Translate this page into:
A Comparative Study of Collagen Dressing versus Petrolatum Gauze Dressing in reducing Pain at the Donor Area
Address for correspondence: Dr. BA Ramesh, Assistant Professor in Plastic Surgery, Sri Ramachandra University, Porur, Chennai - 600 116, TamilNadu, India. E-mail: drbarame@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Skin graft is one of the commonly done procedures by plastic surgeons, dermato surgeons and general surgeons. Pain at the donor area is a common complaint by the patient. The skin graft donor site area is usually covered with petrolatum dressing dermatosurgeons.
Aim:
This study was done to compare collagen dressing with petroleum gauze dressing in control of post-operative pain on skin graft donor area.
Materials and Methods:
The study was done on forty patients, twenty as study group who received collagen dressing and twenty as control group who received petroleum gauze dressing. The procedure was randomly selected by permutated block size of four. The post-operative pain was assessed with numerical pain rating scale 0 to 10. Nursing staff did the recording of pain scale. The nursing staff was not aware whether patient had collagen or petroleum gauze dressing.
Statistics:
Statistical analysis used was independent ‘t’-test (two-sample test) and Levene's test.
Results:
Statistics proved that study group (collagen dressing) had lesser pain than control group (petroleum gauze dressing).
Conclusion:
The collagen sheet dressing on skin graft donor area reduces pain in post-operative period.
Keywords
Collagen sheet
dressing
petroleum gauze
post-operative pain
skin graft
INTRODUCTION
Collagen sheet dressing is a common procedure for covering exposed dermis of superficial thermal burns. It covers the exposed free nerve endings in the dermis, thereby reducing pain and infection. Skin graft is one of the commonly done procedures by plastic surgeons, dermato surgeons and general surgeons. After harvesting the split skin graft dermis is exposed at the donor site, resulting commonly with postoperative pain. Conventionally, the donor area is dressed with non-adherent petroleum gauze. In this study collagen sheet was used for covering the donor site after split thickness skin graft harvest. The donor site pain in the post-operative period can be assessed by numerical pain rating (NPR) scale. NPR scale involves asking the patient to rate their pain from 0 to 10 (11-point scale).
Aim
The study compares collagen dressing versus traditional petroleum (Vaseline) gauze dressing on the donor site region of skin graft with reference to control of pain. The study does not assess wound healing role of collagen.
MATERIALS AND METHODS
The study was done from November 2014 to May 2016 in a tertiary care centre. The inclusion criteria were those with post-traumatic or post-infective raw area and surgically created defect. The exclusion criteria were children below 12 years of age, patients with burns whose analgesic requirement were more and difficult to compare with the study proposed, immunocompromised patients where wound healing may be affected, mentally-ill patients and any condition which influences pain recording.
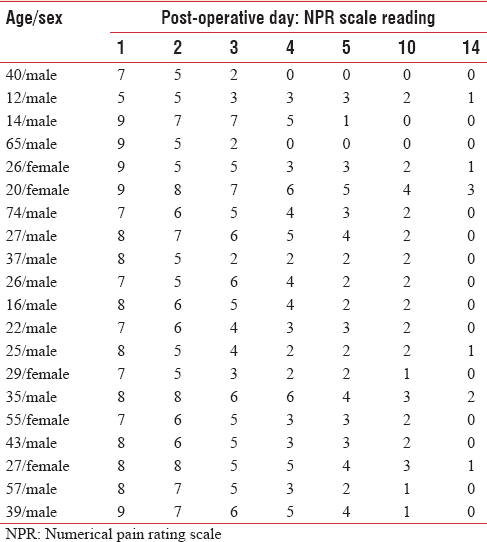
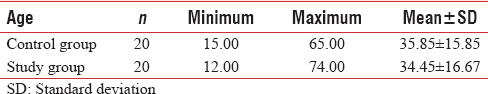
Procedure for the study included dividing the selected sample into two groups. The donor site dressing was done in two different ways. One was dressed with meshed collagen sheet which was dried with warm air dryer and other with petroleum gauze dressing. Randomly permuted block size of 4 which is the most effective method for small sample size randomisation was used in this study. The sample was split into groups of four, namely CPCP, CPPC, PCCP, PCPC, PPCC and CCPP. C stands for collagen and P stands for petroleum gauze dressing. Each block was randomly chosen, and samples were operated accordingly. For example, if CPCP is chosen, collagen was applied for the first surgical donor area and petroleum gauze for second. Assessment of post-operative pain was done by NPR scale from 0 to 10 (11-point scale), with the understanding that 0 represents one end of the pain intensity (no pain) and 10 represents the other extreme of pain severity (unbearable pain). All patients were prescribed paracetamol tablets thrice daily as analgesic. The NPR recording was done in morning before paracetamol was administered. Staff nurse did the recording of pain scale. The staff nurse was not aware whether patient had collagen or petroleum gauze dressing. Pain was recorded on the 1st, 2nd, 3rd, 4th, 5th, 10th and 14th days by NPR [Tables 1 and 2]. On the 10th post-operative day when the superficial dressing was changed by the surgeon, pain was recorded by staff nurse without seeing the wound. If the patient developed dressing soakage, in between, the dressing was changed immediately. Deeper dressing covering the collagen and petroleum gauze was not opened. Standard antibiotics were given to all patients for 5 days.

Statistics
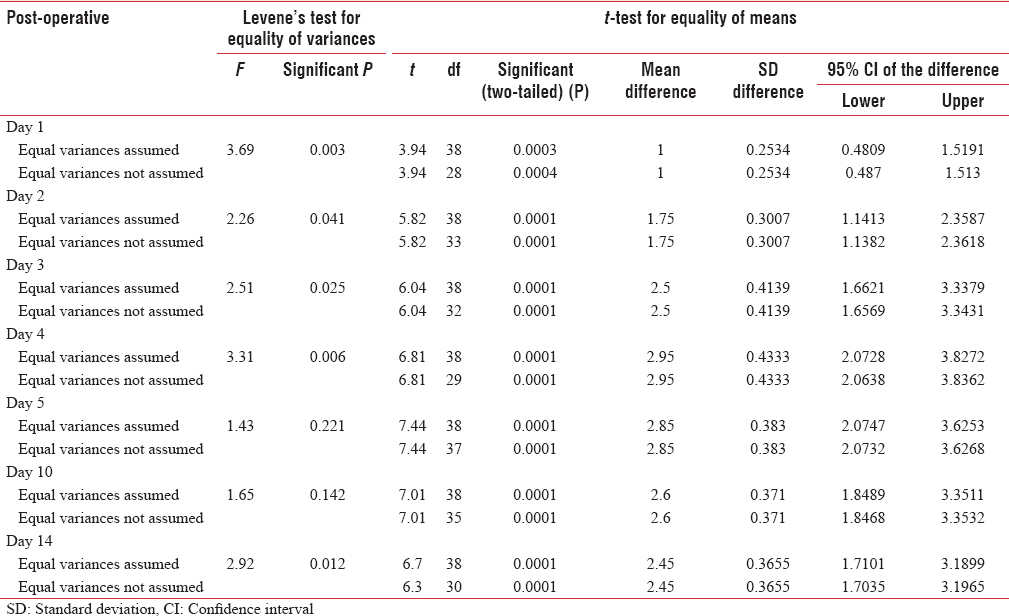
Plan of analysis was based on statistics. Statistical method used was independent two-sample t-test and Levene's test (Levene's test for determining the equality of variances and t-test for equality of means). Test of significance was set at P < 0.05. Null hypothesis was used meaning that there is no difference in pain between control and study groups. The observer bias, selection bias, sampling bias and response bias were eliminated in this study.
RESULTS
From the population of a total of 52 cases operated, forty samples were chosen. Twelve patients were excluded from the study. The reason being nine patients wanted early discharge, one patient in study group and two patients in control group developed infection on donor site during the 1st week. The sampling size was forty; collection of information on pain was done by the NPR scale. The source of information was from sample. The data collected from control and study groups were represented on notched boxplots [Figures 1 and 2]. The pain was analysed using statistics in both groups on days 1, 2, 3, 4, 5, 10 and 14. The average pain score in study group (i.e. collagen sheet dressing) was found to be less compared to control group (i.e., petroleum gauze dressing).
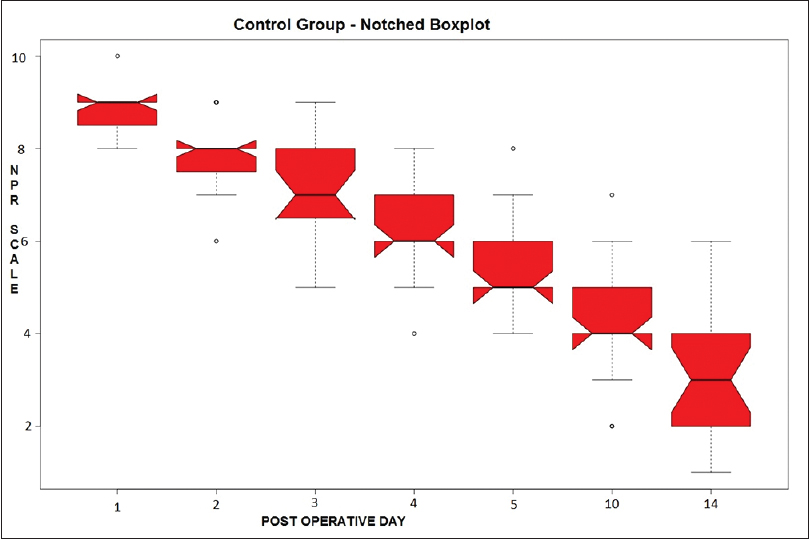
- Control group notched boxplot
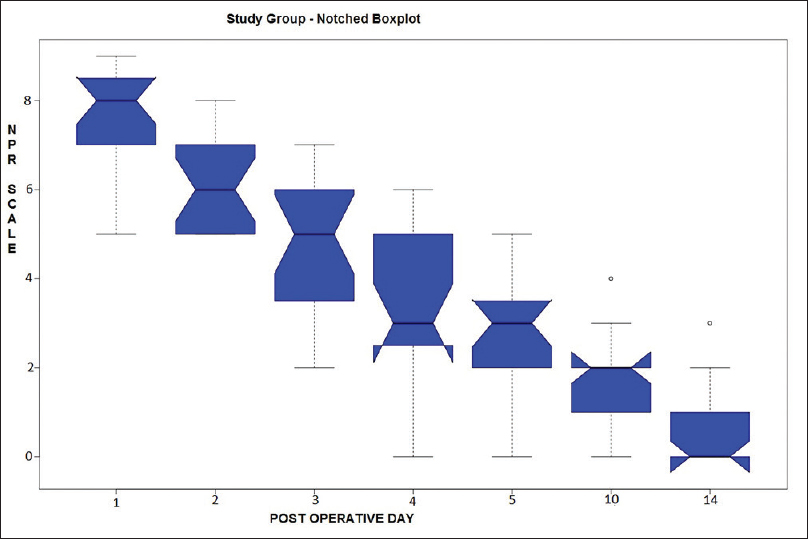
- Study group notched boxplot
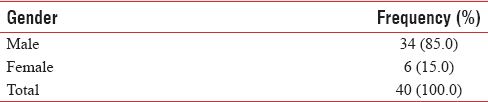
For our study, twenty samples of control and twenty samples of study group were selected. Out of them, 34 (85%) were male and remaining 6 (15%) were females [Table 3]. The control group age was in the range of 34.70 % 18.24 and study group age was in 36.70 % 19.52 [Table 4].
Statistical data provide detailed information regarding the study. Using inferential statistical methods, Levene's test F value was calculated on days 1, 2, 3, 4, 5, 10 and 14. Independent t-test value of study group and control group was analysed [Table 5]. Evaluation of results from tests, Levene's test of equality of variances and independent t-test showed that the study group had less pain. Therefore, the collagen sheet dressing was found to produce statistically significant reduction of pain (P < 0.05). The study design has adequately assessed the null hypothesis. The hypothesis is supported by the statistical results. Thus, collagen sheet was found to be superior to petroleum gauze dressing in reducing the pain in the donor site.
DISCUSSION
The study was done to assess the true role of collagen in post-operative pain control. The role of collagen dressing in better pain control and superior wound healing is found in literature.[123] Collagen sheets, when applied to a wound, not only promote angiogenesis, but also enhance body's repair mechanisms. Collagen dressing is reported to lead to early and greater degree of mobilisation and more comfort. Collagen is a biomaterial that encourages wound healing through deposition and organisation of freshly formed fibres in the wound bed, thus creating a good environment for wound healing. Collagen is easy to apply and has the additional advantage of stopping bleeding.[45] The closed-dressing method shows qualitatively superior healing when compared with open- and semi-open donor sites. This is due to protection from dehydration and mechanical injury and avoidance of contamination.[6] Comparison between collagen dressing and polyurethane showed that collagen was superior in reducing the discomfort and increasing healing.[7] Collagen dressings help to maintain a moist wound environment which is important for better wound healing.[89] The commonly described moist dressings in literature are Kaltostat, Opsite, Duoderm and Allevyn and nonmoist dressings include Xeroform, Scarlet Red and Jelonet.[10111213]
CONCLUSION
We conclude that pain relief was superior with collagen sheet dressing when compared with petroleum gauze dressing and was statistically significant (P < 0.05).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Collagen dressing versus conventional dressings in burn and chronic wounds: A retrospective study. J Cutan Aesthet Surg. 2011;4:12-6.
- [Google Scholar]
- Comparative study of collagen and paraffin gauze dressing on skin graft donor site. Indian J Burns. 2015;23:81-3.
- [Google Scholar]
- Collagen dressing in the management of donor site of split thickness skin grafts. Bombay Hosp J. Available from: http://www.bhj.org.in/journal/april2005/htm/original_Collagen_114.htm
- [Google Scholar]
- Extra cellular wound matrices: Novel stabilization and sterilization method for collagen-based biologic wound dressings. Wounds. 2007;19:148-56.
- [Google Scholar]
- Thrombospondin-1 acts via IAP/CD47 to synergize with collagen in alpha2beta1-mediated platelet activation. Blood. 1999;94:642-8.
- [Google Scholar]
- Which dressing for split-thickness skin graft donor sites? Ann Plast Surg. 2001;46:409-14.
- [Google Scholar]
- Comparison of the effect of a collagen dressing and a polyurethane dressing on the healing of split thickness skin graft (STSG) donor sites. Scand J Plast Reconstr Surg Hand Surg. 1998;32:407-13.
- [Google Scholar]
- Modern collagen wound dressings: Function and purpose. J Am Col Certif Wound Spec. 2011;2:50-4.
- [Google Scholar]
- Comparison of three different methods of dressing for partial thickness skin graft donor site. World J Plast Surg. 2013;2:26-32.
- [Google Scholar]
- Comparison of two dressings in the management of partial-thickness donor sites. J Wound Care. 1999;8:457-60.
- [Google Scholar]
- Comparative clinical study of Bactigras and Telfa AMD for skin graft donor-site dressing. Int J Mol Sci. 2011;12:5031-8.
- [Google Scholar]
- Systematic review of skin graft donor-site dressings. Plast Reconstr Surg. 2009;124:298-306.
- [Google Scholar]






