Translate this page into:
Logic of Hair Transplantation
Address for correspondence: Dr. Aniketh Venkataram, The Venkat Center for Skin and Plastic Surgery, Bangalore, India. E-mail: draniketh@venkatcenter.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hair transplant is a seemingly illogical process wherein we are using a small number of hairs to cover a large area of baldness. This is possible if one understands the logic of this equation. Understanding the pattern of hair distribution, and the sequence of balding, helps us learn the limitations of this technique and give the best possible results to the patient. In this article, we aim to give an understanding of all the processes associated with hair transplantation and the logic behind the same.
Keywords
Hair transplant
hair transplantation
logic
INTRODUCTION
Hair transplantation (HT) is a technique, which has become popular over the years, because of sound scientific logic and consistency in results. The basic principles need to be properly understood to understand the possibilities and limitations of this procedure and to optimize donor usage, plan the overall treatment, and achieve satisfactory recipient cover. This article briefly outlines the logic and basic principles of HT.
Smaller donor for the bigger recipient: One of the fundamental principles of HT is that of using a small area of donor hair to cover a much larger recipient site by creating an illusion or impression of fullness. Behind this is seemingly imbalanced equation, which is as follows:
-
Small donor versus large recipient area: The occipital donor is just about one-third the size of the potential bald area. So, the amount of hairs available is always less than what the patient had on the bald area and hence the exact number of hairs is not available for transplantation. Still it is possible to achieve good results in HT as it is necessary to provide only 50% of actual density to provide fullness or an impression in appearance (sometimes referred to as illusion of density) or the cosmetic density. Hence, a density of usually 35–40/cm2 is adequate.
-
Fullness or volume is achieved because of a combination of factors, such as number of hairs, thickness of hairs, length, color, and curliness of hairs. In particular, the radius (r) of hair is important as the volume of hair (which is a cylinder) is 3.14 × r × r × length. Occipital hair is thicker than frontal hair. Hence, this increase in radius gets squared and leads to a geometric increase in volume. Likewise, long hairs and curly hairs cover a larger area.
FOLLICULAR UNIT
A follicular unit can have 1–4 hairs with the arrectores muscle, sebaceous gland, perifollicular collagen, and nerves and vessels supplying the unit. There is a certain amount of dermis in between the units. The unit is pyramid in shape, the narrowest part being at the junction of arrectores and the widest at the bottom where the hairs splay. The segment below the arrectores is the inferior segment, which is the temporary segment of hairs (as it disappears during telogen) and hence is loosely attached.[1]
Logic of the follicular unit:
-
The more the number of hairs and thickness of hair per unit, the better the appearance.
-
Harvesting by follicular unit excision (FUE) needs only release of the hold of arrectores and hence excision needs to be only up to the level of arrectores. Going deeper to the base of the unit will transect the unit due to splaying of hairs in the lower part of the unit.
-
As the unit is narrowest at the top, up to the level of the unit, a small punch is adequate to reach this level, which results in a small hole and this results in the dramatically quick healing and the minimal scar.
Variables: Two variables to the above scenario, which make FUE process liable for transection or damage to hairs, are as follows:
-
As the level of attachment of arrectores is not the same in all hairs, in all units, in all areas, and in all patients, and also because FUE process is blind, precise depth of the introduction of punch is variable.
-
In addition to the hold of arrectores, there is one other factor, which holds the unit within the dermis—perifollicular plexus of collagen. The amount of collagen and hence the tightness of the hold may vary from area to area and person to person.
-
As the bulge containing the stem cells is located at the attachment of arrectores to the shaft; any damage to arrectores may also cause some damage to stem cells, though this risk may be theoretical.
-
These factors have led to varying degrees of transection and lower quality of grafts during FUE. However, with increasing machination, automation, and experience, these factors are being overcome with a great improvement in transection rates.
HAIR DISTRIBUTION
A scalp is usually 500cm2 (50,000mm2) in area, with a follicular unit distribution of 1/mm2. Each follicular unit has on average two hairs. This leads to a total hair count of 100,000.[2]
It is important to differentiate follicular unit density, which remains relatively constant at 1/mm2 from hair density, which varies from 1.5 to 3/mm2 (normal = 2/mm2). Hence, the hair density is a function of the number of hairs per follicular unit rather than the total number of follicular units.[3]
Logic of hair distribution:
-
Donor area with a lower hair density will need more number of follicular units than a donor with a higher hair density to achieve the same result [Figure 1].
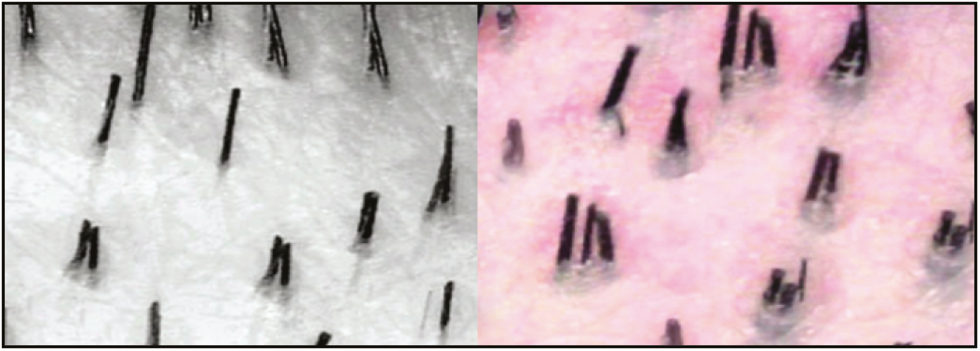
- Comparison of low and high hair density on trichoscan
PROCESS OF BALDING
In the process of balding, the number of follicular units (per mm2) remains constant; the thinning appearance is due to the reduction in the number of hairs per follicular unit. An average person can lose up to 50% of hair, before it is noticeably thin (i.e., a hair density of 1/mm2).
Hence, while performing transplantation from the unaffected donor area, a follicular unit density of 0.5/mm2 is required in the frontal hairline to achieve a hair density of 1/mm2 and appear normal. In areas behind the hairline, where layering and weighting can add value, less than 50% of the original density may be enough to achieve fullness.
Logic of the process of balding:
-
It is not possible to provide normal density in any patient nor is it possible to cover a stage VII scalp with just the occipital donor.
-
What is possible is to provide cosmetic density, to create an illusion of a full head of hair.
DONOR SITE
Of the total 50,000 follicular units on the scalp, 75%, that is, 37,500 are on the frontal region and vertex and hence are at risk of being lost. The permanent donor area has 25%, that is, 12,500 units. As we need 50% to appear normal, this means that a maximum of 6,250 follicular units are available for transplantation. So, in a worst-case scenario, we would have 12.5% (6,250) follicles available to cover 75% (37,500) area, achieving a density of one-sixth (18%) of normal.[4]
This formula teaches us that spacing the follicular unit is most important to achieve fullness. If we try to combine follicular units to increase density, the ratios get more skewed, because of higher intervening areas between units, and a more sparse overall appearance.
Another factor that affects this formula is the hair density. The aforementioned formula refers to a normal hair density of 2 hairs/mm2, or 2 hairs per follicular unit. The effect of any change in this density is magnified in the donor supply as shown in Table 1 as explained by Bernstein and Rassman.[4]
| A | Donor Hair Density (hairs/mm2) | 3.0 | 2.5 | 2.0 | 1.5 | 1.0 |
| B | Follicular Unit Density (units/mm2) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| C | Total Hair in Permanent Zone | 37,500 | 31,250 | 25,000 | 18,750 | 12,500 |
| D | Follicular Units in Permanent Zone | 12,500 | 12,500 | 12,500 | 12,500 | 12,500 |
| E | Hairs that must Remain in Permanent Zone | 12,500 | 12,500 | 12,500 | 12,500 | 12,500 |
| F | Movable Hairs (C–E) | 25,000 | 18,750 | 12,500 | 6,250 | 0 |
| G | Average Hairs per Follicular Unit (G=A) | 3.0 | 2.5 | 2.0 | 1.5 | 1.0 |
| H | Transplantable Follicular Units (F/G) | 8,333 | 7,500 | 6,250 | 4,167 | 0 |
Thus, for example, a hair density of 2.5 hairs/mm2 will have 50% more movable hair than 2 hairs/mm2, even though the increase in hair density is only 25%. This is because the posttransplant donor density to be maintained remains constant at 1/mm2 and does not vary with changes in pretransplant density. So any change in the hair density will have its effect only in the transplantable donor hair. In other words, whether the pretransplant donor density is 3 or 1.5 hairs/mm2, after transplant, the final donor density must be 1 hair/mm2 to avoid looking thin.[4]
Logic of the donor site:
-
The donor area mathematically has around 6000 follicular units that can be harvested safely in an average individual.
-
This number increases with any increase in hair density.
FOLLICULAR UNIT TRANSPLANTATION BY STRIP HARVESTING
In follicular unit transplantation (FUT), all the follicular units from a strip of skin in the center of the occipital area are harvested. What this means is, although the total number of follicular units in the donor area is reduced, the area is reduced as well. So the follicular unit density in the rest of the donor area remains the same. This means that FUE or another FUT can easily be performed in the rest of the donor area.
In strip technique, the strip is elliptical—it is rectangular for most part of its length except at the ends where it becomes roughly triangular. The formula of area of a rectangle is length × breadth. A 20×1cm strip has an area of 20cm2. If density per 1cm2 is 70, a 20cm2 strip would give roughly 1400 units and would contain 2800 hairs if the hair density is 2 hairs per unit
Logic of FUT:
-
FUT does not change the donor-site density, which makes it amenable for another harvest later. It also harvests hairs from the best part of the donor area.
FOLLICULAR UNIT EXCISION
In FUE, fewer units are harvested from a larger area. So this means that the number of units are reduced but the area remains the same. Hence, the donor-site density is reduced by FUE. This has to be kept in mind when planning a repeat harvest.
To harvest without causing thinning, no two consecutive hair units can be taken, so that the maximum gap between two follicular units after harvest will not be more than 2mm. The key to remember is that unlike FUT, as FUE harvest is over a wider area, this formula has to be followed in the vertical as well as the horizontal direction, meaning that every 1 in 4 follicular units can be harvested so that the gap between units is less than 2mm in all directions. Along with the permanent donor, part of the adjoining temporal region can also be harvested as there is no donor scar, thus the total available donor follicles are in the range of 16,000–18,000. It is important not to stray into nonsafe areas of donor in the zeal to harvest greater numbers.
With the one-in-four formula, this gives us a maximum of 4000–4500 available donor follicles. However, the method allows to selectively harvest those units with 3–4 hairs over those with only 1–2 hairs.[5]
Logic of FUE:
-
FUE harvest reduces the donor density, which has to be kept in mind to avoid thinning of the donor site.
-
It is also important to keep this in mind for the sake of future transplants.
Thus, although FUE gives us access to a greater donor area, the proportion of units that can be harvested is less. In contrast, though FUT gives access to a smaller donor area, we can harvest all the follicles from that area without changing the density.
Thus, these two techniques can be combined for maximum possible harvest and best result. For example, a strip of 30cm length and 1cm width and density of 80 units/cm2 can give 2400 units. FUE from above and below the strip can give another 2000–2500 units in the same session. Hence, close to 5000 units can be obtained in one session by combining the two methods, which would not have been possible by one method alone.
RECIPIENT SITE
Calculating the number of grafts required:
The frontal area is triangular and calculated by ½ × breadth × height. The vertex is circular and calculated by π × r2. As the normal number of follicular units is 100 and we need 50%, the total area multiplied by 40–50 (depending on the hair density) gives us the number of follicular units needed.[6]
For example, area of a triangle of width = 20cm and height = 7cm in frontal area (stage 5 baldness: ½ × breadth × height) is ½ × 20×7 = 70cm2 × 40 units/cm2 = 2800 units are the number of follicular units needed.
PLANNING THE HAIR TRANSPLANTATION
Hence to achieve fullness, we need to use our precious supply of follicular units judiciously. The most important component of this is long-term planning. If sequential transplantations might be needed, then each stage should be carried out keeping the final picture in mind. If, for example, the first stage is performed at the age of 25 years, it should be carried out to achieve the overall density that will be present at the age of 45, else we would end up having high density in one area and low in another.[3]
The second key factor is understanding the follicular density. It is important while planning to remember that if we are trying to achieve high density in one region, such as the hairline, another region will have to compensate with a lower density. This can be used to our advantage. If a person combs from left to right, it makes sense to give a higher density on the left side of the scalp. If the patient leaves his hair longer, it would cover a greater area of scalp and give a better visual appearance. This also explains why it is more difficult to give a good result in the vertex as the hairs move in different directions and do not layer over each other.
Logic of planning hair transplantation:
-
Although the recipient area can increase with time, the donor area remains constant. It is important to plan for the future and not for just one surgery.
Logic of body HT:
One great advancement that has been brought in the introduction of FUE is its suitability for extracting body and beard hairs. The concept of recipient influence enunciated by Hwang et al.[7] provided logic for such a process. Body hair when transplanted to scalp hair can grow longer and thicker over successive cycles, thus gradually acquiring the characteristics of scalp hair. However, the following contrarian points need to be kept in mind:
-
Body hair occurs mostly as single hair units.
-
Body hairs have an anagen phase of few weeks (6–10 weeks). Even after transplantation to scalp, though some prolongation of the anagen phase may occur, it is unlikely to match the scalp hair.
For these reasons, body hair cannot be a first choice and when transplanted, should be carried out amid scalp hairs.
Beard hair has an anagen phase of several months (1 year), is thicker than scalp hair, and is more suitable than chest hair.
CONCLUSION
Thus, understanding the above logical mathematical principles with regard to hair loss enables the surgeon to plan and economize donor graft supply to achieve a balanced, aesthetically pleasing appearance in the long run and to avoid mistakes and shortsightedness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Transverse microscopic anatomy of the human scalp. A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol. 1984;120:449-56.
- [Google Scholar]
- Follicular transplantation. Patient evaluation and surgical planning. Dermatol Surg. 1997;23:771.
- [Google Scholar]
- The logic of follicular unit transplantation. Dermatol Clin. 1999;17:277-95, viii; discussion 296.
- [Google Scholar]
- Follicular unit extraction: minimally invasive surgery for hair transplantation. Dermatol Surg. 2002;28:720-8.
- [Google Scholar]
- Changing trends in hair restoration surgery. Indian J Dermatol Venereol Leprol. 2006;72:103-11; quiz 112, 125.
- [Google Scholar]
- Does the recipient site influence the hair growth characteristics in hair transplantation? Dermatol Surg. 2002;28:795-8. discussion 798-9
- [Google Scholar]






