Translate this page into:
Standardization of SMP Procedure and Its Impact On Outcome
Address for correspondence: Dr. Sujit J.S. Shanshanwal, Department of Dermatology, OPD 16, 2nd Floor, New OPD Building, L.T.M.M.C. and Lokmanya Tilak Municipal General Hospital, Sion Hospital, Mumbai, Maharashtra, India. E-mail: shanshanwal.sujit@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Cosmetic deformities can result from various types of alopecia or even post hair transplantation procedures. Patients with such deformities seek aesthetically appealing longer-lasting options. Scalp concealers are commonly used by men and women to camouflage these deformities. Scalp micropigmentation (SMP) is one of the concealers recently gaining popularity.
Objectives:
SMP is a novel technique wherein microdot tattoos are placed in a stippling pattern to mimic hair follicles that are cut close to the scalp and various variables affecting its outcome were evaluated.
Methods:
Forty-five subjects were recruited for the study. The various factors affecting outcome of SMP—angle of needle against the scalp, depth of needle into the scalp, time of the needle contact in scalp, speed of the rotor, resistance of scalp, color of pigment, viscosity of dye, needle number, needle thickness, and pattern of dot placement—were systematically studied in 15 patients through clinical photographs and trichoscopy. Ideal depth of pigment deposition was assessed through histopathological examination. After using these optimum variables, standardized SMP was performed in 30 patients with hair loss (3 patients with cicatricial and 27 patients with diffuse non-cicatricial alopecia). SMP was also used to create an aesthetically denser hairline. The outcome of the procedure was evaluated using standardized global photographs.
Results:
The ideal parameters were established to achieve standard reproducible results. There were great patient satisfaction and acceptance of the procedure. All the patients showed moderate to great improvement after the procedure with satisfactory scalp coverage. Adverse events were transient which were seen in the form of edema and redness.
Conclusion:
SMP offers a non-medical, tattoo-based cosmetically appealing and effective “cover-up” that hides the unsightly conditions. The cosmetic tattoo placement creates an illusion of thicker hair.
Keywords
alopecia
hair
illusion
micropigmentation
scalp
SMP
BACKGROUND
With increasing hair loss, there is a decrease in density of hair, and as a result, the scalp skin can be seen easily due to increase in contrast between hair and skin. This contrast between the hair and skin can be minimized by providing an illusion using various camouflaging or concealing techniques. Camouflaging techniques such as bio fibers and wigs, or concealers such as hair powder are all temporary methods with their own shortcomings. Compared to these modalities, tattooing is a permanent concealer and thus has a pivotal role to play in such patients. Scalp micropigmentation (SMP) is an art in the form of stippled painting. Tattooing involves implantation of exogenous metabolically inert colorfast pigments into the skin. SMP is a sophisticated method of placing microdots less than 1 mm in size using one- or three-pronged needles, creating an illusion of hair by decreasing contrast between hair and skin. The process is performed using manual or electrically driven needles, whereby only pigment particles introduced through the skin surface, below the dermal–epidermal junction, are retained by the dermal macrophages and fibroblasts where they reside permanently, producing an indelible change of the skin color in the form of a recognizable pattern or design.[12] The terms “micropigmentation” and “dermatography,” which are both coined recently, convey the aesthetic use of tattooing for medical purposes. SMP is not as simple as body tattooing due to the difference in the anatomy of the scalp skin compared to the rest of the body.
Historical Aspects
Skin marking with pigments has been used by people for at least 4,000 years.[3] Tattoos have been found on Egyptian mummies as an indication of worship to a god, and Roman gladiators are known to have used tattoos for identification.[1] In the first half of the 20th century, tattooing was considered fashionable among royalty.[4] The first papers to document unequivocally medical application of tattooing in dermatology and ophthalmology appeared by the mid-1800s.[567] The word “tattoo” itself was introduced by Captain Cook (1796), who wrote of the Polynesian practice of inlaying black pigments under the skin, known popularly as “tattow” in their native language.[8] During the past several decades, however, the public perception of tattooing has greatly evolved. Popularity of tattoos and other types of body art, such as piercing, has dramatically increased, especially among adolescents and young adults.[1] The first reported use of micropigmentation on the scalp was in 2001 by Traquina who reported the results of micropigmentation performed in 62 patients with scalp scars.[9] However, this method was crude and the pigmentation was quite detectable. Since then, the procedure of micropigmentation has greatly refined over time.
SMP is a process of intricate maths and science, the outcome of which depends on several variables. The purpose of this article was to create awareness about SMP among plastic surgeons and dermatologists to more readily perform this procedure in patients with hair loss.
Aims and Objectives
-
To study variables and establish optimum parameters that influence the outcome of procedure when performing SMP.
-
To assess response to SMP in patients with hair loss.
MATERIALS AND METHODS
SMP was performed with a specialized medical tattoo machine using alcohol-based tattoo ink. Fifteen volunteers with hair loss were initially recruited for standardization of SMP protocol after taking consent for the procedure. They were advised to avoid taking aspirin, nonsteroidal anti-inflammatory drugs, vitamin E, Ginkgo biloba, and ginseng 1 week prior to the procedure. The procedure was performed without using local anesthesia. The area was cleaned and prepped. The pigment was taken in the plastic well and the conical tip of the activated handle was dipped into the ink whereby the ink was sucked into the chamber around the needle by capillary action.
The procedure was now performed with different parameters of each of the following variables and its impact on the outcome was assessed:
Angle of the needle to skin: needle insertion at different angles.
Depth of needle: insertion at varying depths ranging from 0.3 to 1.2 mm.
Pattern of pigmentation: placement of pigment in regular versus random manner.
Tattoo ink used: jet black versus black-brown in a ratio of 2:1.
Contact time of needle: different contact times with its correlation to pigment deposition.
Resistance of scalp: effect of skin suppleness/elasticity/turgidity on pigment deposition.
Speed of rotor: impact of varying rotor speed on pigment deposition.
Viscosity of dye: fluidity of dye impacting outcome.
Needle number: Single-pronged needle was used for hairline designing and triple-pronged needle for the rest of the scalp.
To ascertain the ideal depth of pigment deposition, 1-mm scalp skin biopsy specimen was obtained from the tattooed target site a month after the procedure.
After deriving the optimum parameters for the aforementioned variables, SMP was performed as a standardized procedure in 30 patients with hair loss with cicatricial as well as noncicatricial alopecia. The improvement was graded on global photography with a 7-point rating scale (−3 to +3). Subjective evaluation was conducted on a patient satisfaction scale of 0–3. Both these evaluations were conducted after completion of 6 months after the procedure.
Trichoscopy was used for gauging proper placement of dots. Immediately after the procedure over a test patch, the excess dye was wiped and examined with a dermatoscope. For ideal placement, some dye should be visible in the underlying dermis when seen through a polarized dermatoscope.
After the procedure, petroleum jelly was applied over the treated area and patients were advised not to wash it for 48 h. The results were evaluated at 1 and 6 months.
RESULTS
Standardization of SMP procedure was acquired from the result obtained by studying the change in results with the change in variable.
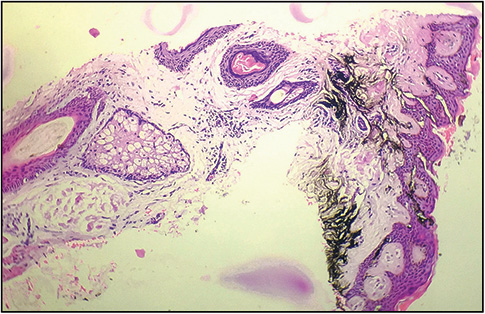
When the needle was placed perpendicular compared to at an acute angle, it resulted in round dots compared to oval dots. The hematoxylin and eosin stained sample of skin biopsy specimens showed pigment deposition in the epidermis at needle insertion of 0.3 mm, in the upper dermis with a depth of 0.7 mm and in the deeper dermis with a length of 1.0 mm. Optimum pigment deposition in the skin was seen when the speed of the rotor was adjusted to 5500–6500 cycles per minute and the time of needle-to-skin contact was 0.5–1.0 s. However, the speed was increased to 7000–8000 cycles per minute when targeting cicatricial patches due to increased resistance of the skin. The single-pronged needle gave a natural look of hairline with finer dots mimicking single follicular units and triple-pronged needles provided a filling effect in the rest of the scalp. Placement of dots linearly gave an unnatural look compared to random placement which mimicked natural hair follicular openings. It was noticed that when dye was watery in consistency, the pigment deposition was inadequate. The retention of pigment was much better when plain black dye was used, whereas the brown-black mix dye was washed away from the skin 1 month after the procedure.
Standardized SMP procedure was performed in 30 patients [24 with androgenetic alopecia (AGA), 3 with cicatricial alopecia, and 3 with alopecia areata (AA)]. Of these 24 patients, those with AGA (14 males, 10 females) had unsatisfactory coverage with medical (n = 22) treatment and/or hair transplantation (n = 2). Three patients with AA showed poor response to medical therapy.
Evaluation conducted after the procedure from 1- and 6-month follow-up photographs showed that appreciation of response was most noted in patients with AGA. Two patients with grade V and VI AGA that were unsatisfied after hair transplantation were very pleased with the results of SMP [Table 1]. However, it was noted that the color of the pigment changed from black to bluish gray over 6 months [Figures 1 and 2].

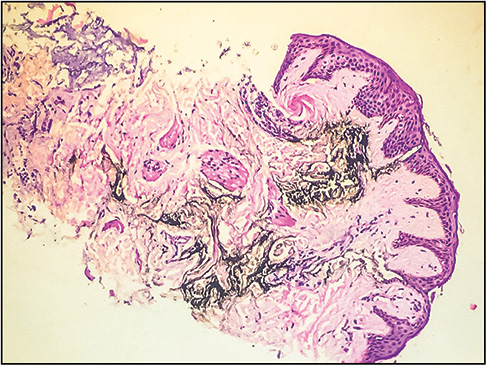
- When the pigment is deposited in deeper dermis, there is diffusion of pigment and results in a blotchy appearance
- Pigment should be placed as high as possible in the dermis. Proper deposition of pigment controls the degree of darkness
DISCUSSION
The utility of SMP is to act as a permanent concealer in such a way that the targeted artistic effect is similar to the visual effect of a stippled painting as dots are created between the pores of a balding scalp. In hair transplantation, surgeons implant 20–40 grafts/cm2, which does not give the natural average hair density of 200 hair/cm2. The density of the stippling does not necessarily match the number of pores that contain the hair in the average adult. As the dots diffuse over time, overcrowding of dots can result in a patchy appearance. Thus, even with hair transplantation as normal density is never reached, SMP can serve as an indispensable tool for providing the illusion of increased density. There are several factors that are important to place the correct amount of pigment, at the correct level, into the scalp for the desired effect.
The various factors include angle of the needle against the scalp, depth of the needle into the scalp, time of the needle contact in the scalp (exposure time), speed of the rotor, resistance of the scalp, color of pigment, viscosity of dye, needle number, pattern of dot placement, and expertise of the operator. The angle of the needle against the scalp skin should be 90°. With a highly acute angle of insertion, the pigment was deposited in a linear manner that resulted in an unnatural look. If the needle is inserted at an angle, it does not result in the formation of round dots. The depth of needle penetration into the skin is a crucial parameter influencing the adequate of placement (deposition) of pigment into the dermis. If the depth is too superficial [Figure 3] (up to the epidermis) then the pigment may not remain in the skin and will be washed off in 3–4 weeks. When the needle was penetrated deep down into the dermis [Figure 4], there was diffusion of pigment into the surrounding skin leading to enlargement of the size of dot giving a patchy appearance over time and also change in color of the pigment. Ideal deposition of pigment is into the papillary dermis [Figure 5]. If the speed of the rotor is high, the surgeon would have to decrease the needle contact time to avoid overdeposition of pigment. If the rotor speed is kept very slow, the needle would not penetrate the skin due to lack of adequate force. Similarly, in certain situations such as in cicatricial alopecia where the skin resistance is high, higher rotor speed is required for penetration into the skin. Various disease processes or scalp surgeries lead to changes in the structure of the skin. Atrophic or scarred skin would not react the same way to pigment deposition as normal skin. In such cases, it is advisable to start with a test patch to get an estimate on the parameters before proceeding to the rest of the scalp. The choice of needle used varies with the target area. A single-pronged needle is used for the area close to the scalp hairline or eyelid tattooing to create fine dots. A triple-pronged needle is used when covering the rest of the scalp. Dots should never be put in a continuous line or regular grid manner. Instead, they should be placed in an irregular pattern, ensuring that the distances between individual dots are maintained. It requires considerable skill and experience of the operator to gauge the feel of resistance and master depth control while performing SMP. The excess pigment that is deposited on the surface of the skin is washed away off during the first hair wash at 48 h after the procedure. Over the course of few weeks, there would be slight softening of the pigment as the epidermal turnover dislodges the keratinocytes with the ink in the epidermal layer. With experience, the operator learns to balance what is seen at the surface at the time the first procedure is performed with an anticipated loss of some of the more superficial epidermal pigments after a number of days pass. It has been observed by the authors that using only black pigment leads to a bluish-green tinge. The bluish-green color of the black or gray pigment is said to be similar to how the red blood vessels appear green under the skin, where the increased absorption of the red spectrum of light gives rise to a phenomenon explained by the trichromatic theory of color vision.[10] Over a period of 8–10 months, there is slight fading of pigment that might warrant a repeat procedure to reinforce the camouflage. It is important to explain to the patient that it will be necessary to dye the hair black on a continuous basis if there are much gray hair. For the same reason, micropigmentation is not recommended for individuals who change their hair color frequently.[10]

- Pre- and post-SMP in a 28-year-old man with androgenetic alopecia who had undergone hair transplantation but was unsatisfied with the results on the recipient site

- Pre- and post-SMP in a 32-year-old man with inactive lichen planopilaris who was unwilling for hair transplantation and wished for other camouflaging options
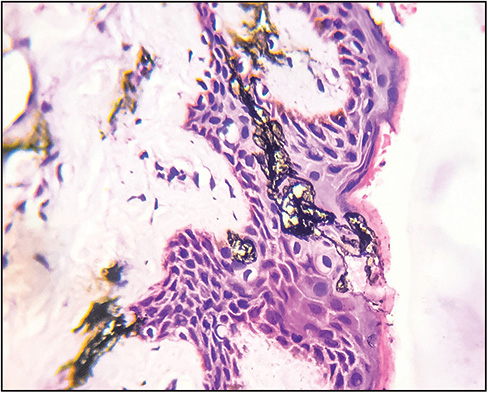
- When the pigment is deposited superficially, it gets washed off soon and does not give the desired effect
SMP is a very useful camouflaging tool to give satisfactory results by augmenting illusion of hair. It is a great therapeutic option for both male and female patients with AGA, posttransplant scars, posthair transplant to further augment results, and cicatricial alopecia (discoid lupus erythematosus, lichen planopilaris, folliculitis decalvans, inflammatory tinea capitis, dissecting cellulitis, central centrifugal cicatricial alopecia, acne keloidalis nuchae, keratosis follicularis spinulosa decalvans). If the scar area is too wide, the results can be further augmented by combining hair transplantation with SMP. SMP has been effectively used in piebaldism.[11] Van der Velden et al.[12] reported excellent response in 30 of 33 patients with AA which also involved the eyebrows.
SMP has a long learning curve and operator needs to understand the intricacies of the procedure. The technical and artistic skills of experienced operator reflect the elegance of the results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
None.
REFERENCES
- Ueber das Feuermaal und die einzig sichere Methode, diease ensteullung zu heilen. J Geburttsh. 1835;15:66-72.
- [Google Scholar]
- Technic of tattooing with mercury sulfide for pruritus ani. Ann Surg. 1942;115:126-30.
- [Google Scholar]
- Basal cell carcinoma arising in tattoos: a clinical report of two cases. Br J Plast Surg. 1983;36:258-9.
- [Google Scholar]
- Micropigmentation as an adjuvant in cosmetic surgery of the scalp. Dermatol Surg. 2001;27:123-8.
- [Google Scholar]
- Micropigmentation: camouflaging scalp alopecia and scars in Korean patients. Aesthetic Plast Surg. 2014;38:199-204.
- [Google Scholar]
- Dermatography as a new treatment for alopecia areata of the eyebrows. Int J Dermatol. 1998;37:617-21.
- [Google Scholar]






