Translate this page into:
A Linear Fleshy Corrugated Plaque on the Right Vulva: A Diagnostic Surprise
Address for correspondence: Dr. Aditya Kumar Bubna, Department of Dermatology, Sri Ramachandra University, Porur, Chennai - 600 116, Tamil Nadu, India. E-mail: zimbabwa21@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Vulvar dermatosis may confuse many specialists who deal with the female genito-urinary system. The difficulty arises because majority of the conditions witnessed are dermatological, and patients usually first attend gynaecology and urology specialist clinics for these disorders. Further, this is compounded by the fact that many common disorders when involving the vulva are usually modified with atypical presentations posing difficulties in the diagnostic acumen of even experienced dermatologists.
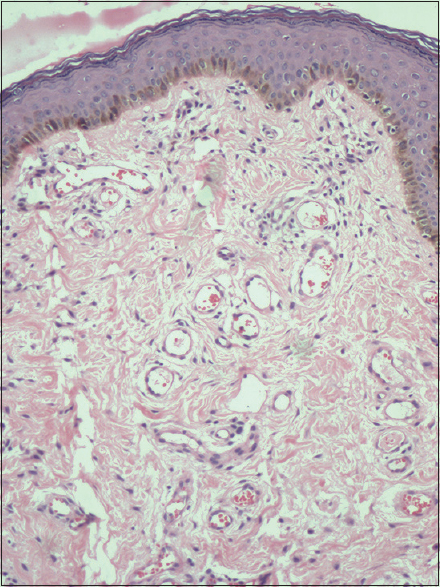
A 23-year-old female presented to the department of dermatology with the chief complaints of an enlarging lesion on the right vulva for the past 4 months. She stated that the lesion began as a small pea-sized growth, almost 1 year back, but because it was asymptomatic, she had completely ignored it. However, now as the swelling was gradually increasing in size, she ascertained the importance of seeking medical attention. Examination revealed a fleshy corrugated linear plaque over the right vulva of length 8 cm extending from the medial to the lateral border [Figure 1]. Palpation demonstrated a non-tender fleshy growth with a bag of worms-like feel. No other associated lesions were identified. Differential diagnosis of plexiform neurofibroma (PN) and isolated collagenoma (IC) was considered, and a lesional skin biopsy was sent for histopathological examination. Histopathology revealed an absolutely unexpected result. Epidermis was intact with normal architecture. Dermis revealed fibrocollagenous tissue interspersed with blood vessels [Figure 2]. With these findings, a diagnosis of fibroepithelial polyp (FEP) was made, and treatment options explained to the patient. Our patient did not want cold knife surgery, therefore the entire lesion was zapped using carbon dioxide laser. After 1 week of follow-up, the lesion was healing well [Figure 3], and after 2 months, there was complete re-epithelialisation with moderate amount of post-inflammatory hypopigmentation [Figure 4]. The patient was satisfied with the result.

- A fleshy, corrugated, linear plaque on the right vulva
- Section of the skin demonstrating a normal epidermis with a fibrocollagenous dermal stroma interspersed with blood vessels (H and E, ×20)

- Right vulva 1 week post-carbon dioxide laser ablation

- Right vulva 2 months post-carbon dioxide laser ablation demonstrating good re-epithelialisation with moderate post-inflammatory hypopigmentation
FEPs are benign neoplasms commonly occurring in obese individuals and located primarily in intertriginous areas. When involving the vulva, they rarely exceed 5 cm in size. These lesions usually are totally asymptomatic and benign. However, there have been reports of the secondary malignant changes in some, and therefore this possibility should not be completely ignored. The main reason for seeking medical attention for genital acrochordons is the fear of suspicion of an existing sexually transmitted disease. In general, the presentation witnessed with vulvar acrochordons is that of a cutaneous flesh-coloured growth, usually attached to a pedicle and protruding from the vulva. However, there have been a few reports depicting atypical phenotypes of FEPs[123456] and they are summarized in Table 1.
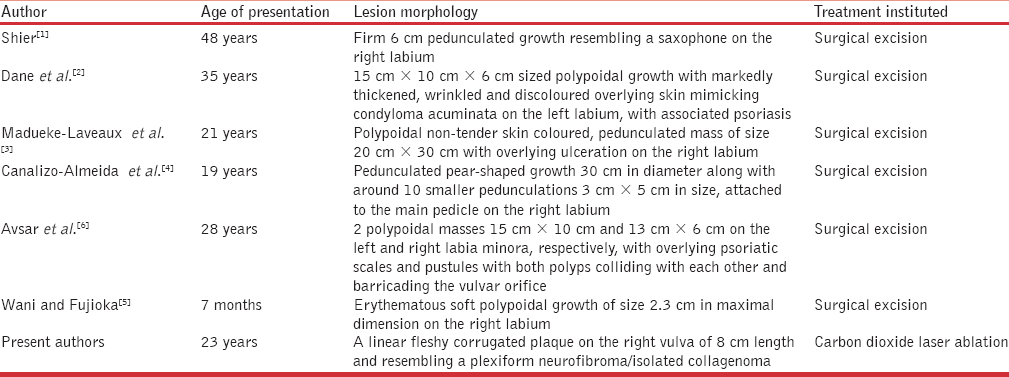
Our case had a distinctive presentation of its own, not blending the slightest, with any of the previous unusual phenotypes described. The morphology in our patient bore a close resemblance to PN with the characteristic bag of worms-like feel. A thorough PubMed literature search with respect to vulvar neurofibroma revealed only two reports by Skorupski et al.[7] and Pascual-Castroviejo et al.[8] However, in all their cases, other hallmark characteristics of Von Recklinghausen (VR) disease were also present. Our case did not demonstrate other findings of VR disease, and therefore it was essential to consider other differentials. The other possibility contemplated upon was IC. ICs are acquired connective tissue nevi characterised by increased dermal collagen deposition usually located on the trunk and upper extremities.[9] IC, involving the vulva, is a rarity, and till date, there have been no reports depicting the same. It was the histological findings that enabled us to clinch the diagnosis. Occasionally, in some biopsy specimens of FEPs, multinucleate giant cells in a focal myxoid stroma maybe encountered,[5] which the diagnosing dermatologist should be aware about. In general, for vulvar FEPs, surgical excision is the treatment employed. However, our patient was reluctant for cold knife surgery. Therefore, the entire lesion was ablated using carbon dioxide laser, which after 2 months of follow-up demonstrated excellent re-epithelialisation. To conclude, all dermatologists should be adequately aware regarding vulvar dermatosis with a careful inclination to atypical phenotypes presented and how a common clinical condition could present so differently, significance of being familiar with the histological characteristics of these dermatoses, importance of a thorough workup to come to a conclusive diagnosis along with knowledge regarding the availability of newer alternative treatment modalities and their appropriate usage while managing these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Fibroepithelial stromal polyp of the vulva. J Obstet Gynaecol Can. 2009;31:1009-10.
- [Google Scholar]
- Association of psoriasis and vulval fibroepithelial polyp:First reported case. Am J Clin Dermatol. 2008;9:333-5.
- [Google Scholar]
- Giant fibroepithelial stromal polyp of the vulva: Largest case reported. Ann Surg Innov Res. 2013;7:8.
- [Google Scholar]
- A vulvar fibroepithelial stromal polyp appearing in infancy. Am J Dermatopathol. 2009;31:465-7.
- [Google Scholar]
- A rare clinical presentation of giant bilateral labial fibroepithelial stromal polyps in patient with psoriasis disease. Case Rep Obstet Gynecol 2016 2016:7942365.
- [Google Scholar]
- A rare vulvar manifestation of neurofibromatosis 1 in a teen. J Pediatr Adolesc Gynecol. 2011;24:e103-5.
- [Google Scholar]
- Neurofibromatosis type 1 with external genitalia involvement presentation of 4 patients. J Pediatr Surg. 2008;43:1998-2003.
- [Google Scholar]





