Translate this page into:
Beware What You Inject: Complications of Injectables—Dermal Fillers
Address for correspondence: Dr. Maya Vedamurthy, Medical Director and Consultant Dermatologist, RSV Skin and Research Centre, Senior Consultant Dermatologist Apollo Hosptials, AB-76, 1st street, Annanagar, Chennai-600040, Tamil Nadu, India. E-mail: Mayavedamurthy@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cosmetic filler injections are most popular among the antiaging procedures. As in any other cosmetic injectable procedures, complications are likely to occur even under experienced hands. However, it is the duty of the aesthetic physician to identify and manage these potential complications. The objective of this symposia is to help the aesthetic physician to identify these complications early and manage them appropriately to improve outcomes.
Keywords
Fillers
hyaluronic acid fillers
complications
adverse effects
INTRODUCTION
Soft tissue augmentation is steadily increasing with the aging of baby boomers in the population, mainly because it is of low cost, has instant results, and is relatively safe. Dermal fillers rank second among the top five nonsurgical cosmetic procedures, behind botulinum toxin injections.[1] According to American Society for Dermatologic Surgery survey, interest in cosmetic procedures continues to rise and these procedures continue to grow with demand, and that there has been a significant (16%) increase in the hyaluronic acid (HA) filler in 2016. As a result, there is a surge in the popularity of dermal fillers to address the signs of aging. The market is flooded with more than 100 products, and dermal fillers are currently being used by several practitioners other than dermatologists and plastic surgeons. With an increase of soft tissue augmentation procedures in the current scenario, the number of complications is also likely to increase. A thorough knowledge of anatomy, the different properties of the available filler substances, and injection techniques are essential to prevent complications of the filler. It is also necessary to detect complications early and manage them effectively to minimize adverse effects and improve patient outcomes.
There is an increase in soft tissue augmentation simply because of increased public awareness, simplicity of the procedure, and high patient satisfaction rates. This has led to a proportional increase in the number of complications.
All dermal fillers and filler procedures can lead to complications, which may be related to one of the following.
-
Product-related: Permanent non-resorbable products, antigenic nature of the material
-
Physician-related: Lack of knowledge, insufficient experience
-
Host-related: Altered host defense mechanism
Hence, it is important to be aware of all the above considerations to avoid or minimize complications.
BEWARE OF PRODUCT
A simple working classification of a product in view of complications would be as follows:
-
Nonpermanent and biodegradable
-
Semipermanent and biodegradable
-
Permanent and reversible
-
Permanent and nonreversible
Fillers are classified into three major classes based on their longevity in the tissues, which in turn depends on its structure and composition.
-
Temporary lasts less than 18 months
-
Semipermanent lasts greater than 18 months
-
Permanent lasts longer than 24 months
It is generally believed that permanent fillers are nonbiodegradable and nonreversible, and therefore complications with the inflammatory process are more likely to occur with permanent fillers.[2]
Fillers are classified based on the histologic reaction as “volumateurs” with little cellular response and “stimulateurs” with strong cellular reaction.[3] A knowledge of this property of the filler substance may serve as a guide in predicting later inflammation or granuloma formation.
Understanding the biology of the fillers will help to avoid filler complications [Figure 1]. The HAs properties vary in terms of cross-linking, gel particle size, and their concentration. Extensive cross-linking is thought to increase longevity as they are more resistant to degradation by native hyaluronidase. Similarly, large particle size of gel has less total area that is subject to attack by the body and is more likely to resist degradation by hyaluronidase. But large particle size and increased concentration increase the hydrophilic nature of the product, leading to more tissue swelling after the procedure. Increased concentration, large particle size, and greater cross-linking increase the longevity of the product and theoretically increase the possibility of adverse reactions.
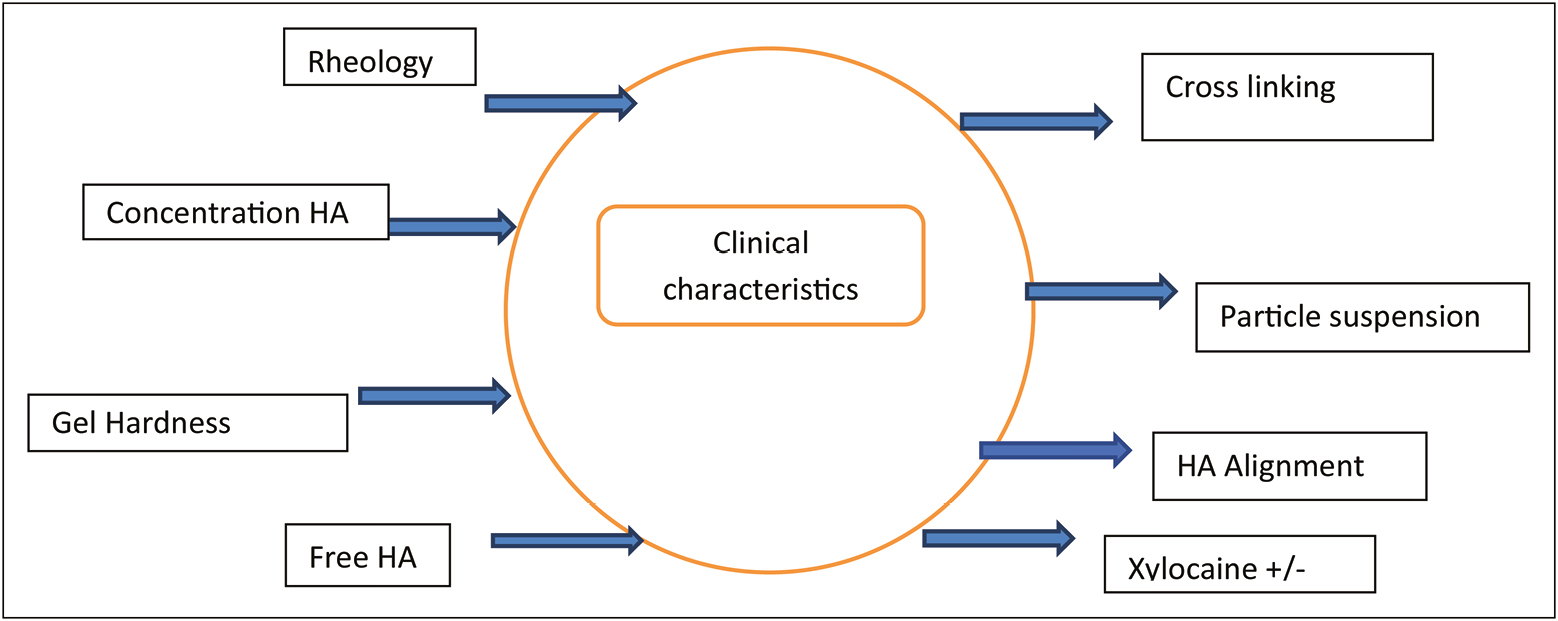
- Characteristics of dermal filler. HA: hyaluronic acid
HISTORY AND PHYSICAL EXAMINATION
A history to assess physical and mental health, drug intake, and history of surgery or previous fillers in the area to be treated is important to avoid complications.
KNOW THE ANATOMY
A thorough knowledge of the anatomy of the skin and vasculature in the treatment area is necessary for the following [Figure 2]:
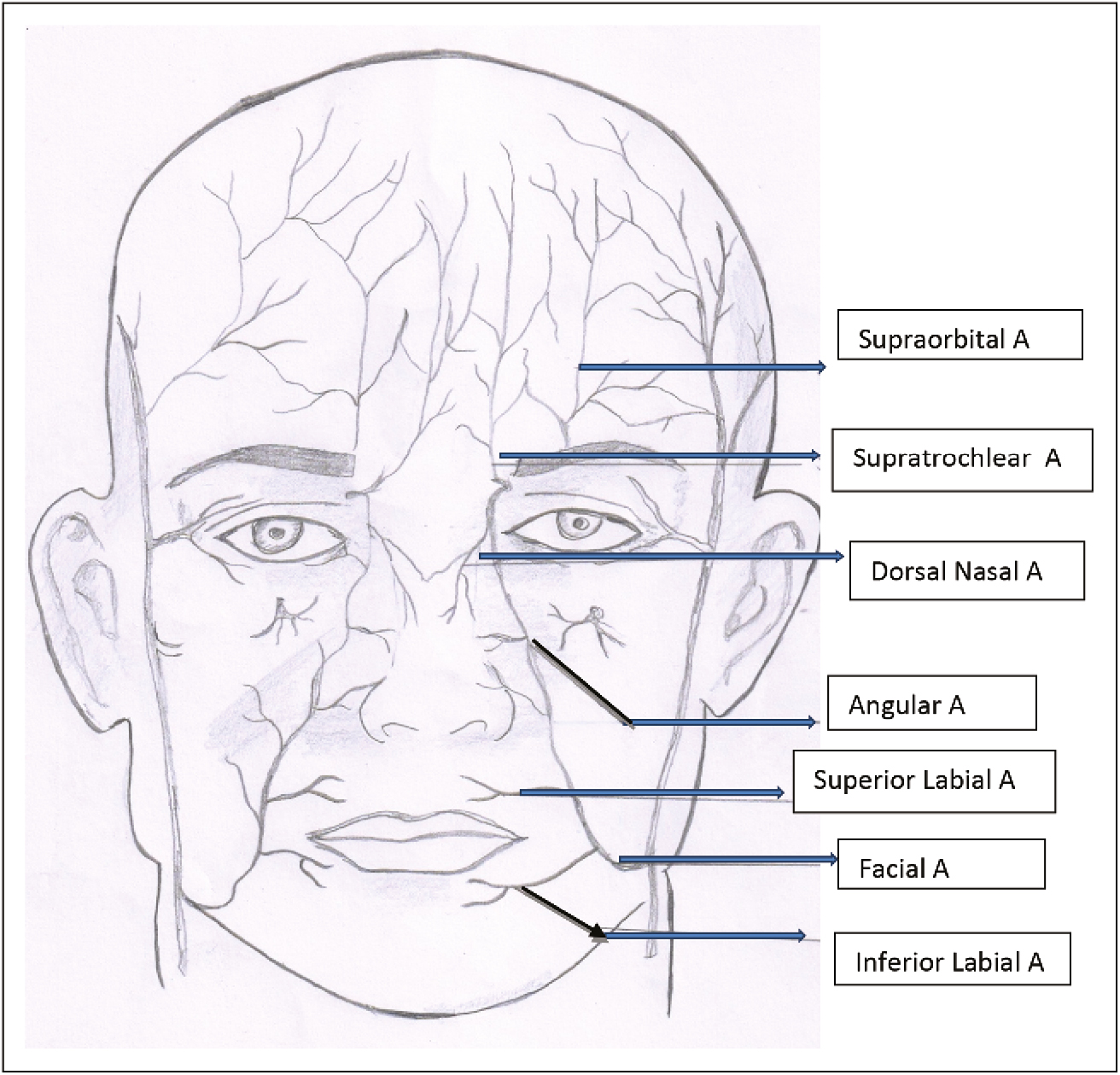
- Arteries of the face
-
For proper placement of filler material to avoid lumps, bumps, or Tyndall effect
-
To avoid inadvertent placement into vessels, which could lead to necrosis, blindness, and other similar vascular accidents
-
To increase longevity of the product as they stay longer when injected in the recommended depth
SKIN THICKNESS
Injecting in the correct plane is important for best results. It is important to know the differences in skin thickness in different parts of the face [Figure 3]. The thickness of the facial dermis varies between 0.4mm in lids and 1.2mm in forehead and cheeks. The outer diameter of 26-G needle can be used as a rough gauge to guide the depth of injection as it measures 0.45mm, which is half the thickness of the dermis, or conversely the facial dermis is only about twice as thick as 26-G needle. So for a proper intradermal injection, the needle should be inserted at approximately 10° angle and one-needle diameter deeper. For injection into mid-dermis to treat moderate-to-deep folds, the needle should be inserted at an angle of 30°–40°, and for injection into deep dermis or supraperiosteal region to treat deeper folds, the needle should be directed at an angle of 45°–90°.
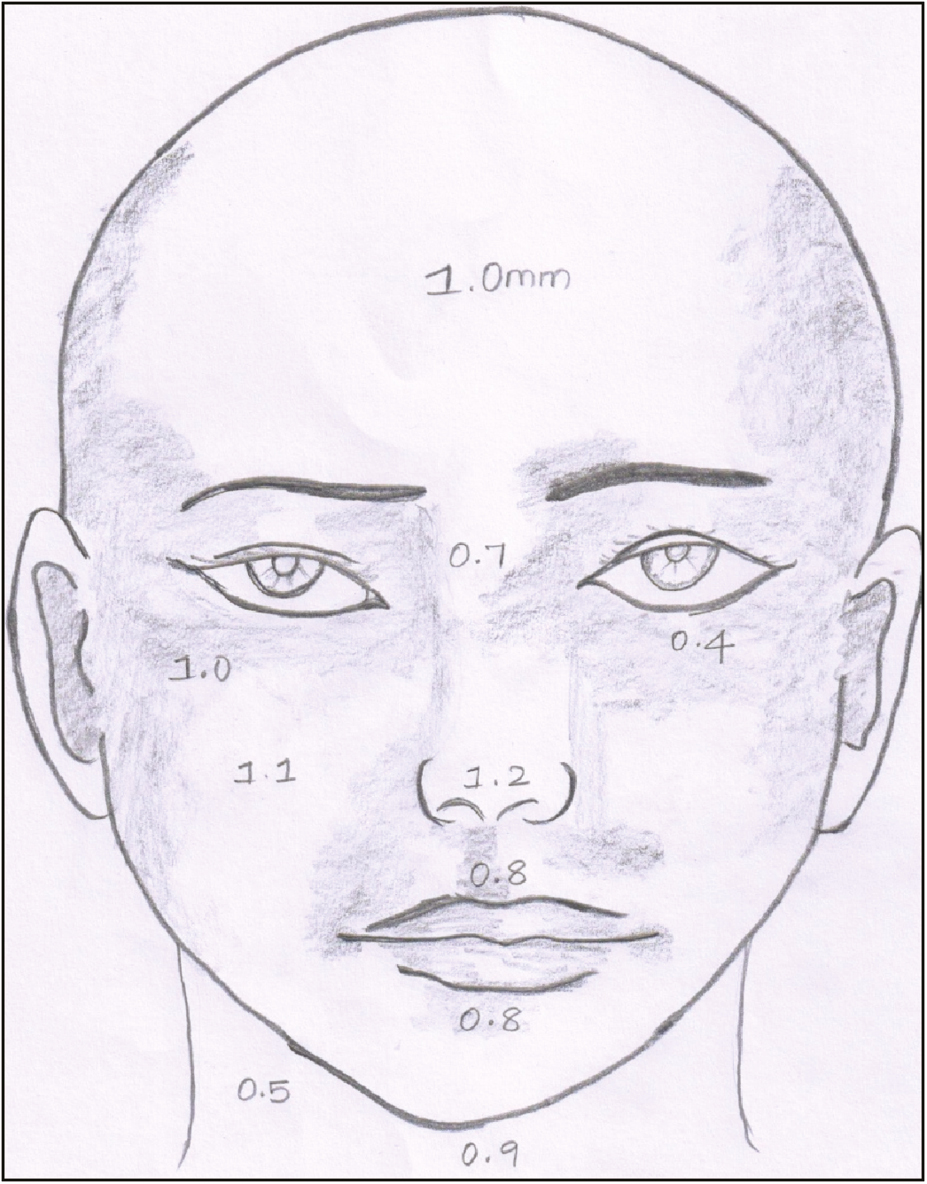
- Thickness of dermis in different areas of the face
BEWARE OF VASCULATURE
Vascular compromise can occur because of inadvertent injections into certain vessels or as a result of external compression due to pressure from the injected material.
The areas prone for embolization leading to blindness are the nose, nasolabial fold (NLF), forehead, and glabella, whereas the areas prone for necrosis are glabella, tip of nose, and lips.
BEWARE OF TECHNIQUE
Dermal fillers may be injected using a needle or cannula based on the experience and comfort of the injector as both have their own advantages and disadvantages. In general, fillers should be injected slowly after aspiration, and the delivery of material should be in small volumes per pass and with least amount of pressure.[4] The use of small-caliber needles slows the speed of injection, and the use of blunt cannulas in high-risk regions, such as glabella, nose, and NLF, reduces the risk of injury to vessels.[5]
Most important for a safe practice is a sterile workplace and strict asepsis during the technique to avoid infections.
RECOGNIZING, MANAGING, AND AVOIDING DERMAL FILLER COMPLICATIONS
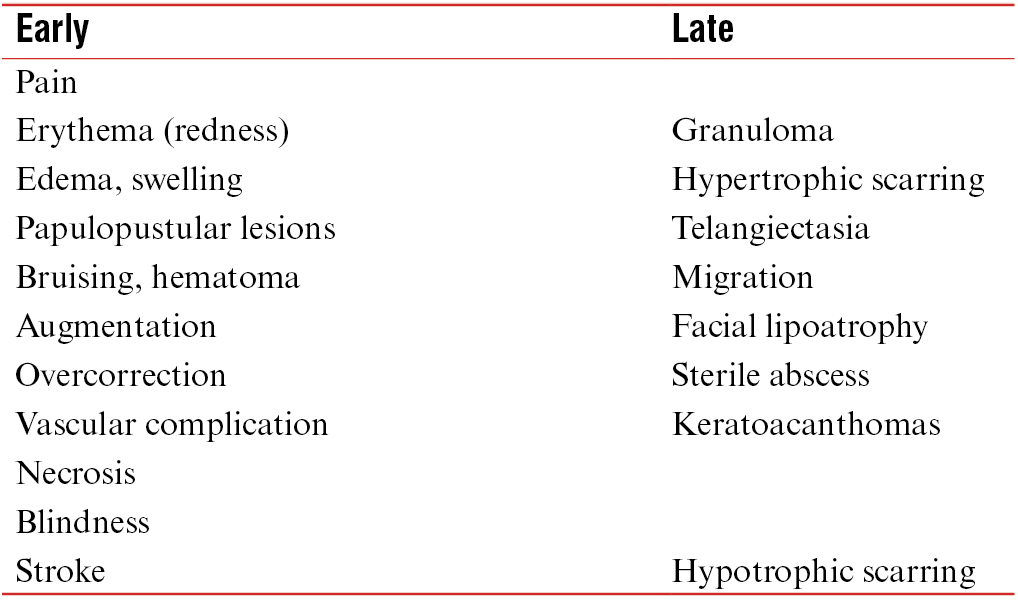
Despite safety measures and safety profiles of the products, adverse events do occur. The complications may be classified based on the timing of occurrence [Table 1] and may be patient related, technique related, or injection substance related.
EARLY COMPLICATIONS
Pain
Pain can occur as a sequelae of multiple needle punctures. If there is a striking radiation pain occurring along the vascular course, during the filler injections or after few hours of the injection, it denotes a vascular complication and appropriate measures need to be taken. Pain can be minimized by slow introduction of a needle with the thinnest gauge possible. Use of long needles to reduce needle pricks, ice anesthesia, and warming up the filler to body temperature can minimize pain.
Erythema (redness)
Transient erythema is common after procedure and usually disappears without any treatment. Longer lasting erythema or persistent erythema is more common as a result of a hypersensitive reaction to different compounds or as a result of infection. So a careful evaluation and appropriate treatment are necessary.
Management includes avoiding erythema-inducing agents such as alcohol, exercise, and sun exposure. Topical steroids can be used for short periods to reduce the erythema. Topical tacrolimus can be used as an anti-inflammatory agent to reduce persistent erythema. Appropriate makeup may be advised to cover the erythema. In severe cases, oral propranolol (20mg) may make the erythema less evident.[6]
Edema (swelling)
Non-hypersensitivity-related swelling
Edema may occur immediately after the injection because of manipulation and rarely persists for more than a couple of days. This can be effectively managed by gentle pressure and ice packs.
Episodic swelling and edema can occur after exposure to vasodilating stimuli such as sun exposure, exercise, or sauna bath following HA injectables.[7] As this may occur without any other sign of allergic reaction, the treatment can be in the form of ice packs and topical steroids along with the avoidance of vasodilating situations. For severe cases, systemic steroids can be given.
True hypersensitive-related swelling
Edema can also occur following true hypersensitivity reactions to injected products. This may occur as an angioedema at the site of injection or at distant sites with or without urticarial reaction over the body. This is treated with antihistamines and systemic steroids over a period of several weeks.
Delayed hypersensitivity-related swelling
Delayed hypersensitivity-related facial edema is usually non-antibody-mediated type IV reaction, which occurs days to months after the injection.
This is T lymphocyte mediated rather than antibody mediated and presents with induration, edema, and erythema.[8] It usually responds to oral steroids rather than antihistamines. The last and the best option is to remove the causative filler material.
Papulopustular lesions
Sterile folliculitis lesions occur because of occlusion of sebaceous or sweat gland openings and mimic bacterial infections or acneiform eruptions. If the filler is injected too superficially into the papillary dermis, it can be extruded through the sebaceous glands and appear like acne. Firm massaging soon after the injection may prevent the occurrence of these lesions. Topical treatment with astringents will help in cleaning these papulopustular lesions.
Bruising, hematoma, ecchymosis
Bruising, hematomas, and ecchymoses may occur because of needle pricks and bleed from these points. It is more commonly seen in patients on anticoagulants or alcohol intake. This can be minimized by firm pressure at the site of needle insertion or by stopping the intake of anticoagulants; supplements including ginkgo biloba, vitamin E, omega-3 fatty acids, and St. John’s wort; alcohol; and mushroom 1 week before the procedure. Use of arnica, topical vitamin K, or bromelain has also been helpful to decrease the incidence of ecchymosis. In some situations, intense pulsed light and vascular lasers have been used to treat postinjection bruises.
Overcorrection
Overcorrection may appear as bumps, nodules, or irregularities, especially when too much of the material is injected. Hyaluronic acid products may be easily resolved using hyaluronidase. In case of non-hyaluronic acid, a simple puncture with a wide bore needle and drainage of the excess product may suffice.
A bluish discoloration also known as the Tyndall effect may occur if an excessive amount of HA is placed superficially under the skin, and this can be decreased by injecting hyaluronidase.
Recommendations for hyaluronidase:
<2.5mm area: 10–20 U single injection
2.5 mm–1 cm: 2–4 injection points with 10–20 U per injection point
Injections may be repeated if required[9]
Old protocol: Repeated daily and continued for at least 4 days
New protocol: Repeated hourly till resolution of the symptoms
VASCULAR COMPLICATIONS
Vascular complications occur as result of inadvertent arterial injection of filler material and could result in serious injury in the form of cutaneous necrosis, blindness, or stroke.
Tissue necrosis
Cutaneous necrosis can also occur as a result of excess material causing external vascular compression, and thereby reduced perfusion leading to scar formation.[10] An intra-arterial injection can cause mechanical obstruction and damage of endothelial cells leading to ischemic changes in the skin. The common sites of necrosis reported after filler injections are the glabella, nasal ala, and NLF area [Figure 4].
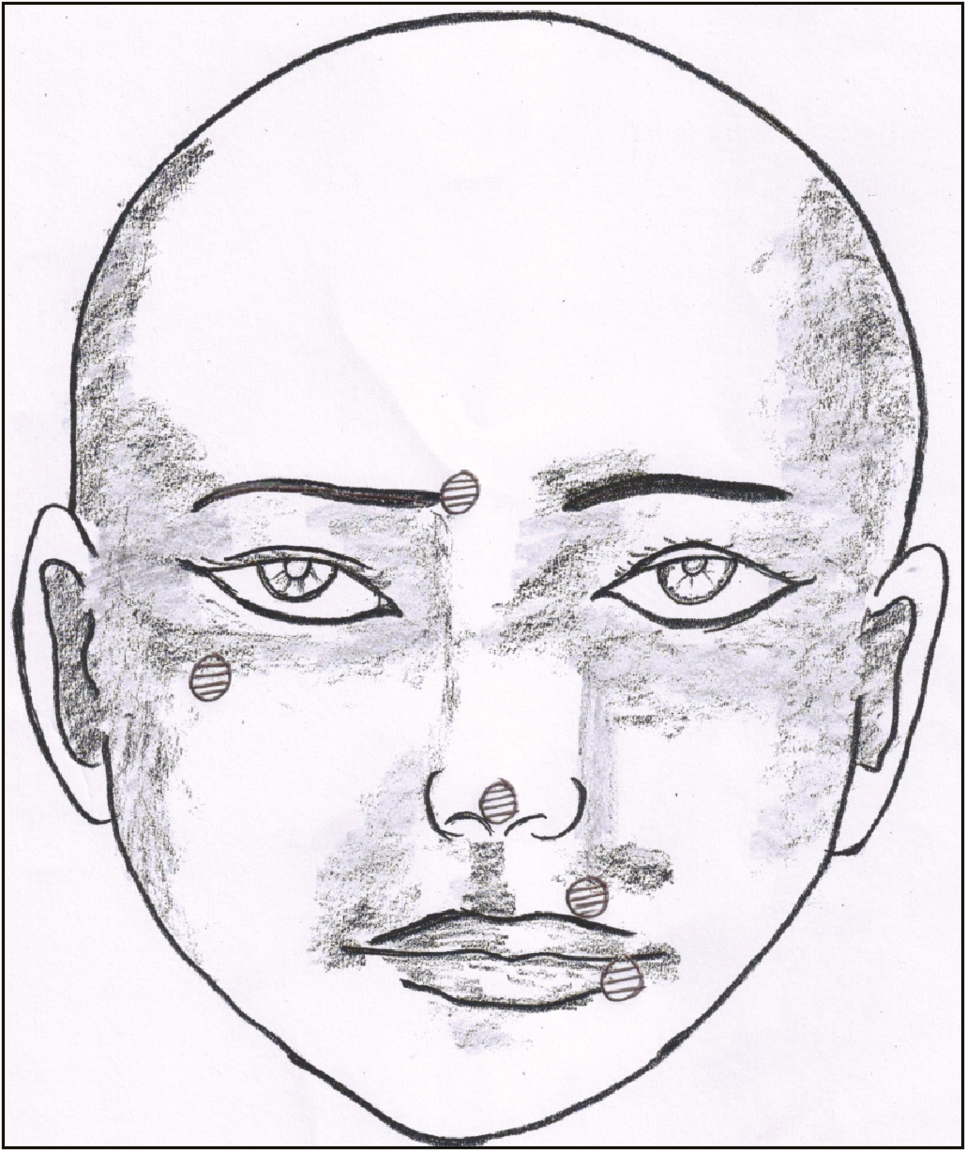
- Sites of injection leading to necrosis -shaded area
Early recognition and prompt action are mandatory. Painless blanching during the procedure followed by severe pain is the first sign of injection necrosis. One should stop injecting immediately and gently massage the treated area. The ischemia is usually followed by a dusky discoloration and then a necrotic skin.
Visual impairment
Blindness occurs from filler embolism to the ophthalmic vasculature. Visual loss usually occurs immediately and is accompanied by pain in the affected eye.[11] Visual complications usually occur following injections in the glabella, nose, forehead, and periocular regions [Figure 5].
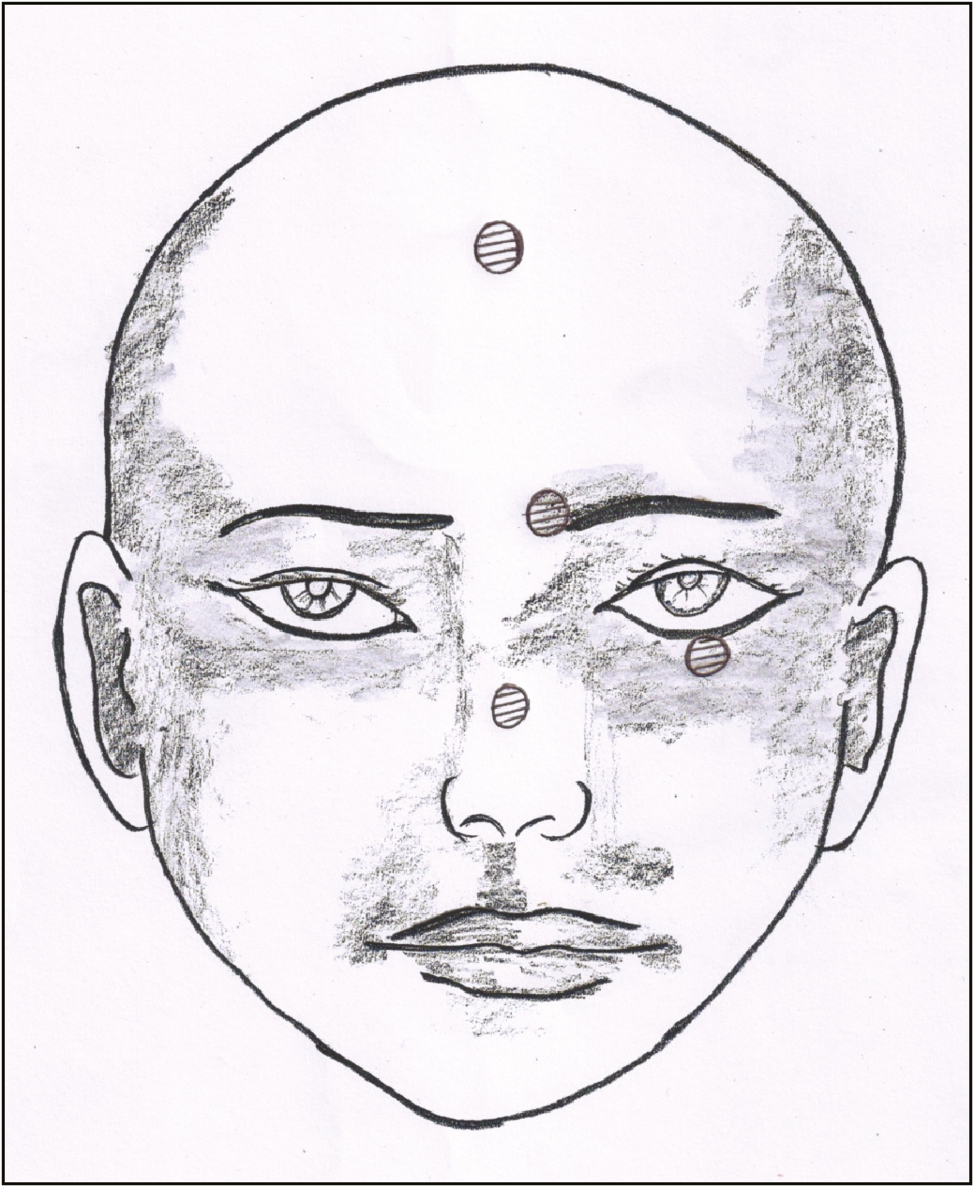
- Sites of injection leading to blindness
The underlying mechanism of retinal artery occlusion is secondary to retrograde embolization from peripheral vessels into the ophthalmic artery system.
Stroke
Rarely when greater force is applied during injection, the filler emboli can enter the internal carotid artery and then be pushed into the intracranial circulation leading to cerebral ischemic events.
Unilateral blindness and left-sided hemiplegia because of retrograde flow of autologous fat following fat injections in the glabellar region have been reported.[12]
Vascular complications are best avoided by a proper understanding of the anatomy and proper injection technique. Aspiration must be performed before each injection and the filler should be injected slowly and injection of small volumes per pass in two or more treatment sessions.
Management
In cases of suspected intravascular injection, one should immediately stop the procedure, massage the area gently, and apply warm compresses. Topical nitroglycerin paste can be used for vasodilation. Aspirin, low-molecular-weight heparin, and intravenous prostaglandins have all been advocated. New high dose pulsed hyaluronidase protocol appears to be a simple, safe and successful way to manage adverse vascular events of HA fillers.[13] Here, the dosing depends on the amount of tissues adversely affected. In case of blindness, immediate ophthalmologic consultation, ocular massage, and retrobulbar injections of hyaluronidase should be given. Unfortunately, the prognosis in such cases is grave regardless of the treatment given. In cases of cutaneous necrosis, proper wound care and antibiotics to minimize scarring is recommended. If scarring occurs, it may be treated with light dermabrasion, scar revision surgery, or dermal filler.[14]
INFECTION AND BIOFILMS
Infections clinically present as warm, tender erythematous fluctuant nodule with or without systemic signs such as fever and malaise. Usually, early low-grade infections are due to Staphylococcus aureus and occur as a result of contaminated filler depots and organize into biofilms, whereas late presentation raises suspicion of atypical mycobacterial infections. Bacteria present in biofilms remain dormant for a long time and emerge from their biofilm following activation by an external triggering factor such as a minor injury or manipulation, leading to low-grade infections, granulomas, or abscesses. Risk of infection is found to be higher in human immunodeficiency virus (HIV)-positive patients.
Management
Management of infection depends on the severity of the condition [Table 2]. Clinical judgment should decide the course of action with regard to choice of antibiotic, use of hyaluronidase, and surgical intervention. For mild cases, empirical therapy with antibiotics such as ciprofloxacin, clarithromycin, and amoxicillin + clavulanic acid for 2–4 weeks is suggested.
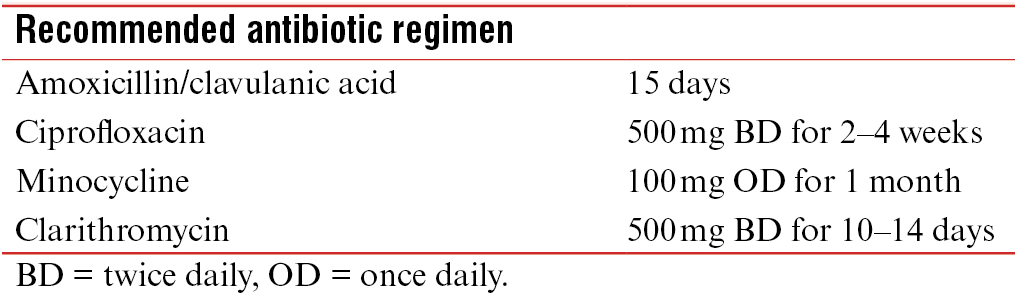
For abscess, incision and drainage or aspiration may help in faster resolution. If empirical antibiotic therapy fails, culture-directed therapy can be useful. Hyaluronidase may be injected to avoid further spread of infection.[9] Intralesional steroids may be injected into inflammatory nodules under antibiotic cover.
INTRACRANIAL PENETRATION
There is a potential risk of accidental intracranial penetration while performing the deep temple injection technique with direct pressure on the bone as the thickness of the bone is variable at the pterion.[16] Therefore, a good knowledge of the anatomy combined with gentle injection technique is mandatory while injecting fillers into the deep temporal fossa.
LATE COMPLICATIONS
Granulomas
Granulomas are rare and occur as a result of type IV hypersensitivity reaction to a foreign body. Usually they occur after a latent period of months to years after injection.
A proper medical and cosmetic treatment history is essential to make a correct diagnosis. The inflammatory reaction may be triggered by systemic infection, excessive sun exposure, impurity of dermal fillers, or consecutive injections of different fillers in the same facial region. A tissue diagnosis fulfilling the pathologic criteria of granuloma consisting of epithelioid cells and multinucleated cells is necessary to distinguish it from an inflammatory nodule.
Hypertrophic scarring
Hypertrophic scarring can occur with superficial placement of fillers. This rarely leads to permanent scar consisting of extracellular matrix components such as collagen, fibroblast, and small vessels.
Management of hypertrophic scarring is softening the tissue with pulsed dye laser or intralesional steroids. In extreme cases, scar revision surgery may be needed.
Telangiectasia
There can be de novo appearance of telangiectasia or worsening of preexisting telangiectasia at the injection site. In addition, treatment of erythema with prolonged topical steroid therapy can also induce telangiectasia.
Management of telangiectasia is by decreasing the volume of filler to minimize the pressure effect on vessels, and in addition, treatment with intense pulsed light therapy and pulsed dye laser can also be effective.
Migration
Fillers composed of suspensions of particles such as HA as microspheres like poly-l-lactic acid are capable of migration. It usually occurs when these fillers are placed in highly mobile areas where they get pushed by the activity of the muscle or because of gravitational forces. Migration to distant sites has also been described. It is influenced by gravity and occurs in patients with lax skin and subcutaneous tissue.
Management is to advise patients to limit all facial expressions for approximately 3 days after injection. In undesirable situations, the filler may be dissolved with hyaluronidase or removed completely.
Sterile abscess
Low-grade inflammation with negative bacterial culture may present as sterile abscess. In such cases, incision and drainage of the abscess and a course of tetracycline have been found to be effective.[17]
CONCLUSION
Use of dermal fillers continues to rise in popularity, and as the use of dermal fillers increases, the adverse events are also likely to increase, and it is important to be aware of all potential complications and be prepared to treat them effectively. Familiarity with prevention, recognition, and early and effective management of complications is the key to a successful and safe filler practice.
Practical tips:
-
Choose the right patient
-
Know your product specifics well
-
Master safe injection techniques
-
Recognize early signs of complications
-
Engage in proactive management to minimize their impact
-
Appropriate timing of other cosmetic procedures to be planned and executed well
In general, most complications are avoidable if injections are administered under aseptic precautions with sound knowledge of facial anatomy and technique. Dermal fillers have a great demand for the future as more and more patients opt for nonsurgical procedures with minimal downtime and risk.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- American Society for Aesthetic Plastic Surgery. ASAPS. 2016. Cosmetic surgery national databank statistics. Available from: http://www.surgery.org/sites/default/files/ASAPS-2016-Stats.pdf
- [Google Scholar]
- Liquid silicone for soft tissue augmentation: histological, clinical and molecular perspectives. In: Klein AW, ed. Tissue augmentation in clinical practice (2nd ed). New York: Taylor & Francis; 2006. p. :141-238.
- [Google Scholar]
- Long-lasting and permanent fillers: biomaterial influence over host tissue response. Plast Reconstr Surg. 2007;13:2271-86.
- [Google Scholar]
- Blindness following cosmetic injections of the face. Plast Reconstr Surg. 2012;13:995-1012.
- [Google Scholar]
- Utilizing blunt-tipped cannulas in specific regions for soft-tissue augmentation. J Drugs Dermatol. 2012;13:s40-1.
- [Google Scholar]
- Injectable hyaluronic acid gel for soft tissue augmentation. A clinical and histological study. Dermatol Surg. 1998;13:1317-25.
- [Google Scholar]
- Global Aesthetics Consensus Group. Global aesthetics consensus: avoidance and management of complications from hyaluronic acid fillers-evidence- and opinion-based review and consensus recommendations. Plast Reconstr Surg. 2016;13:961e-71e.
- [Google Scholar]
- Understanding, avoiding, and managing dermal filler complications. Dermatol Surg. 2008;13:S92-9.
- [Google Scholar]
- Ocular ischemia with hypotony after injection of hyaluronic acid gel. Ophthalmic Plast Reconstr Surg. 2011;13:e152-5.
- [Google Scholar]
- Middle cerebral artery embolism and unilateral visual loss after autologous fat injection into the glabellar area. Stroke. 1993;13:615-6.
- [Google Scholar]
- New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;13:814-25.
- [Google Scholar]
- Abscess formation and local necrosis after treatment with zyderm or zyplast collagen implant. J Am Acad Dermatol. 1991;13:319-26.
- [Google Scholar]
- Treatment of soft tissue filler complication: expert consensus recommendations. Aesth Plast Surg. 2018;13:498-510.
- [Google Scholar]
- Intracranial Penetration During Temporal Soft Tissue Filler Injection—Is It Possible? Dermatologic Surgery. 2018;13:84-91.
- [Google Scholar]
- Delayed-onset complications of facial soft tissue augmentation with permanent fillers in 85 patients. Dermatol Surg. 2013;13:1474-85.
- [Google Scholar]






