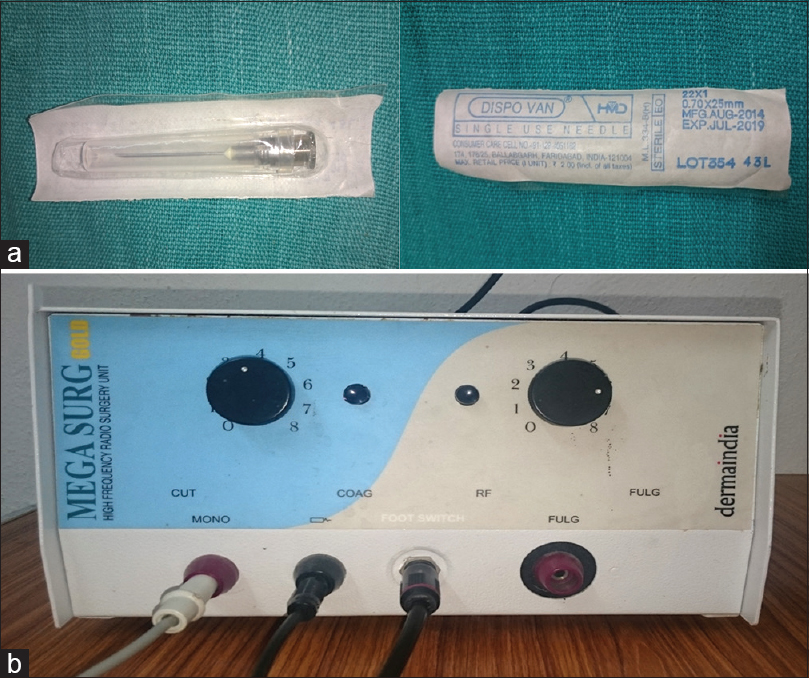
- (a) 22-gauge sterile needle used for intralesional radio-frequency ablation and (b) radio-frequency ablation equipment
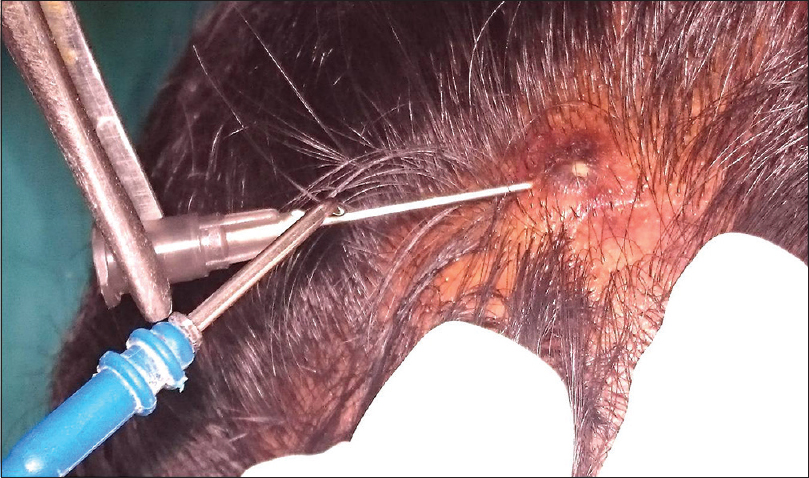
- Intralesional radio-frequency ablation technique
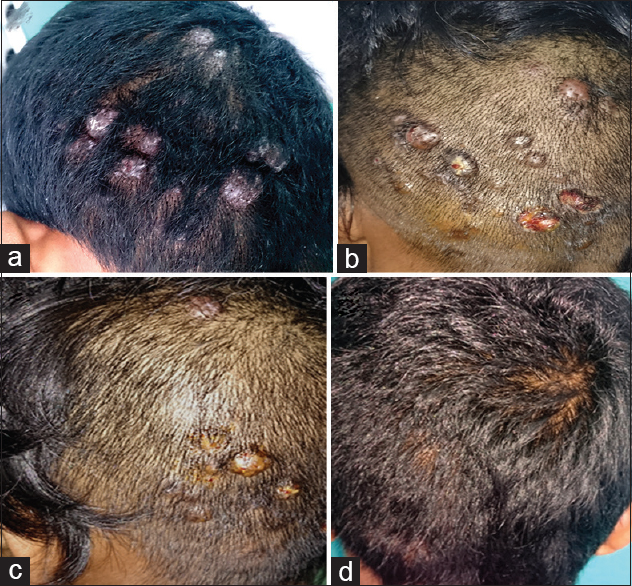
- (a) Initial presentation of angiolymphoid hyperplasia with eosinophilia, (b) at the end of the fourth session, (c) sixth session, (d) 2 weeks after the last session
DISCUSSION
Although ALHE is a benign vascular tumour, it is potentially disfiguring; hence, there is a need for therapy with good curative and cosmetic result as well.
Various topical agents such as timolol, imiquimod, tacrolimus and systemic agents such as corticosteroids, propranolol, retinoids, pentoxifylline and chemotherapeutic agents such as vinblastine and mepolizumab (anti-interleukin-5) have been tried with inconsistent results. Surgical excision can be considered, but local recurrences occur in 33–50% as the lesions are often multilobulated and poorly delineated. Photodynamic therapy, electrocautery, cryosurgery and intralesional corticosteroids, interferon alfa-2a, lasers have shown some success.[1234] Although there are many modalities available in the treatment of ALHE, showing variable results, none of them are completely satisfactory and cost-effective.
Intralesional RFA is a minimally invasive procedure with added advantage of less surface damage and has been employed recently in the management of ALHE. In a report of ALHE being treated with intralesional RFA, an 18 gauge intravenous cannula Venflon was used with good results.[5] We used 22 gauge needle, which is much cheaper than the intravenous cannula for intralesional RFA without any difference in outcome. This particular method is useful for widespread lesions where medical and surgical modalities produce suboptimal results. Post-procedure complications include minimal scarring and depigmentation, which in areas such as scalp can be invisible/camouflaged with hair, like in our case.
This case is reported for intralesional RFA therapy being a new, cost-effective and easy-to-treat modality in the management of ALHE with a long-lasting result and no relapses, especially in limited resource settings, as it just requires an RFA and a sterile needle.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Successful management of angiolymphoid hyperplasia with eosinophilia in a split-face trial of topical tacrolimus and timolol solution. G Ital Dermatol Venereol 2014
- [Google Scholar]
- A long-term follow-up of angiolymphoid hyperplasia with eosinophilia treated by corticosteroids: When a traditional therapy is still up-to-date. Case Rep Dermatol. 2011;3:64-7.
- [Google Scholar]
- Angiolymphoid hyperplasia with eosinophilia treated with anti-interleukin-5 antibody (mepolizumab) Br J Dermatol. 2004;151:1103-4.
- [Google Scholar]
- Angiolymphoid hyperplasia with eosinophilia treated with isotretinoin. Eur J Dermatol. 2007;17:554-5.
- [Google Scholar]
- Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: A minimally invasive approach. Indian J Dermatol Venereol Leprol. 2014;80:419-21.
- [Google Scholar]





