Translate this page into:
Surgical Management of Onychopapilloma, Onychomatricoma, and Subungual Osteochondroma: Case Series
Address for correspondence: Dr. Swagata Arvind Tambe, 19/558, Udhyan Society Nehru Nagar, Kurla East, Mumbai, Maharashtra 400024, India. E-mail: swagatatambe@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The clinical diagnosis of benign and malignant nail tumors can be difficult. Dermoscopy can provide a clue to the diagnosis but nail biopsy is the gold standard in establishing the diagnosis. Here, we report three cases of rare nail tumors, that is, onychopapilloma, onychomatricoma, and subungual osteochondroma, which were diagnosed on histopathology and managed surgically.
Keywords
Onychomatricoma
onychopapilloma
subungual osteochondroma Keymessage: Diagnosis of nail tumors is often difficult compared to their skin counterparts. This is probably because the nail can obscure the lesion or many nail tumors mimic inflammatory dermatoses of the nail unit. Histopathological diagnosis and appropriate surgical excision play an important role in the effective management of nail tumors and prevention of future recurrences.
INTRODUCTION
Tumors of the nail unit are more often clinically misdiagnosed than their skin counterparts. This is probably because the nail can obscure the lesion or many nail tumors mimic inflammatory dermatoses of the nail unit. As a general rule, benign lesions respect the general architecture of the nail apparatus, whereas malignant ones are destructive.
CASE HISTORY
Case 1
A 31-year-old man presented with asymptomatic growth below the left thumbnail associated with longitudinal dark pigmentation of the nail plate for 6 years. There was a history of preceding trauma 12 years ago. He underwent complete nail avulsion thrice in the past 4 years followed by recurrence of the lesion.
Cutaneous examination revealed longitudinal melanonychia with firm verrucous mass near the distal end of nail plate [Figure 1A and B]. Rest of the nail plate was normal.

- Case 1. (A) Longitudinal melanonychia with mass near the distal end of nail plate. (B) Verrucous subungual mass lesion extending beyond distal nail plate, compressing hyponychium. (C) Postoperative day 5. (D) Histopathology of excised tumor showing areas of acanthosis, distal papillomatosis (40×, hematoxylin–eosin). (E) Fusiform cells seen with eosinophilic cytoplasm forming stratified layer with V-shaped configuration resembling keratogenous zone of nail matrix (400×, hematoxylin–eosin)
For diagnosis, excision biopsy was planned. Nail plate was separated from the tumor and avulsion was carried out under proximal digital block to expose the tumor. Elliptical longitudinal incision was made around the tumor till the distal part of the matrix and the tumor was excised. Two parallel relaxing incisions were made on either side of the wound to create flaps. Undermining was carried out on both the sides and the defect was closed with reapproximation of both the flaps with interrupted sutures by 5-0 nonabsorbable, nylon suture [Figure 1C]. Sutures were removed on the 7th day. Histopathology of the excised tumor revealed acanthosis with distal papillomatosis. In areas of distal papillomatosis, fusiform cells were seen with eosinophilic cytoplasm forming stratified layer with a configuration of “V” shape resembling keratogenous zone of nail matrix, suggesting diagnosis of onychopapilloma [Figure 1D and E].
Postoperatively, the patient showed complete nail growth without any recurrence of tumor even after 3 years of follow-up [Figure 1F].
Case 2
A 50-year-old woman presented with dark discoloration and thickening of right ring fingernail for 6 years. A history of occasional pain in the lesion on pressure was reported. There was no history of preceding trauma, drug intake for prolonged duration, diabetes mellitus, or hypertension.
Cutaneous examination revealed thick band of longitudinal melanonychia with linear subungual mass lesion under right ring fingernail, involving almost three-fourth of the surface area of nail plate. Increased curvature of nail plate was observed [Figure 2A and B]. Dermoscopic examination revealed a clear demarcation between the subungual mass lesions from the unaffected nail plate. Multiple linear hyperpigmented striations and grooves on the nail plate arising from the nail matrix were seen. Subungual mass lesion was inseparable from the affected nail plate. Multiple concentric areas were seen on the frontal view containing yellowish material. The tumor was firmly attached to the hyponychium [Figure 2C and D]. High-frequency ultrasonography of the lesions revealed hypoechoic nail bed that was compressed between the tumor and the distal phalanx. Nail plate was uniformly thickened with multiple circular hyperechoic bands within it [Figure 2E].
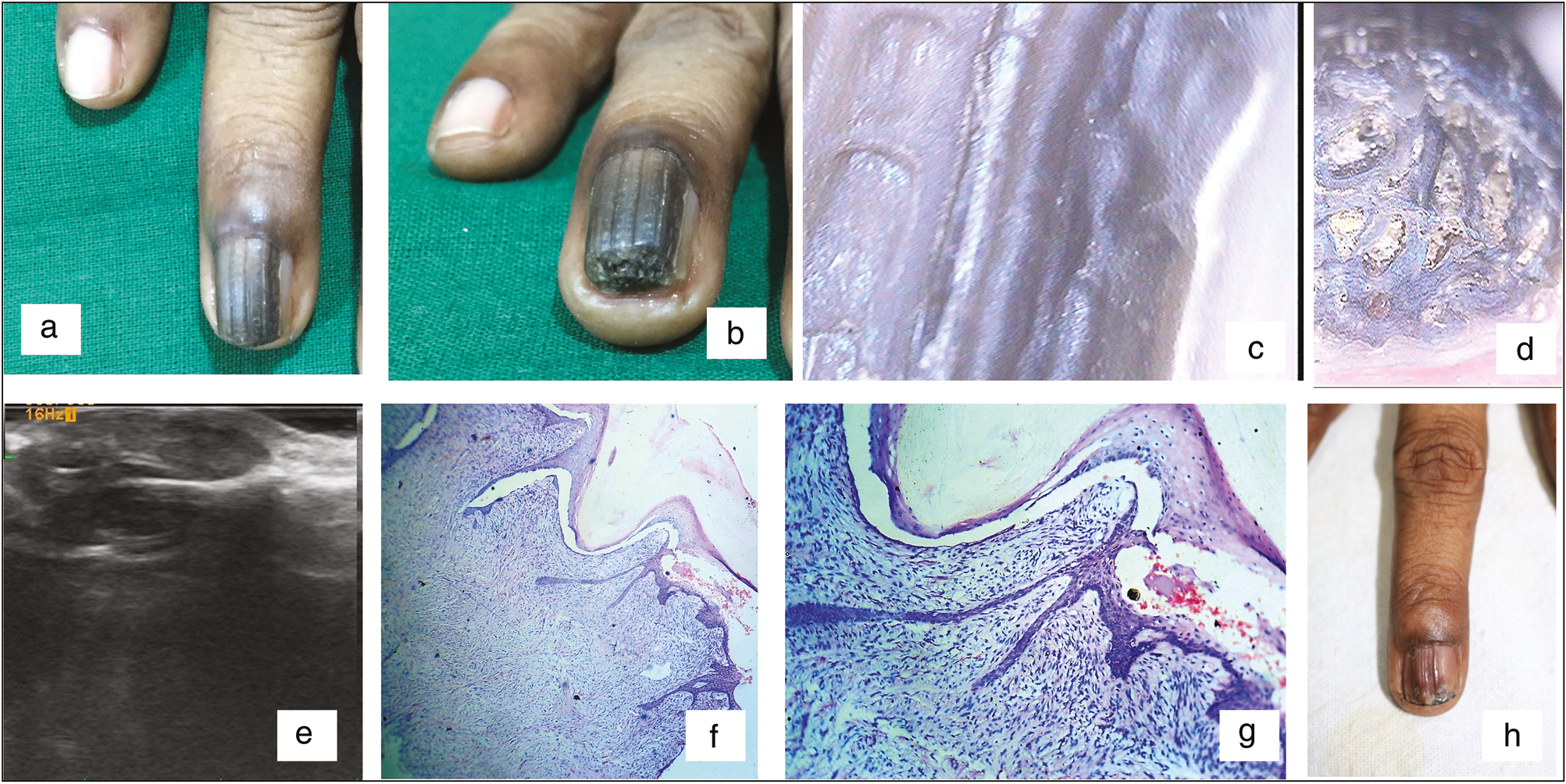
- Case 2. (A, B) Longitudinal melanonychia with linear subungual mass lesion with increased curvature of nail plate. (C, D) Dermoscopy: multiple linear grooves on the nail plate and multiple concentric areas containing yellowish material. (E) High-frequency ultrasonography: thickened nail plate, multiple circular hyperechoic bands within it. Hypoechoic nail bed compressed by the tumor. (F, G) Fibroepithelial tumor with filiform projection of dermis covered with a thin rim of epidermis (hematoxylin–eosin, 40× and 100×). (H) Four months after surgery
The tumor was excised under proximal digital block anesthesia. The procedure was performed by making two lateral oblique incisions at 45degrees at the junction of proximal and lateral nail folds to expose the proximal extension of the tumor. As the tumor was covering almost three-fourth surface area of the nail plate, complete nail avulsion was carried out. During excision, multiple fibrous projections of the tumor were noticed on retracting the proximal nail fold. The tumor was shaved from the matrix with the surgical blade. Proximal nail fold was replaced back and two lateral incisions were sutured.
Histopathological examination of the specimen revealed a fibroepithelial tumor with filiform projection of dermis covered with a thin rim of epidermis confirming the diagnosis of onychomatricoma [Figure 2F and G].
After 4 months, the patient showed reduction in size of the tumor with linear atrophic hyperpigmented band suggesting postsurgical scarring [Figure 2H].
Case 3
A 16-year-old girl presented with a growth that was slowly growing under the right great toenail for 6 months with a history of preceding trauma. Cutaneous examination revealed a single firm, fleshy nodule of size 1×1cm over medial and distal aspect of right great toe, displacing the nail plate without dystrophy, bleeding, eschar, and erosion [Figure 3A and B]. Differential diagnoses of subungual exostosis, subungual fibroma, and glomus tumor were considered. Radiography showed radio-dense outgrowth arising from dorsomedial aspect of distal phalanx of the right great toe in continuity with medullary canal [Figure 3C], suggesting diagnosis of subungual exostoses or osteochondroma. The tumor was removed under proximal digital block anesthesia. A shark-mouth incision was made across the hyponychium to reach the dorsal plane of distal phalanx. The tumor was resected using an osteotome and curettage of base was carried out. Closure of the incision was carried out in layers. Excised specimen on light microscopy revealed well-defined trabecular bone covered with hyaline cartilage cap suggesting the diagnosis of subungual osteochondroma [Figure 3D and E]. Even after 3 years of excision, no clinical or radiographic evidence of the tumor is reported [Figure 3F].
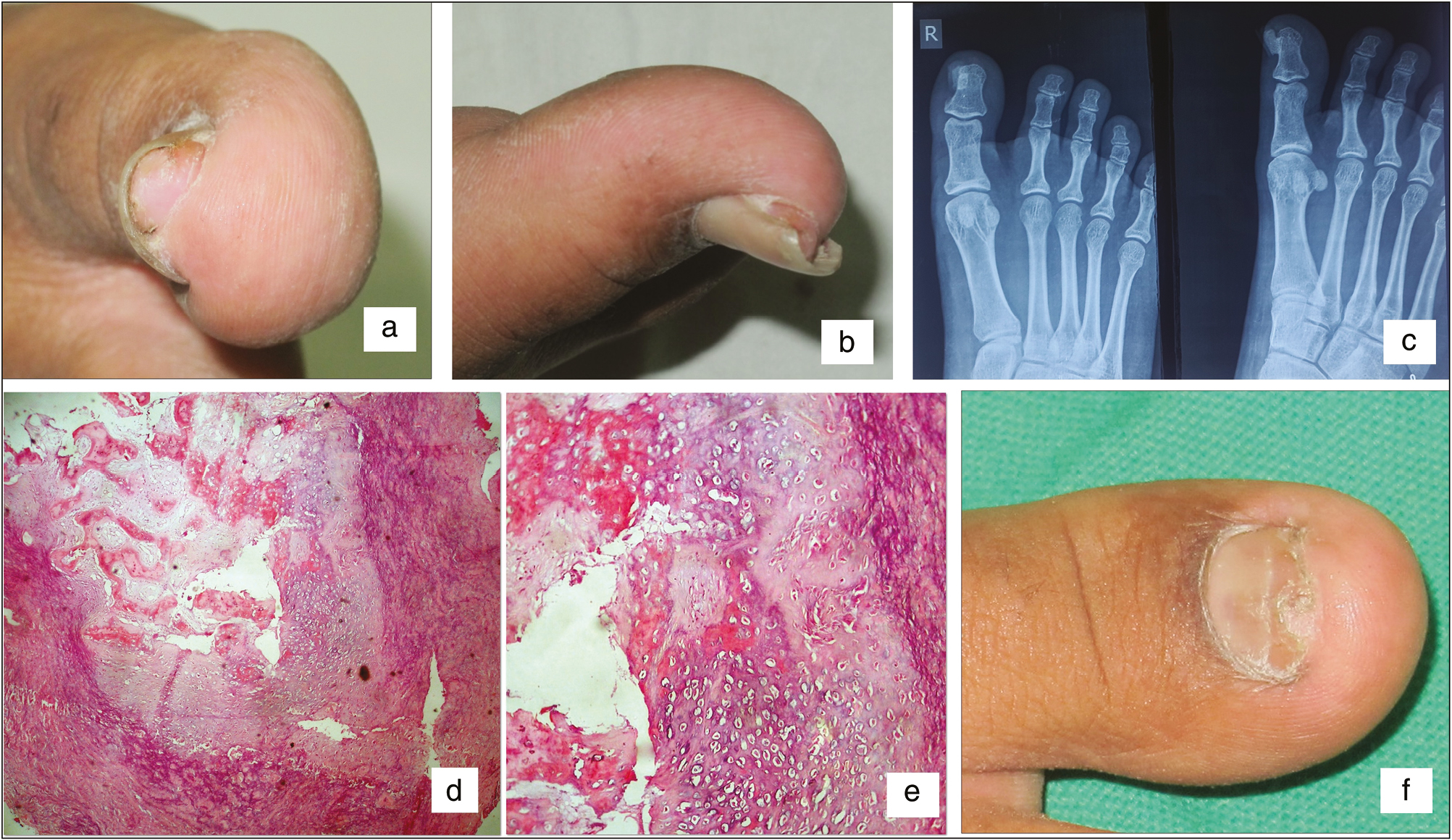
- (A) Single firm, fleshy nodule of size 1×1cm over medial and distal aspect of right great toe, displacing the nail plate (anterior view). (B) Tumor on lateral view. (C) Radiography: radio-dense outgrowth arising from dorsomedial aspect of distal phalanx of right great toe in continuity with medullary canal. (D) Histopathology, mature trabecular bone covered with hyaline cartilage cap (hematoxylin–eosin, 40×). (E) Hyaline cartilage cap containing perichondrium, chondroblasts, and chondrocytes with lacunae. (F) Two months after surgery
DISCUSSION
Onychopapilloma is an uncommon benign tumor of the distal matrix and nail bed characterized by localized distal subungual keratosis.[1] The most common clinical presentation of onychopapilloma is localized longitudinal erythronychia, but it can present as chromonychia or longitudinal melanonychia. Acanthosis, papillomatosis, and a keratogenous zone in the distal nail bed identical to the nail matrix with eosinophilic cells arranged in a V shape at the base of the keratogenous zone are typical histologic features.[2]
Excision of the nail tumor is the treatment of choice. Partial or total nail avulsion can be carried out to expose the tumor depending on the size of the lesion. Nail bed around the lesion is excised in a longitudinal ellipse without a safety margin. The most proximal part of ellipse should include distal matrix to avoid recurrence of lesion. The tumor is carefully dissected from the bone starting from hyponychium to the proximal end. If the defect is less than 4mm and allowed to heal by secondary intention then the risk of onycholysis is present. Hence, it is advisable to suture the defect with absorbable sutures. Defect larger than 4mm should be closed by two lateral flaps. Improper technique may lead to onycholysis and formation of thinner and easily breakable nail plate. Poor matrix suturing may result in split in nail matrix.[3]
Onychomatricoma is an uncommon subungual tumor of nail matrix origin. Although uncommon, the tumor has a unique set of clinical and pathological features that allow its differentiation from the more common ungual and periungual tumors, especially subungual fibroma and digital fibrokeratoma. In the reported cases, it was found that the tumor generally affects middle-aged to older adults with a mean age of 48 years and a range of 4–72 years. Male and female are equally affected, and the fingernail involvement is approximately twice as common as the toenail.[4] Clinically, the affected digit shows a thickened, yellowed, overcurved nail with proximal splinter hemorrhages and cavities. Beneath the dystrophic nail is a polypoid and filiform nail tumor. Histologically, onychomatricoma is a biphasic fibroepithelial tumor with a lobulated and papillary growth pattern, which recapitulates aspects of normal nail matrix histology.[5]
Complete excision, to include normal nail matrix proximal to the lesion, is generally recommended for therapy and to prevent recurrence. Newly grown nail may show mild dystrophy such as irregularity of the nail plate or discrete erythronychia at the location of previous xanthochromia.
Nail plate dystrophy can be observed especially when the tumor is larger, deeper, and cannot be completely removed without hurting the matrix.[3]
Subungual osteochondroma is a relatively rare, benign osteocartilaginous tumor occurring mainly in the second and third decades of life. It affects both sexes equally. They are most commonly seen in the distal phalanx of the great toe. However, other toes may be involved. Clinically, it appears as a small, pink-colored, hard nodule that projects beyond the free edge of the nail. The overlying nail may become brittle and may be lifted or become detached. The exact etiology of subungual osteochondroma is unknown, although trauma, hereditary abnormality, chronic irritation, and long-standing infection have been suggested as possible etiologies.[67]
Surgical excision is the appropriate management of this condition. Excision is usually performed under digital block anesthesia. Techniques of surgical approaches are usually by a direct dorsal surgical incision or by fish-mouth type of incision. Dorsal surgical incision is usually preferred for protruding exostoses, whereas fish-mouth incision is preferred for non-protruding exostoses. After the mass excision, some authors preserve the nail bed, whereas others prefer partial or total nail bed excision to avoid recurrence. Nail bed excision may cause nail deformities, delay in return to daily activities with difficulty in wearing shoes, and unacceptable cosmetic outcome.
Rapid recovery and excellent cosmetic appearance are achieved using a fish-mouth approach. Few studies reported local recurrence rate of 30% with this technique compared to dorsal surgical approach with the nail bed excision,[8] whereas other studies did not report any recurrence.[9]
Here, we report three cases of rare nail tumors, which were treated surgically with minimal deformity and without any recurrence.
The diagnosis of nail tumors by nail biopsy obtained from the appropriate site is still the gold standard. In some tumors, preoperative biopsy is not possible because of larger size of the tumor, hence excision biopsy needs to be done. Knowledge of appropriate surgical techniques is a must to prevent recurrence of tumor and dystrophic nail deformities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen’s disease. Br J Dermatol. 2000;143:132-5.
- [Google Scholar]
- Surgery of the nail bed. In: Richert B, Chiacchio N, Haneke E, eds. Nail surgery. London, UK: Informa Health Care; 2010. p. :59-63.
- [Google Scholar]
- Onychomatricoma: clinical and histopathologic findings in 12 cases. J Am Acad Dermatol. 1998;39:560-4.
- [Google Scholar]
- Rearrangement of the COL12A1 and COL4A5 genes in subungual exostosis: molecular cytogenetic delineation of the tumor-specific translocation t(X;6)(q13-14;q22) Int J Cancer. 2006;118:1972-6.
- [Google Scholar]
- Subungual exostosis: a review of 16 cases focusing on postoperative deformity of the nail. Ann Plast Surg. 2005;55:272-5.
- [Google Scholar]
- Protruded and nonprotruded subungual exostosis: differences in surgical approach. Indian J Orthop. 2014;48:49-52.
- [Google Scholar]






