Translate this page into:
Unusual Site for Cystic Hygroma: A Single Centre Experience
Address for correspondence: Dr. Vijai Datta Upadhyaya, SGPGIMS, Lucknow, Uttar Pradesh, India. E-mail: upadhyayavj@rediffmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Head and neck is the most common site of occurrence of cystic hygroma (CH) constituting 75%[1] followed by axilla. We are presenting a series of CH of rare sites such as breast, parotid gland and anterior chest wall managed with intralesional bleomycin (ILB). A total of seven cases were included in the study. The distribution of the lesion in present series are as; two each of parotid, breast and three in anterior chest wall. Complete resolution was observed in six out of seven cases, number of ILB session per patient was 1.3 and surgery was required in one case.
Clinically, CH is soft, compressible, non-tender, transluminant and lacks bruit. On ultrasound, it is multicystic with no flow on colour Doppler study. Computed tomography (CT) scan and magnetic resonance imaging (MRI) reproduce the same features in difficult locations and help in determining the form, extent and nature of lesion. These cysts are usually filled with; straw coloured, serous and less commonly milky fluid if the cyst has prominent lymphatic communication. The aspiration of serosanguinous fluid, with internal echoes on imaging; points to secondary infection or haemorrhage within the cyst. Conclusive diagnosis of CH/cystic lymphangioma at atypical sites is a challenge; however, ultrasound, Doppler study combined with clinical examination, aspiration of milky/serous/serosanguinous/straw-coloured fluid and aided by CT/MRI in selective cases provides reasonably accurate diagnosis, as in our series. It has been our observation that most of the atypical lesions are relatively smaller in size as compared to head and neck lesions. Moreover, they contain multiple smaller cysts unlike CH in head and neck region which have larger and fewer individual cysts.
For head and neck lesions, due to high morbidity and recurrence,[2] in many centres, worldwide surgical interventions is reserved for cases that have poor response to sclerotherapy. However, surgery has been the mainstay of treatment for atypical sites such as breast,[3] parotid gland[4] and anterior chest wall.[5]
As per our protocol, all patients were strictly scrutinised for the presence of any lung pathology before initiation of therapy and were subjected to one shot of intravenous antibiotic before ntralesional sclerotherapy and oral antibiotics for 72 h and analgesic for 48 h post-procedure. All interventions were done under general anaesthesia/sedation in operation theatre [Figure 1]. Individual cysts were punctured under ultrasonography guidance [Figure 2]; content of the cyst was aspirated completely. Bleomycin was injected individually in each cyst, and care was taken that total dose should not exceed the recommended dose (i.e., 0.5 mg/kg [3 mg/ml solution]). In cases of multiple cysts, the total dose given is divided according to cyst size. The cyst was punctured under ultrasound guidance using 22 Fr. or 20 Fr. intravenous cannula depending on the age of patient and site and size of the lesion [Figure 1]. After puncture, metallic stellate of the cannula was used to monitor, the exact placement of the cannula in the cyst cavity. The main objective of cyst aspiration was to completely evacuate the cyst for optimum action of the drug. Post-procedure, compression of the injection site (wherever it was possible) was done for 6 h. Strict monitoring of the vitals was done up to 6 h post-procedure and patients were discharged within 24–48 h of the procedure. We followed our patients at interval of 3 months [Figure 3] and repeat ultrasound was done at second visit. Reported complications of sclerotherapy with bleomycin include discolouration of the injection site, sudden increase in the size of lymphatic malformation, fever, vomiting, cellulitis, interstitial pneumonia and pulmonary fibrosis but we encountered post-sclerotherapy fever in one patient while others did well in follow-up.

- Chylous fluid aspirated from right breast
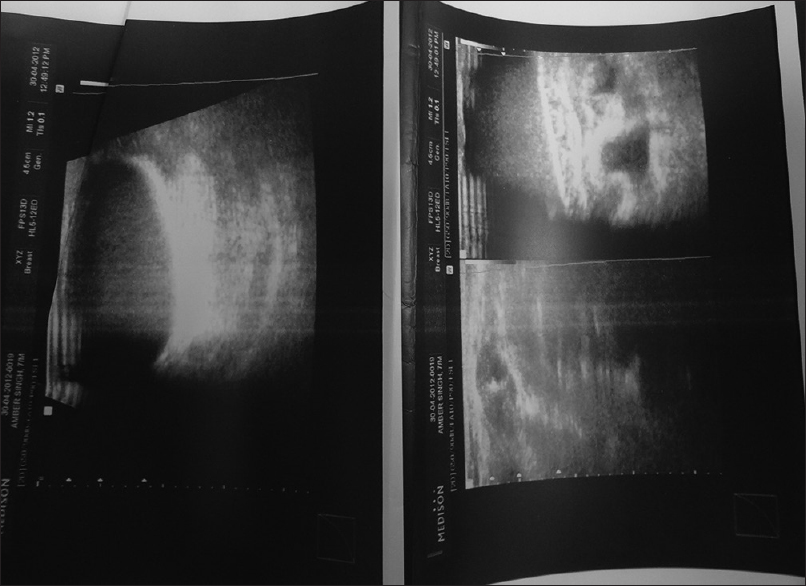
- Ultrasound showing cystic space in the right breast

- Post-sclerotherapy result
We believe that our treatment protocol of post-aspiration sclerotherapy of each individual cyst under ultrasound control provides a good non-surgical treatment option for CH at atypical sites as well. The good result in our series may be because of more intense inflammation on cyst wall due to complete aspiration of cystic fluid before putting bleomycin, use of concentrated bleomycin solution (3 mg/ml) (although the total dose did not exceed 0.5 ml/kg per session) and post-procedural compression (where ever it was possible). Second, in the present series, the proposed interval between the two sessions is 6 months or more which may be the optimum time for desired action of drug especially at atypical sites.
CONCLUSION
CH should be considered as differential diagnosis of cystic lesion in the sites other than head and neck especially in children and can be readily diagnosed by ultrasound ILB is an effective alternative to surgery even at atypical sites of CH which provide better aesthetic outcome, and avoids complication associated with surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Macrocystic lymphatic lymphangioma (cystic lymphangioma) of the upper extremity: A case report. Arch Pediatr. 2008;15:1416-9.
- [Google Scholar]
- Cystic lymphangioma of the breast in a 6-year-old boy. J Pediatr Surg. 2009;44:2015-8.
- [Google Scholar]
- Cystic lymphangioma of the chest wall: A case report. Case Rep Gastroenterol. 2014;8:393-7.
- [Google Scholar]





