Translate this page into:
Extensive Nevus Comedonicus, Complicated with Recurrent Abscesses, Successfully Treated with Surgical Resurfacing
Address for correspondence: Dr. Maheshwari Nallur Siddaraju, #851, Cosmetic Skin Care Clinic, 8th Cross, 8th Block, Koramangala, Bengaluru 560095, Karnataka, India. E-mail: mahe48062@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nevus comedonicus is a rare epidermal abnormality of the pilosebaceous unit, which is congenital in most patients but may also appear early in childhood. It may be localized or have an extensive involvement, the latter showing a unilateral predominance with only a few cases presenting bilaterally. Extensive nevus comedonicus can be associated with musculoskeletal defects, eye and neurological involvement, which constitutes nevus comedonicus syndrome. Uncomplicated nevus comedonicus can be treated with topical keratolytics, diode, erbium laser, and ultrapulse CO2 laser. Surgical excision can be performed to ensure complete removal and nonrecurrence. This case report refers to a young male patient with extensive nevus comedonicus present over left chest, left axilla, and left upper back without systemic involvement, treated with staged surgical excision and resurfacing.
Keywords
Nevus comedonicus
nevus comedonicus syndrome
staged surgical excision
INTRODUCTION
Nevus comedonicus (NC) is an uncommon hamartomatous epidermal abnormality of the pilosebaceous unit, with a reported incidence of 1 in 45,000 to 1 in 100,000.[1] This manifests clinically as giant “blackheads” in the affected areas. Though they may remain asymptomatic for long periods, the deranged anatomy of the pilosebaceous unit [Figure 1] results in an increased incidence of secondary infections; localized lesions can be observed, unless they lead to secondary complications or are cosmetically unacceptable.
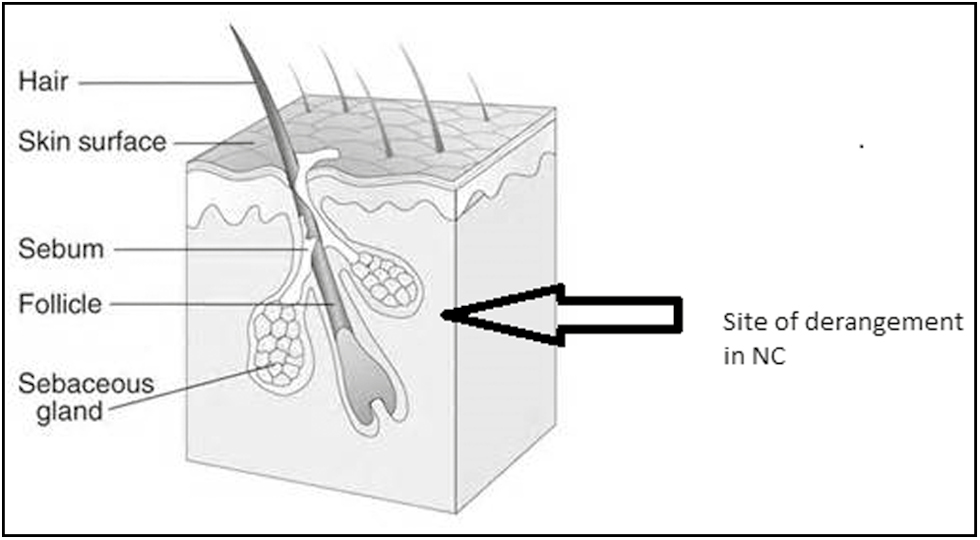
- Anatomy of pilosebaceous unit with site of derangement in NC
CASE REPORT
A 25-year-old male patient presented to the outpatient department with a skin condition present since birth. Being initially smaller in size and localized, the distribution widened during puberty to the present pattern. The patterned lesion was clinically characterized by linearly arranged, grouped acuminate papules with central dark pigmented, keratotic plugs resembling comedones, but much bigger in size. It extended from left anterior chest to left upper back, and included the left axilla and left arm outer aspect. He had recurrent abscesses at multiple locations in the region of the nevus. His symptoms were particularly severe in the left axilla, which was his main complaint [Figures 2 and 3]. He had no family history of similar complaints. He had visited numerous dermatologists for the same, but their treatment, from keratolytics to lasers, was of no avail.

- Linearly arranged nevus comedonicus extending from left anterior chest to left upper back

- Nevus comedonicus involving left axilla complicated with multiple abscesses
The rest of the cutaneous examination was found to be normal.
General physical examination and systemic examination were unremarkable. Special attention was given to ophthalmological, skeletal, and neurological examinations, to rule out NC syndrome, and these too were normal.
After detailed preop workup, he underwent wide local excision of the left axilla skin and subcutaneous fat, down to the level of deep fascia. The resulting defect was resurfaced with a transposition flap from left posterior trunk, and the donor site was skin grafted [Figures 4, 5 and 6]. The surgical procedure was well tolerated and the flap remained fully viable on follow-up. The excised specimen was sent for a detailed histopathological assessment, which confirmed the diagnosis of NC.

- Nevus comedonicus extending over the back

- Local flap planned for transposition
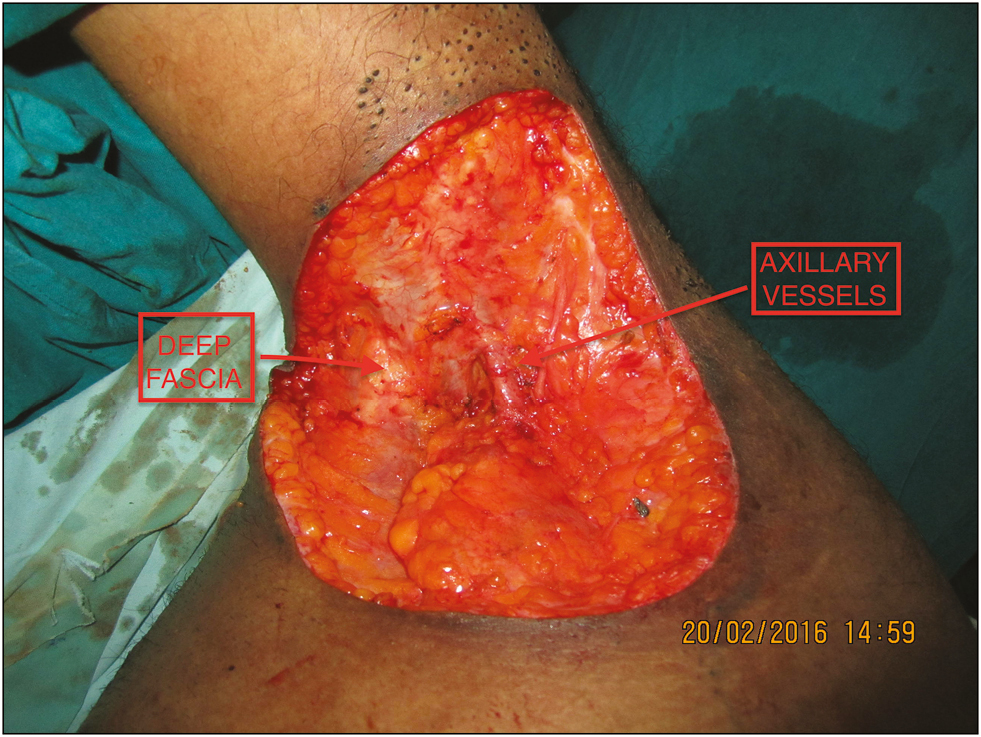
- Wide local excision of the left axilla skin and subcutaneous fat, down to the level of deep fascia
After a 4-month interval, he was taken up for surgery again, wherein he underwent excision of the remaining areas of NC. The anterior chest wall region was then closed primarily, while the posterior and lower axillary chest wall region was covered with a split-thickness skin graft harvested from the thigh [Figure 7]. Once again, he tolerated the procedure well, with the skin graft taking up completely. He was given compression garments and taught to massage the scar at frequent intervals, to optimize scar appearance. However, despite his compliance being suboptimal, his skin-grafted areas and axillary flap settled down well, and he is doing well on long-term follow-up of 2 years [Figures 8, 9 and 10].

- Axillary defect was resurfaced with a transposition flap from left parascapular region and the donor site skin grafted

- Anterior chest wall region was closed primarily and healed well

- Posterior chest wall region covered with a split-thickness skin graft, which has healed well
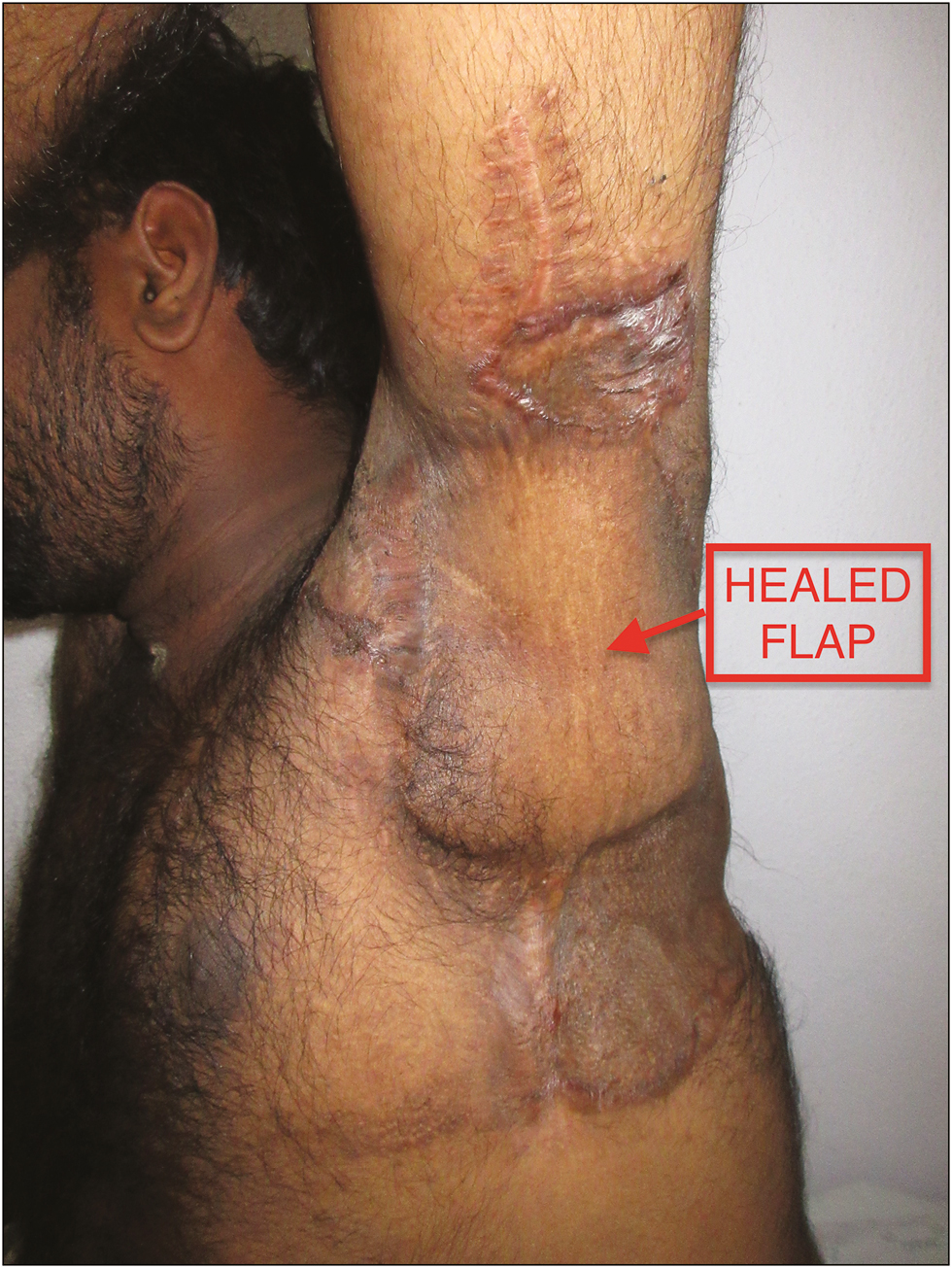
- Axillary flap settled well on long-term follow-up
DISCUSSION
In 1895, Kofmann et al.[2] described the first case of NC and it was initially named “comedo nevus.” NC is due to a pathology in the pilosebaceous apparatus, clinically characterized by papules with central follicular ostia, filled with pigmented keratotic pads resembling comedones, with the neck and face being most commonly involved regions.[3] The lesions, which are present at birth, tend to follow Blaschko lines or Voigt’s lines. Other patterns such as segmental, unilateral, bilateral, or an extensive involvement may also be seen.[45]
NC usually remains asymptomatic and can increase in the size or distribution during puberty under the influence of hormones.[6] Two forms of NC have been described, of which the most commonly encountered is the noninflammatory type that resembles acne-like comedonal eruptions. The inflammatory type, which is not as common, presents with cysts, pustules, fistulae, and abscesses.[78] In our case, the lesions were of the latter type with recurrent abscesses leading to hidradenitis suppurativa, causing pain and discomfort, which prompted the patient to opt for surgery after multiple attempts with topical medications and lasers failed.
Extensive NC can be an associated cutaneous feature of the NC syndrome, which involves neurological, skeletal, and ophthalmological defects. The common symptoms include seizures, paresis, EEG abnormalities, polydactyly, limb defects, and cataracts.[9] Hence, all patients presenting with extensive distribution of NC should undergo thorough systemic examination and necessary investigations to rule out the syndrome, minimizing significant morbidity.
In most cases, NC remains asymptomatic, and hence treatment is not warranted, unless complicated with secondary infections, pustules, abscesses, fistulae, or is cosmetically disfiguring. Treatment can be divided into conservative medical and surgical management. Localized uncomplicated NC can be treated with comedo extraction, dermabrasion, superficial shaving, and topical keratolytics such as urea, tazarotene, retinoids, calcipotriene, and ammonium lactate[10] with varying degrees of improvement, but the high recurrence rate has made topical management unpopular.
Diode laser and ablative lasers such as erbium, neodymium-doped yttrium aluminum garnet, and ultrapulse CO2 lasers have been successfully used in a few NC cases and ultrapulse CO2 laser has been found to be more effective than other lasers, owing to its deeper penetration.[311]
Surgical excision with primary closure and reconstruction with tissue expander have been tried for treatment of NC lesions with good, aesthetic results.[12] Extensive lesions with secondary complications, as in our case, require staged surgical excision and resurfacing, and tissue defects can be effectively reconstructed with flaps and skin grafting. The local flap in the axilla provided good soft-tissue padding, enabling unrestricted arm movements.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Successful treatment of nevus comedonicus with ultrapulse CO2 laser. Indian J Dermatol Venereol Leprol. 2009;75:534-5.
- [Google Scholar]
- Nevus comedonicus: Case report and brief review of the literature. Pediatr Dermatol. 1991;8:300-5.
- [Google Scholar]
- Nevus comedonicus with multiple cysts. J Korean Cleft Palate Craniofac Assoc. 2009;10:135-7.
- [Google Scholar]
- Nevus comedonicus associated with epidermoid cyst. Indian J Paediatr Dermatol. 2016;17:277-9.
- [Google Scholar]






