Translate this page into:
Fourth Dimension in Reconstruction of Defects Following Excision of Basal Cell Carcinoma of Head and Neck!
Address for correspondence: Dr. Sridhar Sruthi, A 2, Srinivasa Apartments, 27, Srinivasa Avenue Road, R. A. Puram, Chennai 600028, Tamil Nadu, India. E-mail: sruthi195@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Basal cell carcinomas (BCCs) are the most common skin tumors of the face. Excision results in soft tissue defects that require reconstruction with the focus on form, function, and patient satisfaction.
Aim:
To analyze the reconstruction of BCC excision defects of the head and neck region using local flaps and skin grafts with respect to the four dimensions of oncological reconstruction: clearance, form, function, and patient satisfaction.
Materials and Methods:
This is a prospective study conducted on 88 patients who presented with BCC of the head and neck region and who were operated in our hospital from January 2015 to December 2016 with a minimum follow-up period of 6 months up to June 2017. All patients underwent wide local excision and reconstruction using appropriate local flaps or split-thickness skin graft (SSG). Patients were analyzed with respect to age, sex, site, size, reconstruction method, complications, and patient satisfaction using the customized Patient Satisfaction Questionnaire (PSQ), derived from PSQ III.
Results:
A total of 77.3% defects were immediately reconstructed using local flaps and 18.2% underwent SSG. All flaps and grafts survived well with a complication rate of 6.8%. Approximately 72.7% of patients had good satisfaction with the medical care and reconstruction.
Conclusion:
Post-excisional defects of BCC in the head and neck region have to be reconstructed with equal weightage to the four pillars of oncological reconstruction: clearance, form, function, and patient satisfaction. Flap reconstruction is ideal as it brings about reconstruction with patient satisfaction, which is indeed the fourth dimension in any reconstructive surgery.
Keywords
Basal cell carcinoma
local flaps
patient satisfaction
reconstruction
INTRODUCTION
Basal cell carcinomas (BCCs) are the most common cutaneous tumors accounting for 70% of skin malignancies.[1] Approximately 80% of BCCs occur on the face.[2] Wide local excision is the standard management, followed by reconstruction with flap or split-thickness skin graft (SSG).
Oncological surgery focuses on clearance, whereas reconstruction has to focus on form, function, and patient satisfaction, which is valued less and has a negative impact on the patients’ daily life.
We analyzed BCC defects of the head and neck region, reconstructed using local flaps and SSG, with respect to clearance, form, function, and the fourth dimension patient satisfaction by using a customized Patient Satisfaction Questionnaire (PSQ), derived from PSQ III.
MATERIALS AND METHODS
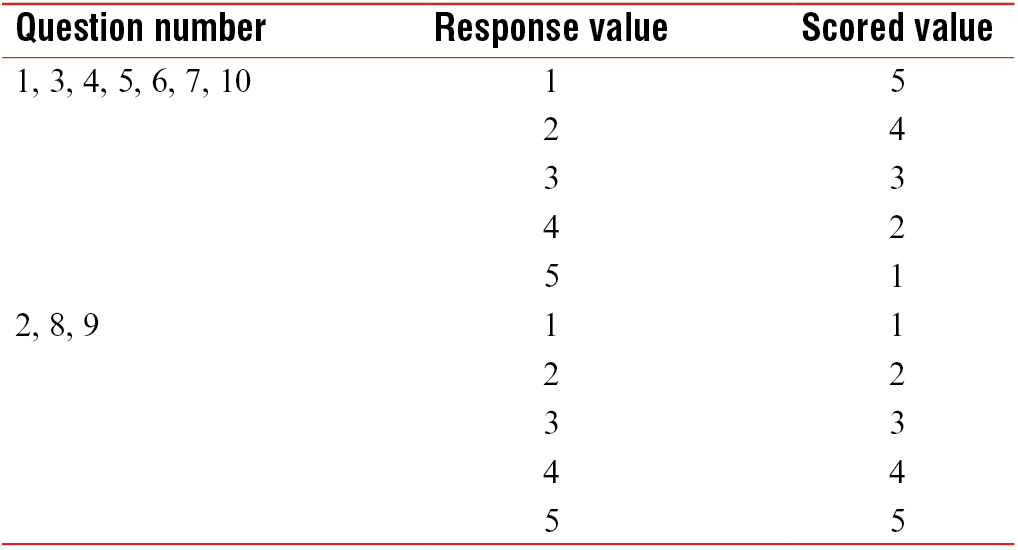
This is a prospective study conducted on 88 patients who presented with BCC of the head and neck region in our hospital from January 2015 to December 2016 with a minimum follow-up of 6 months and a maximum of 2.5 years up to June 2017. All patients underwent routine workup. Lesions less than or equal to 2cm were subjected to excision biopsy with a 5-mm margin clearance. Lesions more than 2cm were subjected to wedge biopsy first, and once diagnosis was confirmed, wide local excision was carried out with a 5-mm margin clearance. All cases were operated under general anesthesia. Resultant defects were immediately reconstructed using appropriate local flaps or SSG. Postoperatively, the patients were assessed for any local complications. The patients were followed up for 1–2 years. Patient satisfaction was assessed using the customized PSQ scale. We made a questionnaire, which was derived from PSQ III, representing the six aspects—general satisfaction, technical quality, interpersonal manner, communication, time spent with doctor, accessibility, and convenience—by including 10 questions numbered 1, 2, 3, 6, 11, 17, 31, 41, 49, and 50 from PSQ III [Table 1]. As the study was being conducted in a government hospital where medical care is free, we did not include the financial aspect of patient satisfaction. The patients were explained the questions in their native language. Responses were graded as follows:

-
Strongly agree
-
Agree
-
Uncertain
-
Disagree
-
Strongly disagree
Each question was scored as shown in Table 2 and the scores were added. Total score equal or above 40 was considered good overall satisfaction. Scores were also analyzed with respect to six aspects of patient satisfaction.
Number of patients: 88
Duration of study: 2 years and 6 months
Inclusion criteria:
-
Primary BCC involving the face and neck region—treated by fusiform excision and primary closure, SSG, and local flaps
-
Patients who could be followed up post-op for a minimum of 6 months
Exclusion criteria:
-
Recurrent BCC
-
Primary BCC reconstructed using regional or free flaps
-
Metastatic BCC
-
Other skin malignancies
-
Patients who opted out or lost to follow-up before 6 months
Parameters assessed:
Apart from patient satisfaction, the following parameters were also assessed:
-
Age and sex
-
Site of BCC
-
Size
-
Reconstruction option used
-
Complications and management
-
Donor-site morbidity
RESULTS
All patients recovered well. No systemic complications were observed. None reported any functional deficit. All flaps and grafts survived. All donor wounds healed well without any complications. All margins were free from tumor pathologically in all cases.
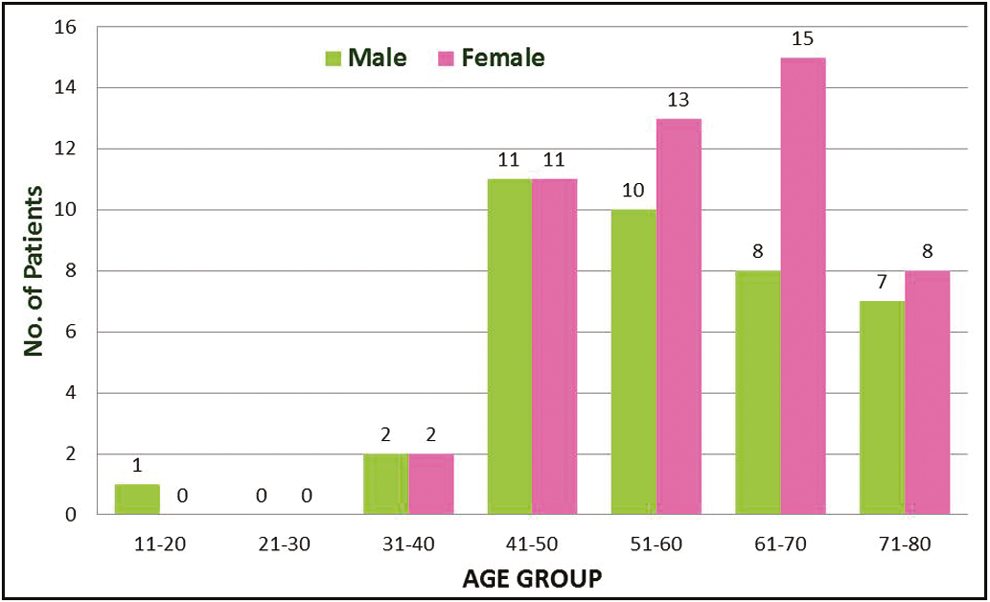
Incidence was more common in female population (55.7%) [Figure 1]. Majority of patients (52.3%) were in their sixth and seventh decades. The youngest in our series was of 15 years and the oldest was of 79 years.
- Number of patients who presented with BCC with respect to age and sex
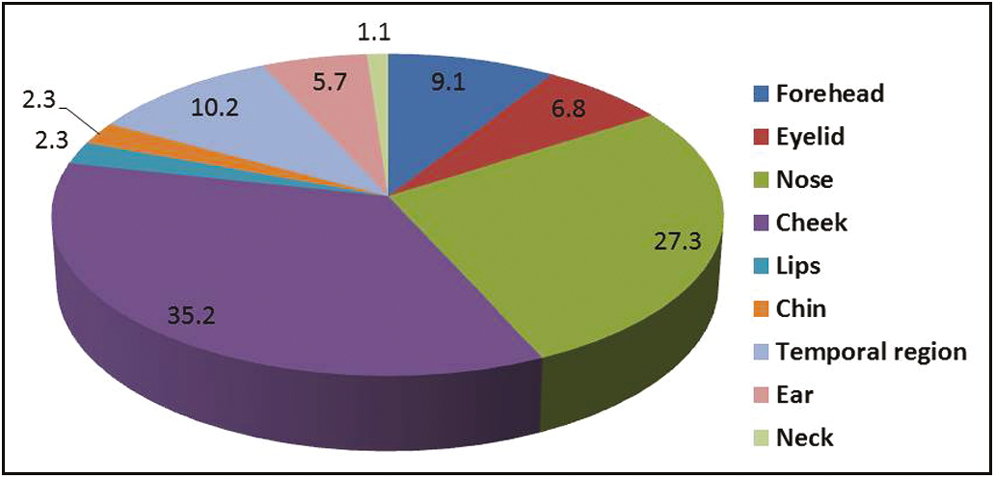
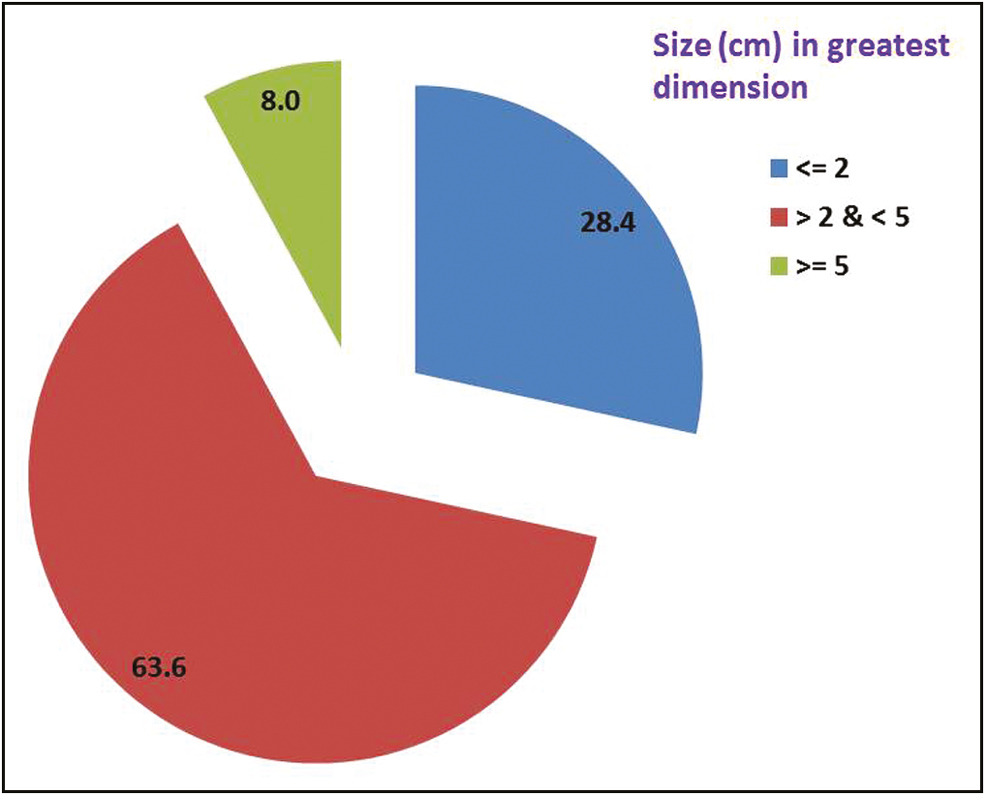
A total of 35.2% cases were present in the cheek and 27.3% in the nose [Figure 2]. Approximately 19.3% of defects involved multiple aesthetic subunits. Clinically, 84% cases were nodular, 10.5% ulcerative, 4.5% superficial spreading, and 1% basosquamous. Approximately 28.4% of patients presented with lesions equal to or less than 2cm in greatest dimension [Figure 3] and underwent excision biopsy based on clinical diagnosis. In 71.6% patients, lesion was more than 2cm and preoperative biopsy was performed to confirm the diagnosis. Eight percent presented with giant BCC.
- Percentage distribution of BCC in different areas of head and neck
- Percentage distribution of lesions based on their maximum dimension
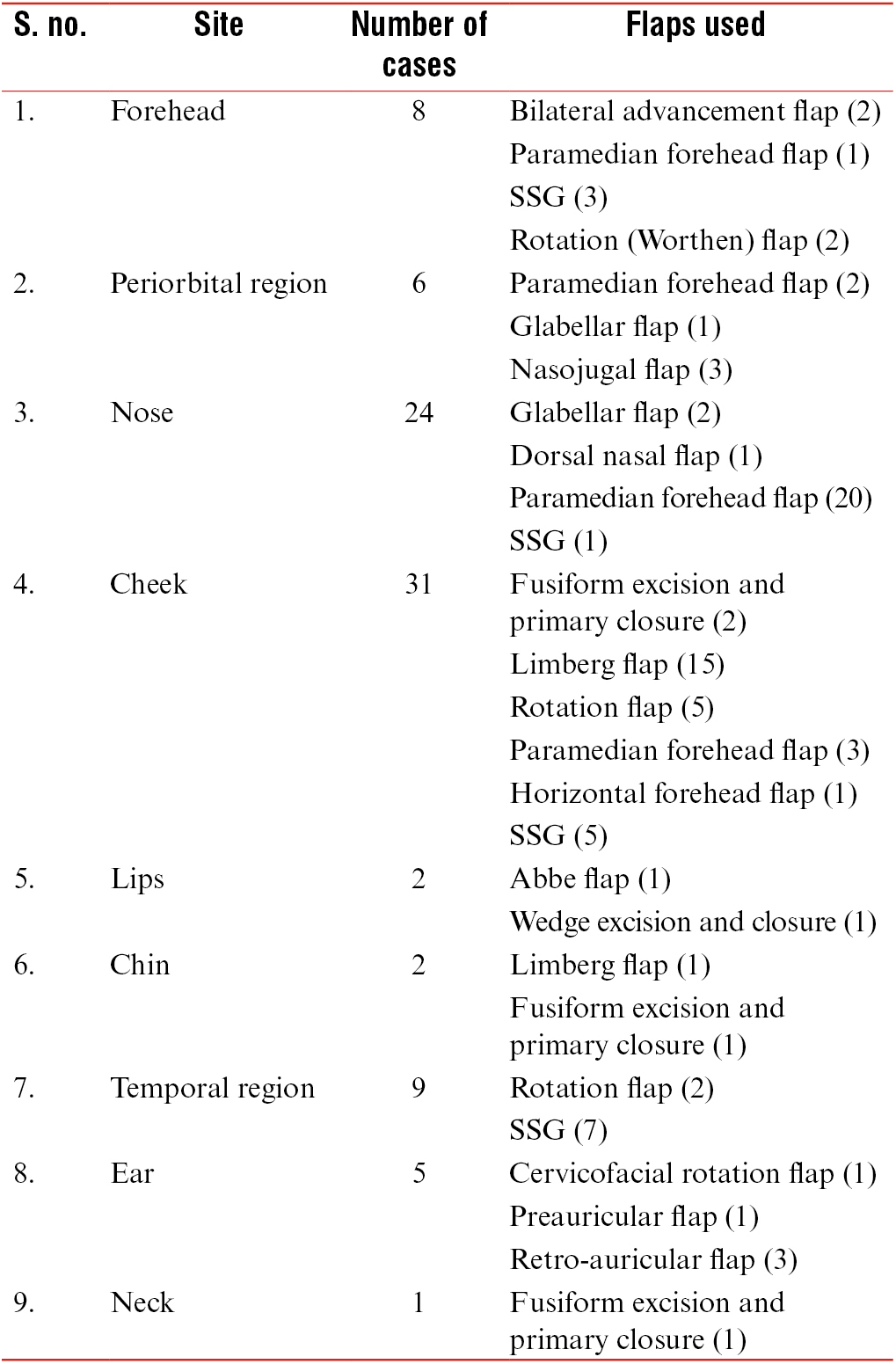
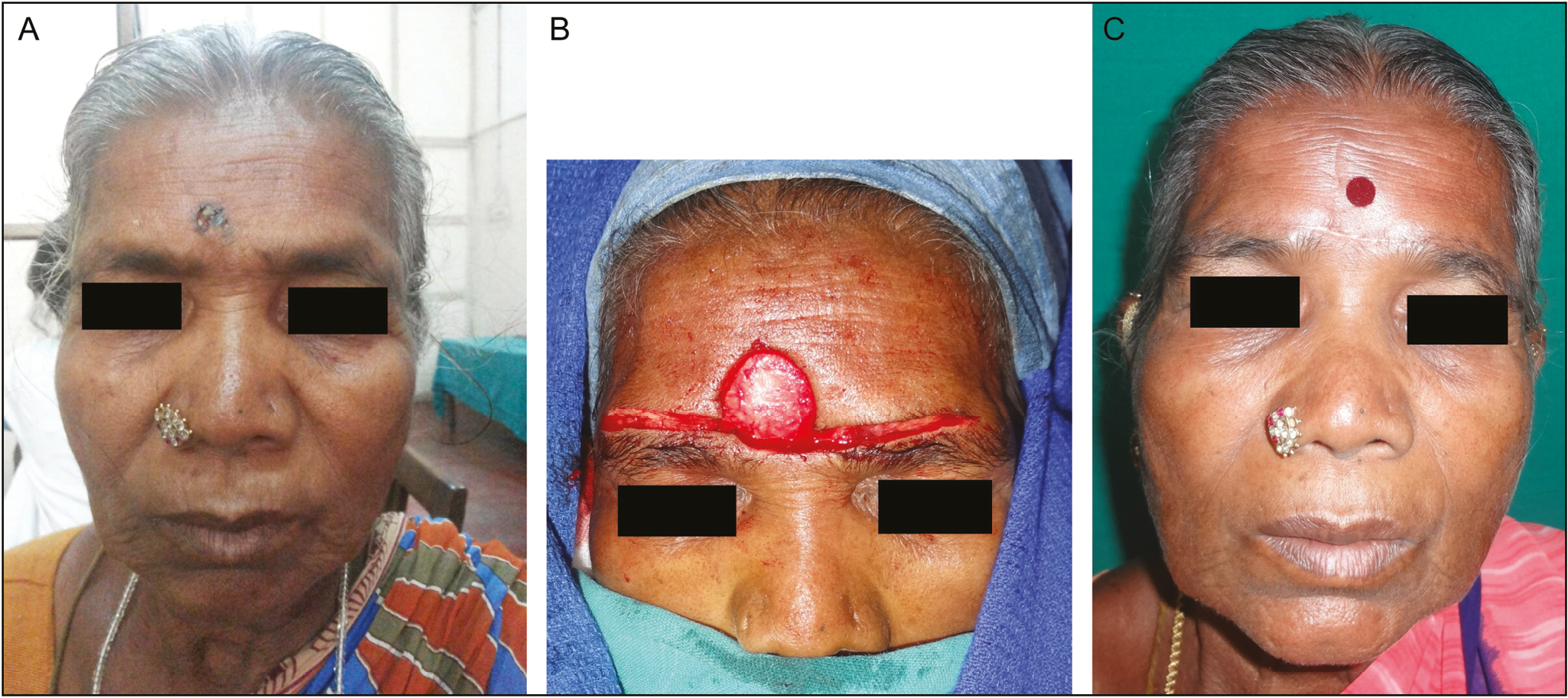
Approximately 77.3% defects were reconstructed using local flaps, 18.2% underwent SSG, and 4.5% underwent fusiform excision and primary closure [Figure 4]. The most common flap for cheek defects was Limberg flap (48.4%) [Table 3]. The most common flap for nose defects was paramedian forehead flap (70.8%) Figure 5A–D]. In 32.9% (29) cases, reconstruction was a staged procedure. Initial flap inset was given and flap division and final inset were carried out after 3 weeks. Flap division was required in all 29 cases. Flap thinning was carried out in 10 cases.
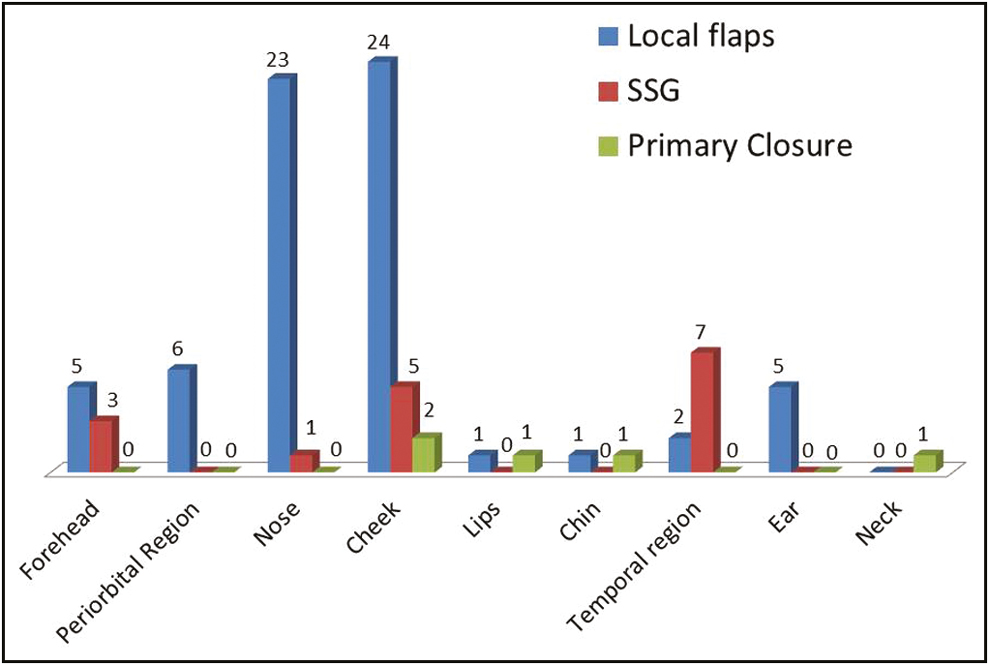
- Reconstruction method used, expressed as percentage for each area

- (A) BCC of nose. (B) Post-excision defect and elevation of paramedian forehead flap. (C) Reconstruction using paramedian forehead flap. (D) Paramedian forehead flap reconstruction after division and inset
Flap donor site wounds were closed primarily, except in two cases of paramedian forehead flap and one case of horizontal forehead flap, which were covered with SSG.
Complications were seen in six cases: two cases with wound dehiscence, two cases with marginal necrosis, one case with partial necrosis, and one case with recurrence [Figure 6]. Both cases of wound dehiscence, seen in rotation flap for cheek, were managed by secondary suturing. Cases of marginal necrosis, one involving the ear and the other involving the nose, were managed conservatively. Partial necrosis was observed in cervicofacial rotation flap for ear and was managed by re-rotation of flap cover [Figure 7]. Recurrence was observed in a case of BCC of the cheek and nose, reconstructed by paramedian forehead flap after 1 year, which was managed by re-excision with a 5-mm clearance and cheek rotation flap Figure 8A–E].

- Rotation flap in cheek, which developed wound dehiscence in the medial aspect

- Partial necrosis of the cervicofacial rotation flap for BCC of ear

- (A) BCC involving right cheek and nose. (B) Reconstruction using paramedian forehead flap. (C) Postoperative picture after flap division and inset of paramedian forehead flap. (D) Recurrence in the lateral aspect after 1 year. (E) Postoperative picture after re-excision and rotation flap
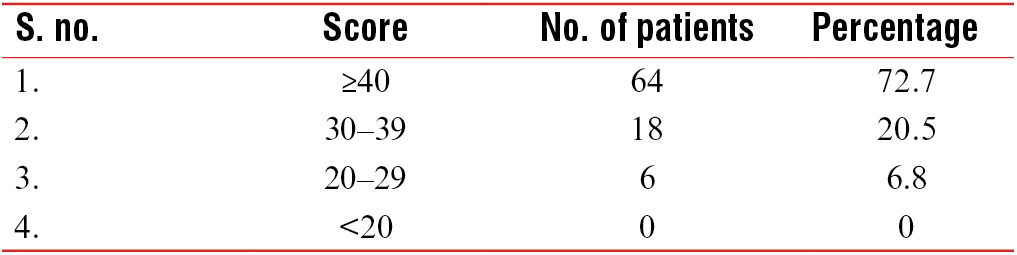
As per the customized PSQ scale and our scoring system, 64 of 88 patients (72.7%) were satisfied with the medical care and reconstruction with a score of 40 and above. Eighteen patients (20.5%) scored between 30 and 39. Thirteen patients had issues with technical quality, three with communication, and two with accessibility and convenience. Six patients (6.8%) scored between 20 and 29, including three cases of flap cover and three cases of SSG. Their primary domain of dissatisfaction was with technical quality. None of the patients scored less than 20 [Table 4].
On the basis of the six main aspects of PSQ III, 24 patients (27.3%) were not satisfied with the medical care. All patients were satisfied with the general aspects of the medical care, interpersonal manner, and time spent with doctor. Nineteen patients (21.6%) were dissatisfied with the technical quality. Among them, sixteen patients underwent SSG and three underwent flap reconstruction. Dissatisfaction was due to color mismatch in SSG, recurrence, pinna excision, and ectropion of lower eyelid. Recurrence was managed by re-excision and flap cover. Ectropion was because of the weight of the flap and was managed by static sling [Figure 9]. The patient with absent pinna secondary to excision was given external ear prosthesis. Color mismatch because of SSG could not be corrected. Among the 24 patients, three (3.4%) were dissatisfied with the communication because of language issues. Two patients (2.3%) were dissatisfied with the accessibility and convenience.

- BCC of cheek reconstructed using horizontal forehead flap showing unsightly scar over forehead and right lower eyelid ectropion
DISCUSSION
Face is the most common site of BCC because of chronic sun exposure. Nose is the most common site of facial BCC, accounting for 25%–30% because of cumulative exposure.[2345678910] In our study, cheek was the most common site accounting for 35.2%, whereas nose accounted for 27.3% of facial BCC. BCC is usually observed in older patients who are frequently and chronically exposed to sunlight. Men are more commonly affected due to their outdoor occupation. In few studies, when the whole head and neck region was encountered, no statistically significant difference between men and women was observed.[11121314] In our study, 55.7% cases were of female patients probably because of dynamic epidemiology of BCC with increasing female preponderance.
Risk factors identified for recurrence of BCC include tumor size (≥2cm), tumors located in the “H zone” of the face (representing embryonic fusion planes and includes portions of the nose, scalp, ears, and lips), recurrent tumors, perineural invasion, poorly defined borders, and more aggressive histologies (infiltrative, morpheaform, or basosquamous histology).[151617]
Giant BCCs are defined as the tumors that are more than or equal to 5cm in its greatest dimension. The most common location of giant BCC is the back.[18] Eight percent of our patients presented with giant BCC of the head and neck.
Though various treatment modalities are available for the treatment of BCC, wide local excision is the standard line of management. Although Mohs micrographic surgery (MMS) has been widely used and has been proven to achieve a high percentage of tumor resection with clear margins, it is not immune to controversies when treating truly aggressive tumors.[1920] Also, frozen section facility is not available in all centers making MMS practically difficult.
After surgical excision, reconstruction is carried out using local flaps, regional flaps, free flaps, or skin grafts. Reconstruction of facial BCC is challenging because equal importance has to be given to clearance, form, function, and patient satisfaction. Local flaps have the advantage of skin color and texture match and are more aesthetically acceptable with minimum donor-site morbidity.
In our study, 77.3% defects were reconstructed using local flaps. The choice of reconstructive procedure depends on several factors, including size, location, and involvement of deeper structures [Figures 10 and 11].[2122] Flaps were chosen for better color and texture match. In our study, most commonly used flap for cheek defects was Limberg flap, which is of single-stage reconstruction type, and for nose defects paramedian forehead flap was used, which is two or three staged depending on the need for thinning [Figure 12A–C]. Split-thickness skin grafting is widely used for primary wound coverage after skin cancer resection because donor-site morbidity is lower and larger donor area is available. SSG was carried out for giant BCC when multiple aesthetic subunits were involved and local flaps were insufficient. SSG was performed only in cases in which underlying bone was not exposed. Defects in the temporal region were predominantly reconstructed using SSG because any local flap would bring down the hairline and would be aesthetically unacceptable. Approximately 93.2% of the cases healed well without any complications.
- (A) BCC of forehead. (B) Post-excision defect over forehead and elevation of advancement flaps. (C) Bilateral advancement flap late postoperative status

- (A) BCC of upper lip right side. (B) Reconstruction using Abbe flap. (C) Abbe flap after division and inset
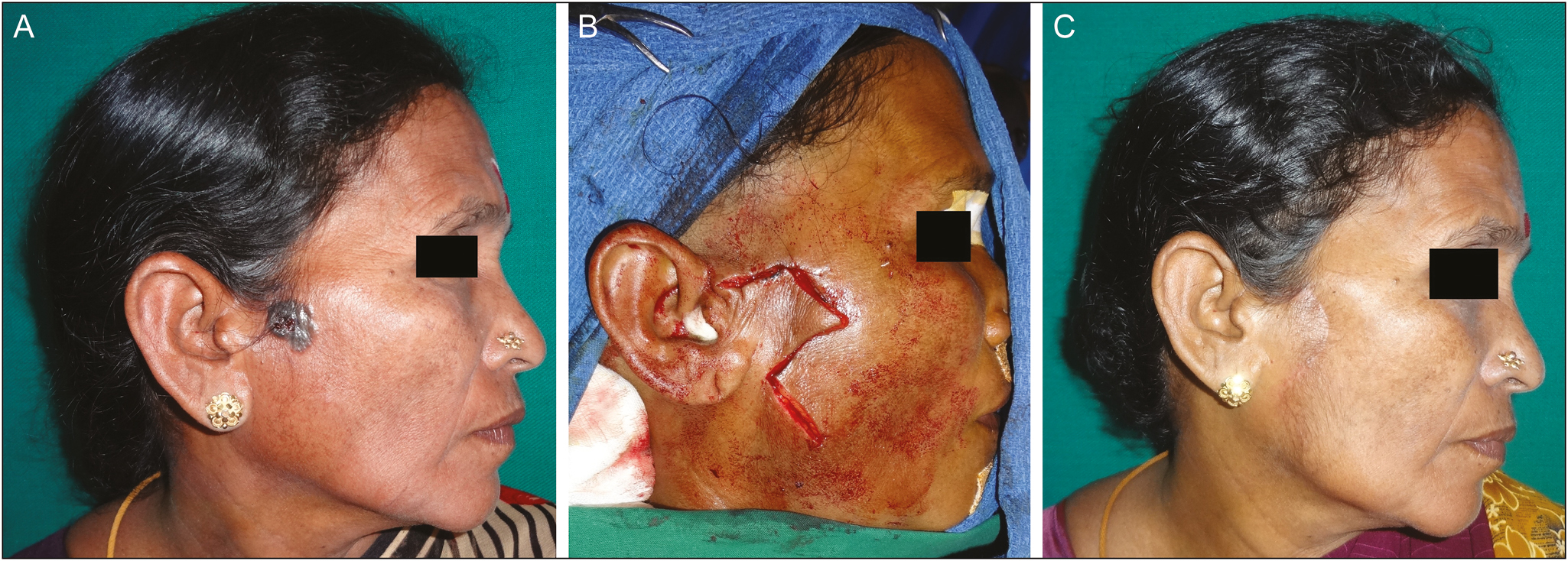
- (A) BCC of right pretragal region. (B) Limberg flap reconstruction. (C) Limberg flap late postoperative status
Patient satisfaction has emerged as a critical outcome of medical care because of the increasing emphasis on patients as consumers of services in the medical marketplace (Davies and Ware, 1988).[232425] Patient satisfaction is not a clearly defined concept, although it is identified as an important quality outcome indicator to measure success of the services delivery system.[26] It is all the more important when reconstructing defects in the exposed regions of the body, particularly, the face and the neck. Ware and his colleagues developed PSQ to assess the quality of medical care.[23] Subsequently, revisions have been introduced. One of the recent versions of PSQ III contains 50 items tapping on the seven aspects of patient satisfaction: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with doctor, accessibility, and convenience.[2427]
Patient satisfaction has been given the least importance in oncological resection surgeries. This is counterproductive in any case of reconstruction of the defects of the face and neck because of the psychological impact the reconstruction has on the patient. An unsightly scar or a formless floppy flap on the face or neck would negatively impact the psyche of the patient and impair normal life [Figures 13 and 14]. Importance of satisfaction in the health system, especially reconstructive surgery, is more than in other services because of the experience of illness and the need to adhere to and follow long treatment process, increased vulnerability of the patients, and requirement of a more comprehensive psychological support.[28] In our study, equal weightage was given to oncological clearance, form and function, and the fourth dimension, which is satisfaction of the patient in terms of reconstruction.
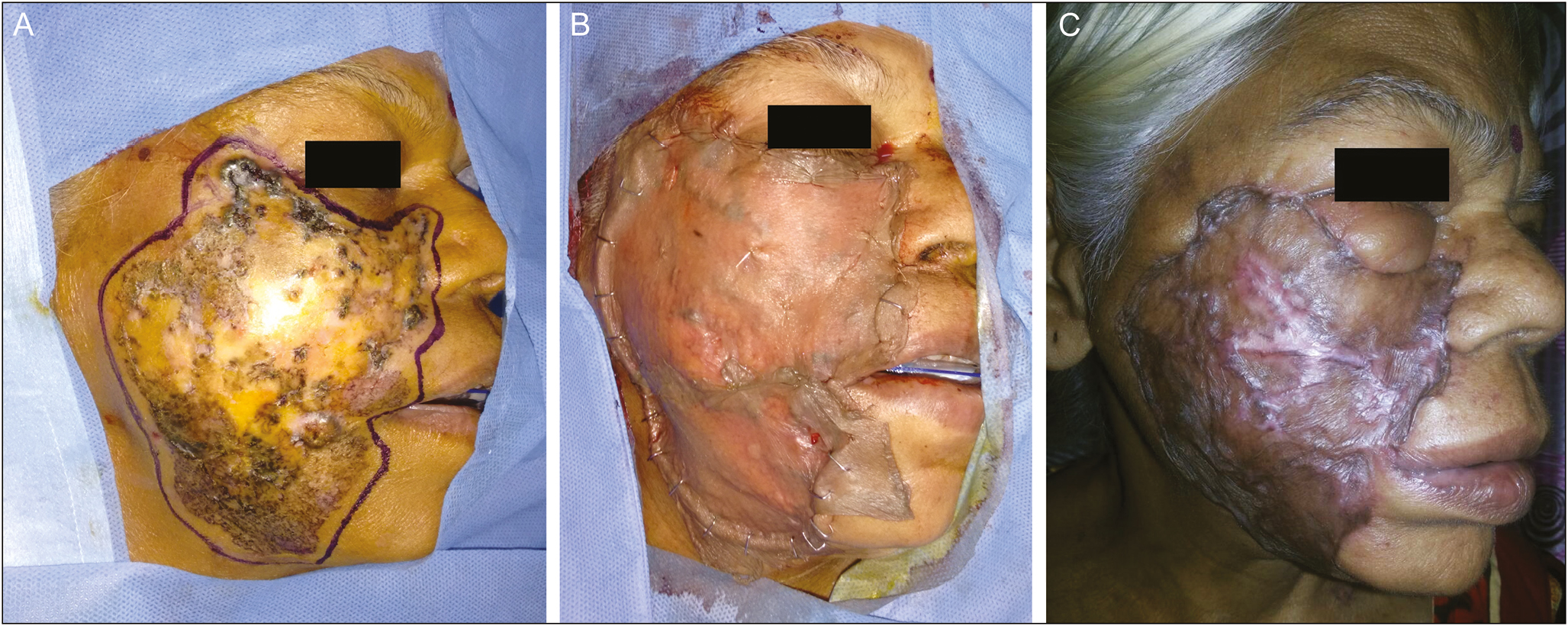
- (A) Giant BCC involving right cheek. (B) SSG applied over the cheek defect after excision of BCC. (C) Hypertrophic scarring of the SSG

- Limberg flap reconstruction in cheek showing trapdoor scar
Skin grafting is usually performed when defects are large and unsuitable for primary closure or a local flap.[29] The patients who underwent SSG were dissatisfied with the cosmesis because of poor texture, color, and contour match. Studies have shown that skin grafting was one of the most useful reconstructive modalities for skin and subcutaneous tissue defects; however, postoperative scars were a determining factor of patient satisfaction, in particular, the color match between the grafted skin and the surrounding recipient skin was important.[30] The reconstruction poses a challenge for the surgeon when the lesions are large, the depth of resection exposes bone, and when like or local tissues are paucity. The risk–benefit balance and the choice of reconstruction were explained to all patients. Though initially accepted, on late post-op follow-up, the patients were discontented with the end result. Fulfilling the four dimensions was more possible with local flaps than with SSG. The patients with smaller lesions and those with lesions in the lateral segments of the face were easily satisfied with the reconstruction. In the central segment of face, some patients who were initially unhappy were satisfied after flap thinning. As reconstructive surgeons, our main aim is to provide a method of reconstruction where donor tissue resembles native tissue, contour match is good, suture line scars are less obvious, and complications are nil. This brings about a better patient satisfaction.
CONCLUSION
Post-excisional defects of BCC in the head and neck region have to be reconstructed with equal weightage to all the dimensions of oncological reconstruction: clearance, form, function, and patient satisfaction. Though split-thickness skin grafting is an easier option, it is fraught with unsightly scars on healing. Local flaps have good color and texture match and are sensate, making them ideal for reconstruction of facial defects. Facial animation is also better restored after flap reconstruction. Thus, local flaps are better in satisfying the fourth dimension of reconstruction, which is patient satisfaction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Basal cell carcinoma: an overview of tumor biology and treatment. Plast Reconstr Surg. 2004;113:74E-94E.
- [Google Scholar]
- Nonmelanoma skin cancer of the head and neck II: surgical treatment and reconstruction. Am J Otolaryngol. 2009;30:181-92.
- [Google Scholar]
- Facial basal cell carcinoma: analysis of recurrence and follow-up strategies. Oncol Rep. 2011;26:1423-9.
- [Google Scholar]
- Incomplete excision of basal cell carcinoma: rate and associated factors among 362 consecutive cases. Dermatol Surg. 2007;33:1207-14.
- [Google Scholar]
- Treatment of facial basal cell carcinoma: a review. J Skin Cancer. 2011;2011:380371.
- [Google Scholar]
- Actinic keratosis, basal cell carcinoma and squamous cell carcinoma. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. Beijing, China: Elsevier Saunders; 2012. p. :1773-93.
- [Google Scholar]
- Epidemiology of surgical treatment of nonmelanoma skin cancer of the head and neck in Greece. Dermatol Surg. 2010;36:15-22.
- [Google Scholar]
- Age and site prevalence of histologic subtypes of basal cell carcinomas. Int J Dermatol. 1995;34:174-6.
- [Google Scholar]
- Basal-cell carcinoma in temperate and tropical Australia. Int J Cancer. 1992;50:874-5.
- [Google Scholar]
- Basal cell carcinoma of the head and neck region: a retrospective analysis of completely excised 331 cases. J Skin Cancer. 2014;2014:858636.
- [Google Scholar]
- Head and neck cancer: a multidisciplinary approach (4th ed). Philadelphia, PA: Lippincott Williams & Wilkins; 2014.
- Histologic pattern analysis of basal cell carcinoma. Study of a series of 1039 consecutive neoplasms. J Am Acad Dermatol. 1990;23:1118-26.
- [Google Scholar]
- AJCC cancer staging manual (7th ed). New York: Springer; 2010.
- Giant basal cell carcinoma: clinicopathological analysis of 51 cases and review of the literature. Anticancer Res. 2009;29:2655-63.
- [Google Scholar]
- Applications of kite flap in reconstruction of cheek defects after tumour excision. MJMS. 2012;5:313-6.
- [Google Scholar]
- Surgical management of skin cancers of the head and neck. Open access atlas of otolaryngology head and neck operative surgery 2017:8-10.
- [Google Scholar]
- The Patient Satisfaction Questionnaire short-form (PSQ-18). Santa Monica, CA: RAND; 1994.
- Reconstruction of large facial defects after delayed Mohs surgery for skin cancer. Acta Dermatovenerol Croat. 2015;23:265-9.
- [Google Scholar]
- Patient satisfaction survey as a tool towards quality improvement. Oman Med J. 2014;29:3-7.
- [Google Scholar]
- A comprehensive review of head and neck cancer rehabilitation: physical therapy perspectives. Indian J Palliat Care. 2012;18:87-97.
- [Google Scholar]
- Satisfaction in orthopedic patients based on patient satisfaction questionnaire (PSQ) Int J Med Invest. 2015;8:214-21.
- [Google Scholar]
- V-Y advancement flap for reconstruction of defects after excision of basal cell carcinoma of the face. Int J Surg Res. 2014;3:15-8.
- [Google Scholar]
- Comparison of local flaps and skin grafts to repair cheek skin defects. J Cutan Aesthet Surg. 2015;8:92-6.
- [Google Scholar]






