Translate this page into:
Use of the CONUT Index as a Predictor of Integration Of Cutaneous Grafts in Burn Patients
Address for correspondence: Dr. Jaime Aron Garcia-Espinoza, Aldama Street, Tule, San Bartolo Coyotepec, Oaxaca, Mexico. E-mail: jaime_506@yahoo.com.mx
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To present the initial experience of 12 patients with burns treated with cutaneous grafts and to analyse the variables that influence their integration.
Materials and Methods:
We analysed data from 12 patients seen in a year in the regional hospital of high speciality of Oaxaca. Quantified variables: Age, sex, burned body surface, depth of burn, airway injury, nutritional status by CONUT index, type of graft, development of local infection and days of hospital stay.
Results:
We included 10 men (83%) and 2 women (17%) with median age of 28 years, median burned body surface area of 19%, depth: 75% were mixed burns and 25% were third degree; with median time between injury and application of grafts of 13 days, 1 patient presented airway injury and 50% concomitant trauma.
Regarding Nutritional Status:
Fifty percent had severe malnutrition, 33% moderate and 16% mild. About 67% of the grafts were meshed and 33% intact, the mean integration percentage was 80%, 25% developed local infection and the average length of hospital stay was 21 days.
Conclusions:
Cutaneous grafts are the definitive treatment of burns, in their integration process influence different factors, including nutritional status. The CONUT index seems to be a useful, safe and widely available tooling in the nutritional assessment of the burned patient and can be related to the percentage of integration of the grafts and the days of hospital stay.
Keywords
Burn
cutaneous graft
hospital stay
malnutrition
nutrition
INTRODUCTION
Burns are thermal injuries caused by biological, chemical, electrical and physical agents that produce significant local and systemic effects.[1] These types of injuries are relatively frequent and have a greater incidence in economically and culturally marginalised countries. In the United States, 500,000 burn patients are treated each year and about 3500 deaths/year.[2] In 2011 in Mexico, burns ranked 17th in incidence and affected 129,779 patients, men between the ages of 20 and 40 were the gender and the most affected age group. The cost generated by its attention to health services is very high, in Mexico, it is estimated that moderate burns generate an expense between 30,000 and 500,000 pesos per patient; on the other hand, serious burns can reach costs of up to 40 million pesos per patient attended.[3]
Burns induce local and systemic damages that are perpetuated mainly by the lack of skin cover. Systemic changes appear when the affected body surface area is >10% and occur due to severe alteration of homeostasis in response to the release of insulin-counterregulatory hormones that induce hypercatabolic states, humoral and cellular immunodeficiency, water balance disorders, temperature, haemodynamic and nutrient absorption.[4] The care of the burned patient is divided into two phases. Primary care focuses on protecting the airway and providing adequate fluid resuscitation (essential to prevent burn progression and prepare the patient for skin graft application).[56] On the other hand, the secondary care treats the sequelae of the burn and promotes definitive treatment through the application of cutaneous grafts.[7]
Cutaneous grafts are fragments of skin extracted from a donor surface, have no irrigation of their own, require placement on a receiving surface and undergo a complex integration process.[8] This process occurs in phases: The plasma imbibition phase occurs during the first 3 days, in this period the graft captures exudates rich in proteins that favour their survival, and then the inoculation phase where the capillaries align. The revascularisation phase occurs from the 4th to the 8th day, is the product of adequate immobilisation of the graft and a high secretion of endothelial growth factor that induces the formation of blood vessels. Finally, the maturation phase is reached on average after 21 days, at this stage the graft is fully integrated.[9] Graft survival is only possible when placed in an area with adequate irrigation, free of infection, adequate fixation and haemostasis.
The influence of nutrition on the evolution of the burned patient has been demonstrated in different studies, usually the nutritional status is evaluated by the determination of serum albumin; however, it has been shown that it is not useful to predict the evolution of the grafts.[10]
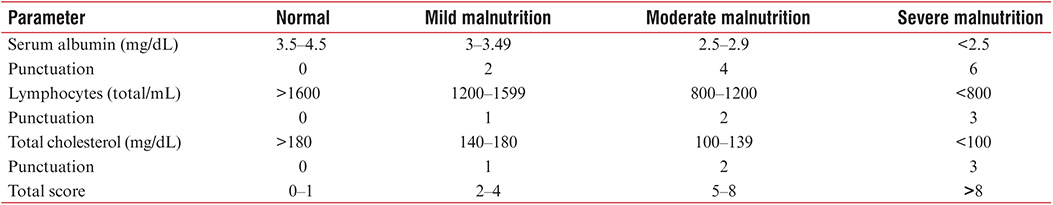
In 2010, a study was published, in which it was found that elevated serum levels of pre-albumin predict a higher percentage of skin integration;[11] however, its use is limited by its availability. Ignacio de Ulíbarri et al. developed a screening tool to assess the nutritional status of hospitalised patients through routine screening (CONUT).[1213] This tool uses two biochemical parameters and one immunological: Total cholesterol, albumin and total lymphocytes; each of them provides a specific score and the result establishes the degree of malnutrition of the patient [Table 1]. In recent years, its high sensitivity and specificity (82%–92.3% and 85%, respectively) have been demonstrated to evaluate the nutritional status of surgical patients, hepatopathies, cardiac patients, among others.[14]
MATERIALS AND METHODS
We included patients who, within a year, entered our hospital diagnosed with deep or second-degree burns and who received grafts as part of the surgical treatment. At admission, burned body surface area (nines rule), depth of burn, concomitant trauma, airway injury and nutritional status (CONUT index) were assessed; we later evaluated the type of graft used (mesh or laminar), time elapsed between burn and graft application, percentage of graft integration at 10 days of follow-up (to estimate the percentage of integration of the grafts, first the measurement was done in cubic millimetres of the burned area to be grafted, and then, we measured the area of tissue integration in cubic millimetres and quantified the corresponding percentage), days of hospital stay from admission to discharge and development of infection of the affected bed (confirmed by cultures of the same). For the sample size, the statistical analysis was performed using non-parametric tests.
RESULTS
We analysed data from 12 patients (10 men and 2 women), with a median age of 28 years with an interquartile range between 19 and 41 years. The age range between 16 and 33 years was the most frequently affected [Table 2].
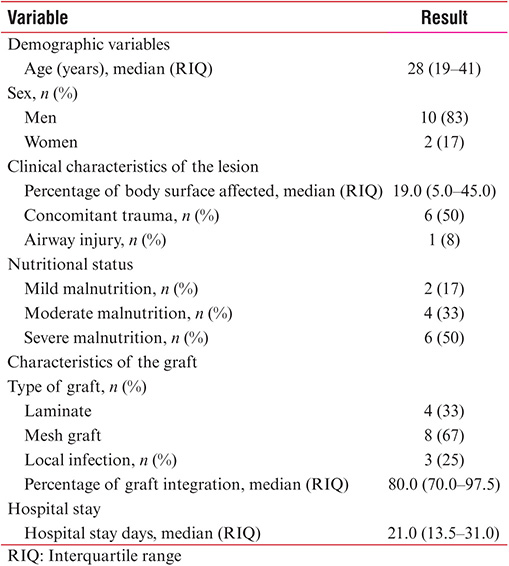
The median body surface area affected was 19.0% (5.0–45.0) and in terms of depth, 75% (8) of the patients had mixed depth burns (50% (6) with superficial/deep second-degree burns and 25% (3) of deep second and third degree) and 25% (3) suffered third-degree burns. As for the mechanism of injury: 42% (5) had burns by flame, 33% (4) by scalding, 17% (2) electric burn and 8% (1) per contact.
Six patients (50%) had concomitant trauma at the time of burn: two patients had moderate traumatic brain injury due to fall of their own height, two patients suffered perineal trauma that required sigmoid terminal colostomy, one of them suffered traumatic amputation of the lower limb [Figure 1], one had a right femur traumatic fracture, and one patient was classified as having an airway lesion due to clinical suspicion (closed area burn, facial area, dysphonia and carbonated sputum) and required immediate intubation in the area of medical emergency.

- Traumatic amputation of the lower limb
In relation to the nutritional status evaluated by the CONUT index, we found that from hospital admission all patients had some degree of malnutrition, mainly severe malnutrition, followed in descending order by moderate and mild malnutrition [Table 2]. All patients received partial thickness grafts, mesh grafts were the most frequently used [Figure 2] and the remainder were laminar grafts [Figure 3 and Table 2]. The median number of days elapsed between the time of the injury and the skin graft placement was 13.0 days (7.0–16.0).

- Mesh graft

- Laminar or integral graft
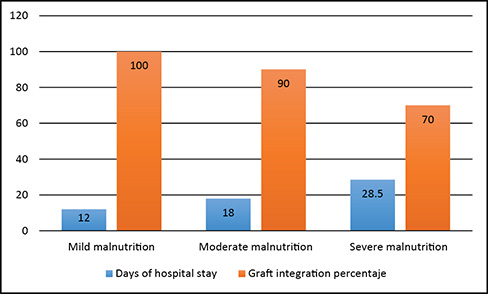
The median percentage of integration of skin grafts after 10 days of placement was 80.0% (70.0–97.5); however, when we performed a stratification of the percentage of integration according to the degree of CONUT malnutrition, we found that the patients with the highest degree of malnutrition had a lower percentage of graft integration [Figure 4]. The median length of hospital stay was 21.0 days (13.5–31.0); similarly, to what was observed with the graft integration, patients who had the highest degree of malnutrition had a higher number of days of hospital stay [Figure 4]. Regarding the development of local infection, we found that a quarter of patients had local infection and all three patients had Pseudomonas aeruginosa isolates in association with Staphylococcus aureus [Table 2].
- Percentage of integration of the graft and days of hospital stay stratified by nutritional status
DISCUSSION
Currently, the definitive treatment of deep or severe second-degree burns is based on the placement of skin grafts; however, to achieve adequate integration of the graft it is necessary to maintain optimal local and systemic conditions that allow an adequate plasma imbibition phase.[15] Tangential excision and early cutaneous grafting are the treatment of choice in deep burns because it minimises fluid loss, reduces metabolic demand, protects the wound from infections, reduces inflammation and prevents multi-organ failure,[16] it is recommended to do so in the first 7 a 14 days with the haemodynamically stable patient, and adequate debridation should be performed with the aim of removing the devitalised tissue and avoiding graft loss, preferring partial-thickness grafts taken with a suitable dermatome. Ong et al. reported that in burned patients treated with skin graft, mortality was 27% compared to 36% in non-grafted patients; this difference was notorious in patients with airway lesions, where mortality was 22% in grafts and 62% in non-grafts.[17]
Early grafting should be performed within the 1st week after the injury to decrease hospital stay and infection rates.[18] There are several factors that influence the correct integration of the graft, among them the nutritional status of the patients. There have been studies that have analysed this factor, in which it has been reported that serum levels of transthyretin or pre-albumin correlates and somehow predicts the integration of cutaneous grafts,[19] however, because of its high cost this marker is not available in all hospital centres.
On the other hand, there are tools such as the CONUT index[1920] that simplify the estimation of nutritional status. The CONUT index uses conventional parameters to estimate the nutritional status of hospitalised patients; this index has not been applied to assess the nutritional status in patients burned and much less has been used as a parameter that evaluated the health and integration of the grafts. In our patients, we observed that those with severe malnutrition (CONUT index) had a lower percentage of graft integration and a longer hospital stay. Despite the limitations of our study, mainly the small sample size, these results are in agreement with previous observations, in which it has been demonstrated that the precarious nutritional status decreases the percentage of integration of the grafts, in addition we consider that the index of CONUT could be an easily accessible to evaluate and predict the integration of the grafts and could even be comparable to the pre-albumin measurement; however, it is obviously necessary to carry out larger studies and a methodology to evaluate these hypotheses.
Regarding surgical site infection rates, the current studies show that colonisation by S. aureus or Acinetobacter spp. is associated with a higher rate of graft loss, in our study, the mean graft integration in this group of patients was less.
An unfavourable result in the evaluation of our patients is the time elapsed between the time of the injury and the placement of the graft since it was greater than the recommended average;[2122] this was due to the concomitant trauma that caused haemodynamic instability and non-optimal haematological parameters for performing tangential excision and graft application.
CONCLUSIONS
The definitive treatment of burns is tangential excision and early grafting since they are the only measures that decrease the metabolic demand, infections, hospital stay and mortality.
The nutritional status is fundamental for the correct integration of cutaneous grafts; the CONUT index can be a useful tool in the prediction of the health status of the graft as well as the percentage of integration thanks to its easy access, lower cost and high sensitivity and specificity. It is necessary to carry out extensive studies to evaluate its usefulness in the clinical evolution of burn patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- American Burn Association Home Page.. Available from: http://www.ameriburn.org
- Skin graft vascularization involves precisely regulated regression and replacement of endothelial cells through both angiogenesis and vasculogenesis. Plast Reconstr Surg. 2006;117:836-44.
- [Google Scholar]
- A reference standard for plasma proteins is required for nutritional assessment of adult burn patients. Burns. 1998;24:337-45.
- [Google Scholar]
- Assessment of the relation between prealbumin serum level and healing of skin-grafted burn wounds. Burns. 2010;36:495-500.
- [Google Scholar]
- CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38-45.
- [Google Scholar]
- Confirming the validity of the CONUT system for early detection and monitoring of clinical undernutrition: Comparison with two logistic regression models developed using SGA as the gold standard. Nutr Hosp. 2012;27:564-71.
- [Google Scholar]
- A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10:1103-8.
- [Google Scholar]
- Standard operating procedures for the clinical management of patients enrolled in a prospective study of inflammation and the host response to thermal injury. J Burn Care Res. 2007;28:222-30.
- [Google Scholar]
- Outcomes of continuous process improvement of a nutritional care program incorporating TTR measurement. Clin Chem Lab Med. 2002;40:1355-9.
- [Google Scholar]
- New procedure for the early detection and control of hospital malnutrition. Nutr Hosp. 2002;17:179-88.
- [Google Scholar]






