Translate this page into:
The Clinical Pattern of Axillary Hidradenitis Suppurativa among Saudi Arabians: Mode of Presentation and Treatment Challenges
Address for correspondence: Bader Hamza Shirah, King Abdullah International Medical Research Center, King Saud bin Abdulaziz University for Health Sciences, P.O. Box: 65362, Jeddah 21556, Saudi Arabia. E-mail: shirah007@ksau-hs.edu.sa
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Hidradenitis suppurativa is a chronic follicular occlusive disease affecting the folliculopilosebaceous unit. The clinical course is variable, ranging from mild to severe cases. Definitive evidence-based guidelines for the management are lacking. In addition, the multifaceted clinical features and the unpredictable course of the disease make a uniform approach to treatment impractical. As a result, there are multiple therapeutic approaches. Therefore, in this study, we aim to analyze the results of management of axillary hidradenitis suppurativa among the local community in Saudi Arabia.
Materials and Methods:
A retrospective cohort database analysis of 1369 patients diagnosed and treated for axillary hidradenitis suppurativa between January 2004 and December 2013 was done. Seven hundred and forty-one (54.12%) were females and 628 (45.87%) were males. All patients with Stage I disease favored the conservative method while all patients with Stage II chose the surgical approach.
Results:
The mean age was 25.5 years. Nine hundred and seventy-four (71.15%) patients were treated conservatively; the mean healing time was 5.5 weeks. Three hundred and ninety-five (28.85%) patients were treated surgically. One hundred and fourteen (28.9%) had incision and drainage, 281 (71.1%) had complete excision; all wounds eventually healed without significant scarring. The recurrence rate was 12.5% (122 patients) in the conservative method group and zero (0%) in the surgical method group.
Conclusions:
Hidradenitis suppurativa remains a challenging clinical condition for patients and physicians. Further studies need to focus not only on the etiology of this disease but also on the optimal treatment regimen. Public awareness programs are necessary to avoid late presentation and complications.
Keywords
Hidradenitis suppurativa
conservative treatment
Saudi Arabian
surgical excision
INTRODUCTION
Hidradenitis suppurativa is a chronic recurrent cutaneous inflammatory disease that affects the apocrine glands and hair follicles of the intertriginous areas, caused by occlusion of the follicular epithelium. It can present as a recurrent simple cutaneous infection or as recurrent attacks of discharging sinuses with abscess formation in the severe form, mainly in the skin folds that possess terminal hairs and apocrine glands. It can become a chronic disabling disorder that aggressively progresses, causing keloid scars, contractures and immobility. The chronicity and scarring effects of the disease usually lead to substantial impact on the patient's quality of life.[123]
It can affect any body surface area where apocrine glands are present, but most commonly the skin of the axillae and inguinoperineal regions are involved. The incidence is reported as approximately 1%. It is usually painful and disabling, and often worsens over time. Females are more prone than males. Patients are usually post-pubertal.[45]
The pathogenesis is poorly proven; it is postulated that an obstruction of the apocrine and follicular holes result in dilatation of the glands followed by bacterial infection and gland rupture spreading the infection all through the planes of the subcutaneous tissue. As a consequence, hidradenitis suppurativa could manifest as a chronic painful abscess, multiple foul smelling sinus tracts, fibrotic tissue and scar formation. As the abscesses progres deeper in the subcutaneous tissue, single or multiple communicating tracts may develop, which can result in the formation of irregular hypertrophic scars.[678] Rarely, the chronicity may result in a malignant transformation to squamous cell carcinoma.[9]
Bacterial infection is considered a secondary occurrence in the pathogenesis. Many clinical studies have isolated different bacterial species, such as Staphylococcus aureus, Staphylococcus epidermidis, and Corynebacterium species. A polymicrobial anaerobic microflora comprising strict anaerobes, actinomycetes, and Milleri group streptococci was found in about 24% of abscesses or nodules and 87% of chronic suppurating lesions.[101112]
Definitive evidence-based guidelines for the management are insufficient due to a paucity of high-quality data. Furthermore, the multifaceted clinical features and the unpredictable course of the disease make a uniform approach to treatment impractical. As a result, there are multiple therapeutic approaches to this disease.[12345678910111213141516171819202122232425]
Hidradenitis suppurativa is under-reported in Saudi Arabia, evident by a thorough literature search. In the past few years, we encountered an increase in the number of clinical presentations and referral of cases by different specialities, mainly in the young female population. Therefore, in this study, we aim to analyse the clinical pattern, treatment options, and the results of management of axillary hidradenitis suppurativa among the local community in Saudi Arabia.
MATERIALS AND METHODS
A retrospective cohort database analysis of the digital files of 1369 patients who were diagnosed and treated for axillary hidradenitis suppurativa between January 2004 and December 2013 was done. The study was part of the quality care programme for improving the medical care provided to the patients in Al Ansar General Hospital, Medina, Saudi Arabia. It was approved by the hospital Scientific Ethical Committee and the subcommittee for management guidelines and clinical pathway. A digital constructed clinical pathway form was unified to all the patients and attached to the medical record of each patient.
The diagnostic work up, conservative treatment, surgical procedures and follow-up were carried out by the same surgical team in a referral general public health hospital in Medina, Saudi Arabia, serving a population of about 1.2 million citizens of Al-Madinah Al Monawarrah region.
All the study patients were selected from the outpatient clinic and all presented with Stage I and II. All the patients were reviewed at the initial presentation regarding the symptoms, duration of the disease, previous treatment modalities, co-morbid disease, smoking, personal hygiene habits, armpit shaving methods and the use of deodorants.
The treatment options were discussed carefully with all patients. All patients who presented with Stage I disease favored the conservative method, whereas all patients who presented with Stage II chose the surgical approach.
The conservative treatment protocol included three times per day washing the affected area with antibacterial soap, application of warm compresses for 10 min, followed by application of topical sodium fusidate 2% ointment.
All patients who preferred the surgical option had pre-operative workup (complete blood count, coagulation profile, blood chemistry, chest X-ray and electrocardiogram). Ultrasound of the axilla was done to locate the deep lesion for the precise incision and drainage and to outline the involved areas to minimise tissue loss for the complete excision cases.
The surgical procedures were performed according to the complexity of the case. Simple incision and drainage (transverse axillary incision from medial to lateral side over the abscess area with the digital opening of all abscess pockets) and oral antibiotics (clindamycin 300 mg twice daily) were performed for the uncomplicated cases. Total excision (elliptical transverse axillary tissue preserving excision– including all affected tissue in one mass followed by tension-free primary closure subcuticular using 3–0 vicryl sutures) and oral antibiotics (clindamycin 300 mg twice daily) for the complicated cases. All the procedures were done under local anaesthesia.
Follow-up for all patients was done at the outpatient clinic once every week until complete healing, once every month for the following 3 months to check for recurrence, and once every 3 months for 1 year. All patients were given an open clinic appointment whenever recurrence occured. All the patients completed 2 years of follow-up and no drop out recorded.
As part of the clinical review of our quality care programme, the digital database files were collected and analysed. A statistical software SPSS version 22 (IBM Corp., Armonk, NY, USA) was used for data analysis. Results were represented by absolute percentages, average and mean.
RESULTS
Between 2004 and 2013, 1369 patients who were diagnosed and treated for axillary hidradenitis suppurativa were included in the study. Seven hundred and forty-one (54.12%) were females and 628 (45.87%) were males. Female to male ratio 1.18:1. The overall number of patients treated in our hospital during the same period was 1,989,648 patients. Therefore, the incidence rate of axillary hidradenitis suppurativa was 0.07%.
The mean age was 25.5 years, range 14–37 years. The age group showed that 506 (36.96%) were below 20 years old (the youngest was 14), 643 (46.96%) were between 20 and 30 years, 220 (16.1%) were between 31 and 40 years; (the oldest was 37). The majority of patients, 973 (70%) were citizens of Medina city, whereas 396 (30%) were referred from towns and villages of Al Madinah Al Monawarrah region.
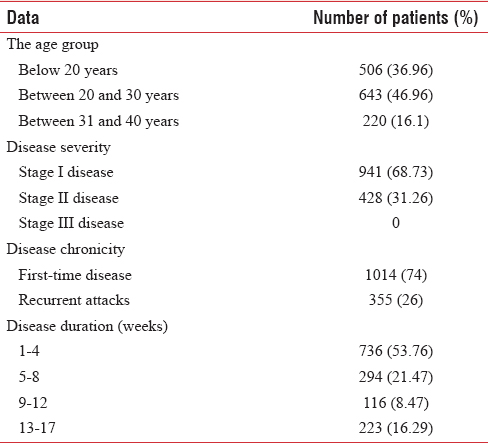
Nine hundred and forty-one (68.73%) patients presented with Stage I disease, whereas 428 (31.26%) presented with Stage II disease, no Stage III disease was recorded. One thousand and fourteen (74%) patients reported first time disease, whereas 355 (26%) had recurrent attacks that were conservatively treated (antibiotics and herbal creams). The mean duration of the disease was 9 weeks, range 1–17. It showed that 736 (53.76%) patients had the symptoms for 1–4 weeks, 294 (21.47%) for 5–8 weeks, 116 (8.47%) for 9–12 weeks and 223 (16.29%) for 13–17 weeks [Table 1].
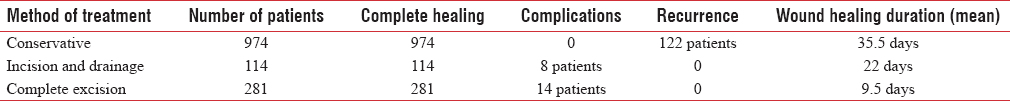
Nine hundred and seventy-four (71.15%) patients were treated conservatively, 261 (26.8%) of them had complete healing within 2 weeks, 528 (54.21%) within 3 weeks, 147 (15.1%) within 4 weeks, and 38 (3.9%) required more than 4 weeks. The mean healing time was 35.5 days, range 2–9 weeks.
Three hundred and ninety-five (28.85%) patients were treated surgically. One hundred and fourteen (28.9%) had an incision and drainage; wound healing duration mean was 22 days, range 18–26 days, 8 (2%) had hypertrophic scar treated conservatively while 387 (98%) healed nicely.
Two hundred and eighty-one (71.1%) had complete excision; wound healing duration mean was 9.5 days, range 8–11 days, 14 (4.98%) had wound infection treated with topical and systemic antibiotics, all wounds eventually healed without scarring [Table 2].
The most common isolated organism from the tissue samples or the abscess cultures was S. aureus in 127 (32.2%) patients. S. epidermidis was found in 86 (21.8%) patients. Multiple species were found in 182 (46.1%). Tissue samples showed a sterile result in 93 (33.1%) of the total 281 patients who had surgical excision.
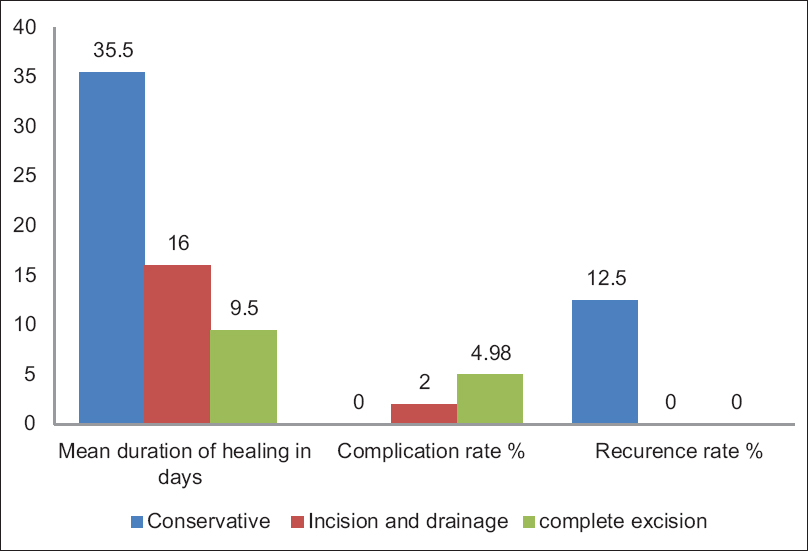
The recurrence rate was 12.5% (122 patients) in the conservative method group; all were retreated conservatively, whereas in the surgical method group, the recurrence rate was zero (0%) [Figure 1].
- Comparison between the treatment modalities
Three hundred and eighty-four (28%) patients were smokers, 279 (72.66%) were cigarettes smokers, 105 (27.34%) were shisha (waterpipe) smokers. Smoking was statistically found to represent a significant difference in the recurrence of the disease, (P < 0.05).
Regarding body hygiene habit, 152 (11%) patients reported daily body shower pattern, 264 (19.3%) every 2 days, 285 (2%) every 3 days, 407 (29.7%) every week and 261 (19%) reported no regular habit. Poor body hygiene was statistically found to represent a significant difference in the development, and the recurrence of the disease, (P < 0.05).
Armpit hygiene results showed that 759 (55.5%) patients used a sharp razor, 231 (16.9%) used molded sweet syrup (traditional Arabian method), 197 (14.4%) used scissors, 160 (11.7%) used creams and 22 (1.6%) did not use to shave at all. Sharp razor shaving was statistically found to represent a significant difference in the development of the disease, (P < 0.05).
Eight hundred and six (58.9%) patients reported regular habit of using deodorants. Regular use of deodorants was statistically found to represent a significant difference in the development of the disease, (P < 0.05) [Figures 2 and 3].
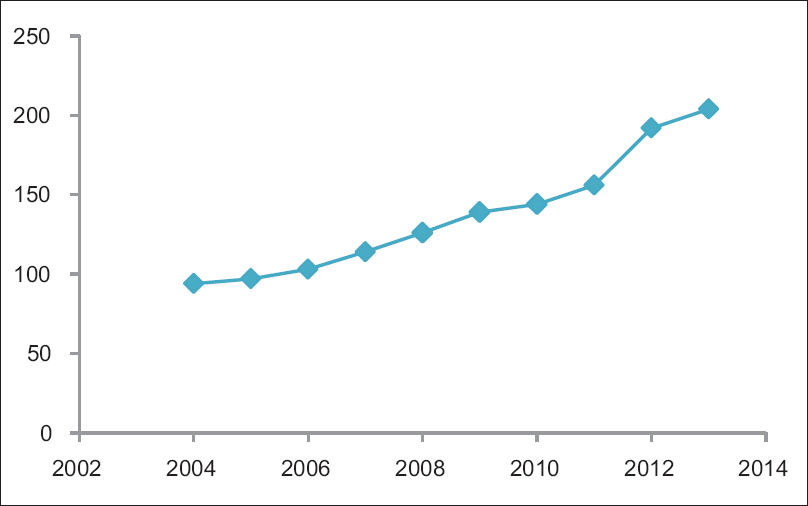
- The annual increase in presentation of axillary hidradenitis suppurativa in Saudi Arabian patients

- Stage II axillary hidradenitis suppurativa in a 32-year-old Saudi Arabian female, before (left) and after complete excision surgical treatment (right)
DISCUSSION
Hidradenitis suppurativa is a challenging clinical condition for the patient as well as the treating physician. It is not life-threatening, but the pain, odour, drainage and disfigurement associated with it regularly have deleterious effects on the patient quality of life. Patients could occasionally experience feelings of sadness or depression related to the disease, and sense of shame may contribute to self-imposed social isolation.[1415] In our series, most of the patients clearly stated that the social factor was an important reason to seek treatment, especially among females.
It is common in women; the reported female to male ratio is 3.3:1.[12345678] While it was 1.18:1 in our study. This also shows a female predominance, but, less than the international figure, which could be explained by the observation we noticed in our local community that females in general, and teenagers in particular, feel shy to seek proper medical help when affected. About 24% of our young female patients confirmed that by admitting no intention to seek medical treatment; parents decision was the main reason for presenting to the clinic. This observation clearly indicates the necessity of a broad spectrum nationwide awareness programme in our Saudi Arabian community.
The age at onset is often reported in the 20–30 year age group,[23] which was similar to our study population (14–37 years). In the recent few years, we observed an increase in the incidence in the female, young teenage group (14–18 years), with almost 100% association of sharp razor shaving of the armpit and deodorants use. Therefore, we strongly recommend a national awareness program in females elementary and high schools targeting those teenagers early in their lives.
Unfortunately, hidradenitis suppurativa is often mismanaged because of the difficult early diagnosis, chronicity, complexity and progression.[1234567891011121314151617181920] We observed that more than 50% of our patients had a history of previous episodes of misdiagnosis and treatment done by many health care practitioners at their local premises. Hidradenitis suppurativa is a clinical diagnosis; no specific test is well established. Therefore, high clinical suspicion is mandatory.[1011121314] Consequently, due to the variable clinical manifestations and the multiple sites involved by the disease, most of the patients with hidradenitis suppurativa may present to or are referred to many different medical specialities, including medicine, surgery, gynaecology, dermatology, plastic surgery, immunology and primary care.[15161718]
Among our local community, traditional herbal practitioners are still treating a good number of patients. In fact, many patients in our series reported experiencing one or two traditional Arabic herbal modalities of treatment before seeking medical care. An issue that should be thoroughly taken care of by healthcare officials and medical professionals for analysing the methods used and legalising such practice.
According to Hurley's Staging System,[19] Hidradenitis suppurativa can be classified into three clinical stages. Stage I: Formation of abscess, single or multiple lesions, without scarring and sinus tracts. Stage II: Recurrent abscesses associated with sinus tracts and multiple scarring; the presence of a single or multiple separated lesions. Stage III: A diffuse or almost diffuse involvement or multiple interconnected tracts and abscesses. The mode of presentation in our study was in accordance to that reported in the literature, and the severity was within Stage I and II. No patient presented with the Stage III despite the fact that a good number of our study population were referred from rural areas (small towns and villages) where the level of health service providing and education is not that optimum. The explanation to that is the health system guidelines in our community where most of the Stage III cases are referred to plastic surgery subspecialty.
The best treatment of hidradenitis suppurativa must provide a high cure rate, a low recurrence rate, minimal inconvenience and loss of work time. Medical management is recommended in early stages while surgery should be performed following the formation of abscesses, fistulas, scars and sinus tracts.[2021] The most common reported treatment for the early-stage cases could be summarised into topical (clindamycin) or systemic antibiotics (tetracycline, clindamycin and rifampicin), topical antiseptic solutions and intralesional corticosteroids (triamcinolone acetonide), systemic retinoids (isotretinoin and etretinate), antiandrogen therapy (cyproterone acetate, finasteride), immunotherapy (tumor necrosis factor alfa inhibitors and more recently, adalimumab), oral immunosuppressive therapy (cyclosporine). All had shown a positive effect on the disease progression.[2225]
Many conservative treatment protocols, incision and drainage, and the surgical removal of the abscesses and fistulas are usually ineffective for definitive cure. The success rates of any medical modality are often limited due to the high rate of recurrence and the indolent nature of the disease. Total surgical excision of the involved follicles and inflammatory process is the only curative treatment proven clinically.[2021222324] For most cases, radical surgery can be the only curative treatment option in the early stages.[26] It was reported that the early wide surgical excision is necessary and efficient to prevent many complications, lower the recurrence rate, and to improve the quality of life.[27] In our surgical protocol, we used ultrasound to locate the lesions and precisely plan the excision to minimise tissue loss. It was a key point in the tension-free wound closure and the cosmetic result in all the patients.
During 20 years of clinical practice, we had very good results in treating superficial surgical infections (cellulitis, carbuncles and blisters) with fusidic acid, which is why we chose it in our conservative protocol. The results of 100% initial success rate with a subsequent low recurrence rate (12.5%) were a good result. Recently, we published a paper about our results using fusidic acid in treating hidradenitis suppurativa; the results were very encouraging.[28]
Simple treatment modalities have been implemented worldwide. They include the avoidance of prolonged exposure to heat and humidity (like Saudi Arabia's climate most of the year), the avoidance of shaving if irritation occurs, the avoidance of tight, synthetic clothing near affected area, the use of topical antiseptics and antibacterial soap, the application of warm compresses, warm baths and hydrotherapy are among the conservative modalities. Weight loss has been reported to be of benefit. The help of non-narcotic analgesics was also recommended.[202122] We observed that patient's counselling regarding those factors played a significant role in improving the management in our local community, in fact, positive changes in personal habits and hygiene were well noticed.
We found that in our community, Grade I disease is more prevalent in young age groups compared to older age groups in Grade II and III. We believe that young people are keener to seek medical help when developing such infections, either self-influenced or parental guide while the elderly would prefer the traditional herbal modalities, which usually fail until the disease reaches a late stage. As a result, we developed a recommendation memorandum to the health officials in the ministry of health endorsing the importance of a nationwide awareness programme.
Although many exogenous factors such as the use of deodorants and shaving are believed to be causal, they have not been proven to be significantly responsible for developing hidradenitis suppurativa.[16] Obesity is reported as an exacerbating factor, and weight loss can help control the disease severity.[18]
Among our study population, 384 (28%) patients were smokers, all of them were males, and all the patients who had recurrences were smokers. Smoking was reported to be strongly associated with hidradenitis suppurativa; smokers are more severely affected than non-smokers.[17] Nicotine promotes follicular plugging.[25]
Hirsutism, low level of body hygiene, sharp razor shaving of the armpit, and the use of deodorants were well noticed in our study, and the proper social and clinical counseling provided to our patients played a significant role in patients behaviour change which was a keystone in the management.
Recurrence rates could be lower with aggressive surgery, but recurrences often continue. After radical excision, the disease has been reported to recur in 33% of patients.[15] In our study, the recurrence rate was 12.5% (122 patients) in the conservative method group, which is within an acceptable range. While in the surgical method group, the recurrence rate was zero (0%) which can be attributed to the mild to moderate severity of the disease in that group, in addition to the proper post-operative care, change of personal hygiene and compliance in avoiding deodorants.
Most of the patients in the conservative method group reported that washing the affected area with antibacterial soap on the 1st day of therapy was associated with a mild burning sensation which disappeared by the third or the 4th day. We attributed that to the degree of inflammation which eased as the effect of fusidic acid started to control the pain and the other manifestations of the infection.
The daily, gentle cleansing of affected areas may help to reduce odour and the occurrence of secondary infection. We advised the patients to use a gentle cleanser and to wash carefully with only their fingers. Scrubbing with washcloths, loofahs, or brushes causes unnecessary trauma and irritation. If malodor is a problem, daily use of an antibacterial cleanser or soap to reduce bacterial colonization on the skin may be of benefit.
Factors that promote follicular maceration and follicular trauma may contribute to worsening of hidradenitis suppurativa due to the promotion of inflammation, follicular occlusion, and follicular rupture. We advised the patients to wear loose, light clothing and to avoid actively excessive heat, friction and shearing trauma.
Since hidradenitis suppurativa is a psychologically distressing disorder that can have a significant impact on patient quality of life,[26] patient education and support are essential components of management. The clinician should inquire about the implications of the disease on the patient's quality of life and assess for symptoms of depression. Patients should be offered resources for psychological support.
Most of our patients presented with low to intermediate level of personal hygiene, average socioeconomic status, mild to moderate level of medical awareness, and a good number were referred from rural areas. However, patient compliance, the strict adherence to the management protocol, and the change of personal habits were major contributing factors to the excellent results achieved. This observation clearly illustrates the importance of individual social counseling of the patients affected by hidradenitis suppurativa in addition to other forms of treatment.
Given our study results, we believe that more clinical studies need to be designed to explore the challenges of managing hidradenitis suppurativa among Saudi Arabians with a particular focus on the social factors, demographic analysis, and the treatment options. Public awareness programmes are strongly recommended, particularly for the young female age group.
CONCLUSIONS
Hidradenitis suppurativa remains a challenging clinical condition for the patients and physicians. Due to the shortage of research trials comparing different treatment options, the choice of the treatment modality should depend on the patient's circumstances and preferences, the outcome of previous treatments, the experience of the physician and surgeon, and the chronicity and severity at presentation. Further clinical research needs to focus not only on the etiology of this disease but also on the optimal treatment regimen. Public awareness programs are necessary to avoid late presentation and complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Surgical treatment of hidradenitis suppurativa: Case series and review of the literature. Int Wound J. 2006;3:159-69.
- [Google Scholar]
- Surgical approach to extensive hidradenitis suppurativa in the perineal/perianal and gluteal regions. World J Surg. 2009;33:481-7.
- [Google Scholar]
- Surgical treatment of hidradenitis suppurativa: A 10-year experience. Surgery. 2005;138:734-40.
- [Google Scholar]
- Hidradenitis suppurativa: A frequently missed diagnosis, Part 1: A review of pathogenesis, associations, and clinical features. Adv Skin Wound Care. 2015;28:325-32.
- [Google Scholar]
- Hidradenitis suppurativa: A retrospective study of 846 Dutch patients to identify factors associated with disease severity. J Am Acad Dermatol. 2014;71:460-7.
- [Google Scholar]
- Hidradenitis suppurativa: Pathogenesis and management. Br J Plast Surg. 2003;56:451-61.
- [Google Scholar]
- Clinical characteristics of a series of 302 French patients with hidradenitis suppurativa, with an analysis of factors associated with disease severity. J Am Acad Dermatol. 2009;61:51-7.
- [Google Scholar]
- Hidradenitis suppurativa complicated by squamous cell carcinoma and paraneoplastic neuropathy. Am J Med Sci. 2005;329:150-2.
- [Google Scholar]
- Clinical features and patient outcomes of hidradenitis suppurativa: A cross-sectional retrospective study. J Cutan Med Surg. 2016;20:52-7.
- [Google Scholar]
- An update on medical treatment options for hidradenitis suppurativa. Drugs. 2016;76:215-29.
- [Google Scholar]
- Bacterial pathogens associated with hidradenitis suppurativa, France. Emerg Infect Dis. 2014;20:1990-8.
- [Google Scholar]
- Prevalence and factors associated with hidradenitis suppurativa: Results from two case-control studies. J Am Acad Dermatol. 2008;59:596-601.
- [Google Scholar]
- Depression in patients with hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2013;27:473-8.
- [Google Scholar]
- The role of depilation and deodorants in hidradenitis suppurativa. Arch Dermatol. 1982;118:101-2.
- [Google Scholar]
- Objective scoring of hidradenitis suppurativa reflecting the role of tobacco smoking and obesity. Br J Dermatol. 2009;161:831-9.
- [Google Scholar]
- Axillary hidradenitis suppurativa: A further option for surgical treatment. J Cutan Med Surg. 2004;8:6-10.
- [Google Scholar]
- Soluble interleukin-2 receptor serum level is a useful marker of hidradenitis suppurativa clinical staging. Biomarkers. 2009;14:432-7.
- [Google Scholar]
- Long-term infliximab for severe hidradenitis suppurativa. Br J Dermatol. 2006;155:1105-7.
- [Google Scholar]
- Hidradenitis suppurativa: A treatment challenge. Am Fam Physician. 2005;72:1547-52.
- [Google Scholar]
- The natural history of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2000;14:389-92.
- [Google Scholar]
- Topical clindamycin versus systemic tetracycline in the treatment of hidradenitis suppurativa. J Am Acad Dermatol. 1998;39:971-4.
- [Google Scholar]
- Pharmacologic interventions for hidradenitis suppurativa: What does the evidence say? Am J Clin Dermatol. 2012;13:283-91.
- [Google Scholar]
- Surgical treatment of hidradenitis suppurativa. Scand J Plast Reconstr Surg Hand Surg. 2001;35:305-9.
- [Google Scholar]
- Effective modified conservative tissue preserving protocol to treat stage I axillary hidradenitis suppurativa: A prospective cohort study of 627 patients with five years follow-up. J Dermatolog Treat 2017:1-6.
- [Google Scholar]






