Translate this page into:
Efficacy of 308-nm Monochromatic Excimer Light in the Management of Halo Nevi: An Open-Label, Pilot Study
Address for correspondence: Dr. Swapnil D. Shah, 441, Shukrawar Peth, Manik Chowk, Solapur 413002, Maharashtra, India. E-mail: drswapnilshah@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Halo nevus (HN) affects approximately 1% of the population. Presence of hypo- or depigmented lesion carries tremendous psychosocial disturbance in the mind-set of population in the Indian subcontinent. Hence, HN requires intervention by any modalities. Here authors attempted to evaluate the efficacy of monochromatic excimer light (MEL) in treating HN.
Materials and Methods:
A total of 29 patients with HN were included in the study. A xenon chloride lamp emitting noncoherent, monochromatic 308-nm light that represents the natural evolution of the excimer laser was used. The initial dose was 100 mJ/cm2, which was increased by 100 mJ/cm2 per session. All the patients were followed up for 6 months.
Results:
A total of 29 patients with 10 males and 19 females (male to female ratio of 1:1.9) completed the study. The age of onset of HN ranged from 5 to 47 years and the mean age of the patients was 23 years. HN was seen on the face, back, neck, chest, trunk, and extremities in 5 (17.2%), 6 (20.7%), 4 (13.7%), and 6 (20.7%) patients, respectively. Outstanding response was noticed in 14 patients (48.2%), whereas 6 (20.6%) patients showed excellent improvement. Only 2 (6.8%) patients showed no response after 10 consecutive sessions.
Conclusion:
HN causes apprehension in the Indian population because of the social stigma associated with depigmented patches on the body. Mere observation and only counseling in the treatment protocol are not sufficient. MEL is a noninvasive procedure, which results in excellent repigmentation of HN without scarring.
Keywords
Halo nevi
monochromatic excimer lamp
308 nm
Depigmentation associated with halo nevi is psychologically disturbing to the patient. Monochromatic excimer lamp is safe and effective and a rapid way to treat these nevi.

INTRODUCTION
Sutton[1] described halo nevi (HNs) as leukoderma acquisita centrifugum in1916. These are common benign melanocytic nevi in which an inflammatory infiltrate develops that result in surrounding zone of depigmentation, giving rise to a halo around the melanocytic nevus.[1] HN affects 1% of the population with no sex predilection.[2] The association between vitiligo and halo nevi is long been debated with some authors consider halo nevi as one end of the spectrum of vitiligo,[3] whereas others consider them as two different entities.[456] HN can be traditionally associated with dysplastic nevus[7] and malignant melanoma.[8] Either of these conditions are extremely rare in Indian subcontinent wherein benign HN is usually encountered. Hypo- or depigmented macules on body impart a lot of psychosocial disturbances in patients with pigmented skin. Various treatment modalities ranging from no intervention[9] to topical tacrolimus,[10] surgical excision of nevus,[11] and excimer laser[1213] are reported in the literature. Monochromatic excimer light (MEL) has a similar mechanism of action to the excimer laser.[14] We decided to use MEL on HN.
MATERIALS AND METHODS
After obtaining ethical clearance and informed written consent, a total of 29 consecutive patients with HN were included in the study. Site and size of HN were noted and respective demographic data were collected. Patients with generalized vitiligo, those treated with phototherapy in the past 3 months and those with a history of immunosuppressive or photosensitizing agents were excluded from the study. A dermoscopic examination of nevus was carried out in all patients to rule out atypical patterns.
Treatment protocol
A xenon chloride lamp emitting noncoherent, monochromatic 308-nm light that represents the natural evolution of the excimer laser was used.
All patients were treated with xenon chloride 308-nm MEL (Exciplex; Clarteis, Valbonne–Sophia Antipolis, France) producing 100 mW/cm2 power density with a total optical power of 2500 mW. The spot size available with this system is 5×5cm. A suitable silicone stencil of the size of HN was used to protect the surrounding skin to prevent burns and post-inflammatory hyperpigmentation. Treatment was started with a fluence of 100 mJ/cm2. The fluence was increased by 100 mJ/cm2 per session until a slight erythema appears after 24h. If there was intense erythema lasting for more than 48h, the next session was skipped until the erythema resolves and the dose was reduced by 100 mJ/cm2. The same dose was continued for the next two sessions and then it was increased by 50 mJ/cm2. Treatment was administered twice a week on nonconsecutive days. If the patient did not show any repigmentation even after 10 sessions, it was considered as treatment failure. And if the patient developed repigmentation in the initial sessions of treatment but did not show further improvement even after 10 continuous sessions, then the patient was labeled as a partial responder and the treatment was discontinued. Clinical photographs were taken in all the patients once a month. Two independent dermatologists evaluated the results by observing the clinical photographs. All the patients were followed up for 6 months. Side effects during the treatment were also recorded. Repigmentation was graded as:
Grade 0: no repigmentation
Grade 1: 1%–24% repigmentation (partial improvement)
Grade 2: 25%–49% repigmentation (good improvement)
Grade 3: 50%–74% repigmentation (very good improvement)
Grade 4: 75%–99% repigmentation (excellent improvement)
Grade 5: 100% repigmentation (outstanding improvement)
RESULTS
A total of 29 patients with 10 males and 19 females (male to female ratio of 1:1.9) completed the study. The age of onset of HN ranged from 5 to 47 years and the mean age of the patients was 23 years. Patient characteristics, the result obtained, and doses used are summarized in Table 1.
| Case no. | Age (years) | Sex | Site | Number of sessions | Max. dose [mJ/cm2] | Mean dose | Percentage of repigmentation (%) | Complication |
|---|---|---|---|---|---|---|---|---|
| 1 | 10 | M | Back | 7 | 700 | 257 | 100 | -- |
| 2 | 12 | F | Lower extremity | 12 | 1000 | 625 | 70 | -- |
| 3 | 42 | F | Chest | 32 | 2200 | 893 | 60 | -- |
| 4 | 28 | M | Neck | 17 | 1300 | 794 | 100 | Developed vitiligo in surrounding skin |
| 5 | 5 | F | Chest | 10 | 400 | 260 | 100 | -- |
| 6 | 21 | M | Trunk | 21 | 2500 | 1171 | 50 | -- |
| 7 | 12 | F | Face | 9 | 500 | 294 | 100 | -- |
| 8 | 19 | F | Lower extremity | 10 | 800 | 520 | 0 | -- |
| 9 | 37 | M | Back | 17 | 1000 | 735 | 100 | -- |
| 10 | 29 | F | Neck | 39 | 2800 | 1671 | 75 | -- |
| 11 | 9 | M | Lower extremity | 28 | 1100 | 539 | 90 | Developed vitiligo in surrounding skin |
| 12 | 11 | F | Neck | 12 | 800 | 566 | 100 | -- |
| 13 | 21 | F | Lower extremity | 30 | 2200 | 1313 | 90 | -- |
| 14 | 22 | F | Face | 32 | 2000 | 881 | 60 | -- |
| 15 | 15 | F | Trunk | 10 | 800 | 520 | 100 | -- |
| 16 | 38 | M | Chest | 20 | 1200 | 835 | 80 | -- |
| 17 | 29 | F | Face | 8 | 500 | 362 | 0 | Intense erythema and blistering |
| 18 | 21 | F | Neck | 20 | 900 | 695 | 100 | -- |
| 19 | 32 | F | Chest | 10 | 1000 | 550 | 100 | -- |
| 20 | 17 | M | Back | 12 | 800 | 566 | 70 | -- |
| 21 | 47 | F | Trunk | 11 | 900 | 563 | 100 | -- |
| 22 | 21 | F | Trunk | 26 | 1400 | 988 | 100 | -- |
| 23 | 12 | F | Face | 24 | 1100 | 841 | 100 | -- |
| 24 | 43 | F | Neck | 5 | 400 | 360 | 70 | -- |
| 25 | 8 | M | Upper extremity | 38 | 2400 | 1521 | 100 | -- |
| 26 | 29 | F | Back | 21 | 1500 | 919 | 100 | -- |
| 27 | 20 | F | Face | 16 | 1400 | 781 | 90 | -- |
| 28 | 21 | M | Lower extremity | 8 | 600 | 412 | 100 | -- |
| 29 | 40 | M | Neck | 26 | 2800 | 1288 | 70 | -- |
F = female, M = male
The percentage of repigmentation in different age groups and gender is shown in Tables 2 and 3, respectively. HN was distributed all over the body, 5 (17.2%) patients had it on the face, 6 (20.7%) on the neck, 4 (13.7%) each on the chest, trunk, and back, and 5 (17.2%) and 1 (3.4%) on the lower and upper extremities, respectively. The number of sessions to achieve satisfactory response ranged from 5 to 39 sessions, with an average number of sessions of 18.3. The frequency of repigmentation in different body sites is shown in Table 4. Maximum fluence ranged from 400 to 2800 mJ/cm2 to attain repigmentation. The average fluence used in the study ranged from 400 to 1671 mJ/cm2 with a mean fluence of 748 mJ/cm2.
| Crosstab | |||||||
|---|---|---|---|---|---|---|---|
| Repigmentation | Total | ||||||
| No pigmentation | Grade-3 (very good improvement) | Grade-4 (excellent improvement) | 100% (outstanding improvement) | ||||
| Age (years) (Binned) | ≤10 | Count | 0 | 1 | 1 | 2 | 4 |
| % within age (Binned) | 0.0% | 25.0% | 25.0% | 50.0% | 100.0% | ||
| 11–20 | Count | 1 | 1 | 2 | 4 | 8 | |
| % within age (Binned) | 12.5% | 12.5% | 25.0% | 50.0% | 100.0% | ||
| 21–30 | Count | 0 | 2 | 3 | 5 | 10 | |
| % within age (Binned) | 0.0% | 20.0% | 30.0% | 50.0% | 100.0% | ||
| 31–40 | Count | 1 | 2 | 0 | 1 | 4 | |
| % within age (Binned) | 25.0% | 50.0% | 0.0% | 25.0% | 100.0% | ||
| 41+ | Count | 0 | 1 | 0 | 2 | 3 | |
| % within age (Binned) | 0.0% | 33.3% | 0.0% | 66.7% | 100.0% | ||
| Total | Count | 2 | 7 | 6 | 14 | 29 | |
| % within age (Binned) | 6.9% | 24.1% | 20.7% | 48.3% | 100.0% | ||
| Repigmentation | Total | ||||||
|---|---|---|---|---|---|---|---|
| No repigmentation | Grade-3 (very good improvement) | Grade-4 (excellent improvement) | 100% (outstanding improvement) | ||||
| Gender | Male | Count | 0 | 4 | 1 | 5 | 10 |
| % within gender | 0.0% | 40.0% | 10.0% | 50.0% | 100.0% | ||
| Female | Count | 2 | 3 | 5 | 9 | 19 | |
| % within gender | 10.5% | 15.8% | 26.3% | 47.4% | 100.0% | ||
| Total | Count | 2 | 7 | 6 | 14 | 29 | |
| % within gender | 6.9% | 24.1% | 20.7% | 48.3% | 100.0% | ||
| Crosstab | |||||||
|---|---|---|---|---|---|---|---|
| Repigmentation | Total | ||||||
| No pigmentation | Grade-3 (very good improvement) | Grade-4 (excellent improvement) | 100% (Outstanding improvement) | ||||
| Site | Back | Count | 0 | 0 | 0 | 4 | 4 |
| % within site | 0.0% | 0.0% | 0.0% | 100.0% | 100.0% | ||
| Upper and lower extremities | Count | 1 | 2 | 2 | 1 | 6 | |
| % within site | 16.7% | 33.3% | 33.3% | 16.7% | 100.0% | ||
| Chest | Count | 1 | 2 | 0 | 1 | 4 | |
| % within site | 25.0% | 50.0% | 0.0% | 25.0% | 100.0% | ||
| Neck | Count | 0 | 1 | 2 | 3 | 6 | |
| % within site | 0.0% | 16.7% | 33.3% | 50.0% | 100.0% | ||
| Trunk | Count | 0 | 2 | 1 | 1 | 4 | |
| % within site | 0.0% | 50.0% | 25.0% | 25.0% | 100.0% | ||
| Face | Count | 0 | 0 | 1 | 4 | 5 | |
| % within site | 0.0% | 0.0% | 20.0% | 80.0% | 100.0% | ||
| Total | Count | 2 | 7 | 6 | 14 | 29 | |
| % within site | 6.9% | 24.1% | 20.7% | 48.3% | 100.0% | ||
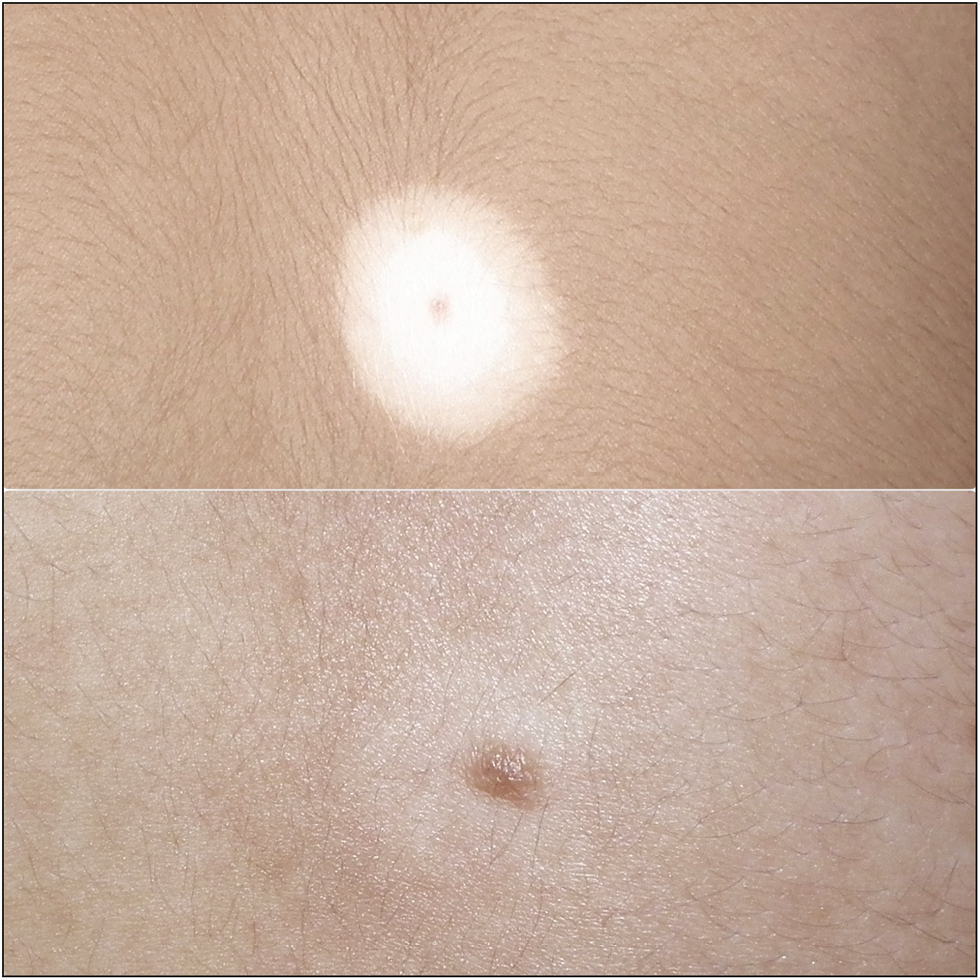
An outstanding response was noticed in 14 (48.2%) patients [Figures 1–4], whereas 6 (20.6%) patients showed excellent improvement [Figures 5 and 6]. Very good and partial improvement was observed in 6 (20.6%) patients and 1 (3.4%) patient, respectively [Figure 7]. Only 2 (6.8%) patients showed no response after 10 consecutive sessions and declared the treatment as failure. Dermoscopy showed diffuse structureless area at the periphery with reticular pigment network in the center. After treatment, it showed an increased amount of melanin in the nevus area and pockets of reticular pigment network in the white area [Figure 8]. The lesion on the face and neck responded fast, and lesions on the extremities took relatively long time to respond. But no statistically significant difference was observed between the lesion location and the outcome of the treatment by analysis of variance, which is shown in Table 5.

- Clinical image of halo nevus on the face showing outstanding improvement after MEL treatment

- Clinical image of halo nevus on the face showing outstanding improvement after MEL treatment

- Clinical image of halo nevus on the back showing outstanding improvement after MEL treatment

- Clinical image of halo nevus on the chest showing outstanding improvement after MEL treatment

- Clinical image of halo nevus on the thigh showing excellent improvement after MEL treatment
- Clinical image of halo nevus on the back showing outstanding improvement after MEL treatment

- Clinical image of halo nevus on the upper leg showing very good improvement after MEL treatment
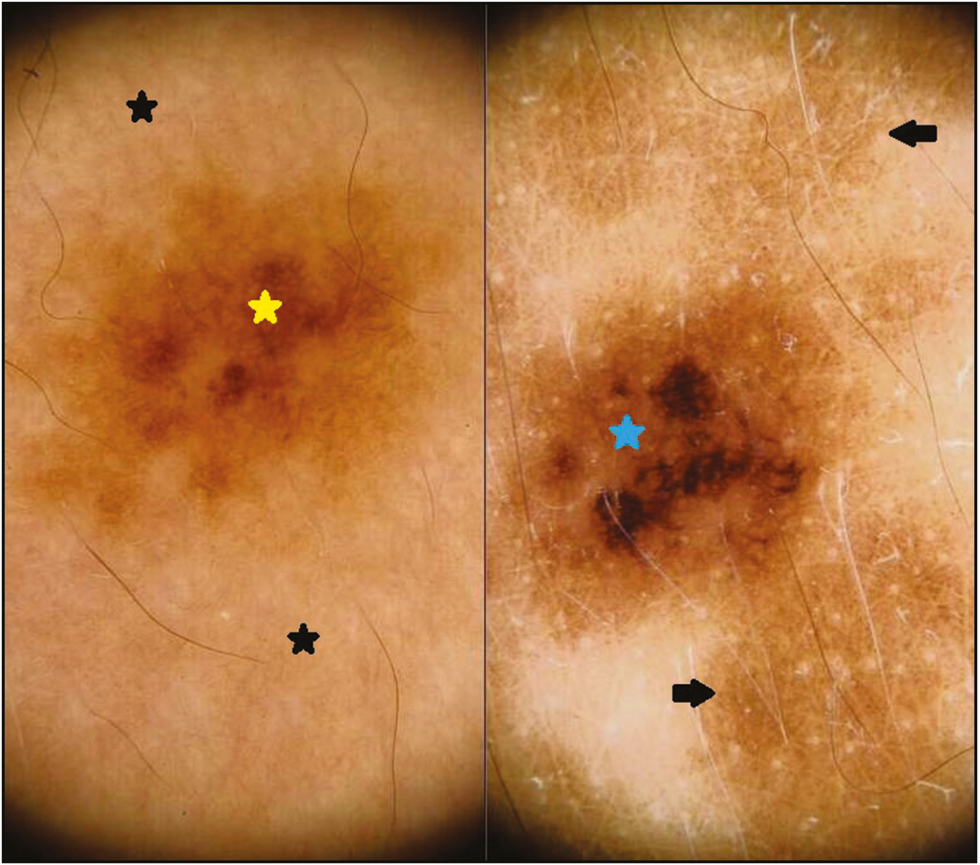
- (A) Dermoscopy of halo nevus showing pigment network (yellow star) in the center surrounded by diffuse structureless white areas (black stars) (left panel). (B) After treatment, faint pigment network (black arrows) is well appreciated in the white structureless area and also note the increased melanin amount in the pigment network (blue star) (right panel)
| Site | Number of sessions (mean ± SD) | Maximum dose [mJ/cm2] | Minimum dose [mJ/cm2] | Percentage of repigmentation (mean ± SD) |
|---|---|---|---|---|
| Face | 17.8±10.2 | 1100±636.3 | 631.8±280 | 98.0±4.4 |
| Neck | 19. 8±11.7 | 1500±1046.9 | 895±490 | 87.5±14 |
| Chest | 18.0±10.4 | 1200±748.3 | 634.5±291.2 | 55±41.2 |
| Trunk | 17.0±7,78 | 1400±778 | 810.5±319 | 77.5±22.1 |
| Back | 14.2±6.07 | 1000±355.9 | 619.2±218.2 | 100 |
| Extremities | 21.0±12.5 | 1350±758.2 | 821.6±192.1 | 68.3±35.4 |
SD = standard deviation
All patients tolerated the procedure well. Only one patient with HN on the chest developed intense erythema and blistering at the site, which resolved on its own. This particular lesion did not respond to treatment. Two patients developed vitiligo in the perilesional skin during the course of treatment but both of them responded to MEL with complete repigmentation. We did not contemplate perilesional hyperpigmentation as a complication rather it was considered as the normal outcome of treatment as the patients in this study were of skin type 4 and 5. However, it was minimized by using silicone stencils and interestingly, it resolved in all patients after discontinuation of MEL.
DISCUSSION
HN is found most commonly in children. The average age of onset is 15 years. In our study, it was 23 years. There is no predilection for sex or race.[2] In our study, female outnumbered male by 2:1 ratio. This can be attributed to greater awareness in the female subjects because of social stigma.
HNs can develop anywhere on the body but are seen most frequently on the trunk.[15] The neck is the most common site involved in our study followed by the face and lower extremity.
The treatment of HN is controversial. There are reports for spontaneous resolution of halo nevi with the disappearance of nevus and repigmentation of halo.[9] The appearance of halo represents the onset of nevus regression and disappearance of nevus leaving behind a depigmented halo. Eventually, the halo gets repigmented spontaneously.[1516] Aouthmany et al.[17] reported the average duration for complete resolution of the halo as 7.8 years. They also reported that 51% of HN showed no change after an average of 4.2 years, and 78% of HN failed to resolve during an average follow-up of 5.6 years.[17] Such a long duration for spontaneous resolution is unacceptable in our patients.
There are not many reports on the treatment of HN. Hossain[10] treated two cases of benign halo nevi with topical tacrolimus ointment. Wang et al.[11] treated HN by complete excision. They also reported repigmentation of associated vitiligo following excision. Excision of HN is not always possible because of the size and location. The resulting scar may be unacceptable to many of the patients, and the frequency of achieving the regression of depigmented halo after excision is lesser and sometimes it takes place after many years.[11]
Excimer lasers are sometimes called as “exciplex” lasers, which are pulsed gas lasers typically emitting ultraviolet light. The term “excimer” is used as the short form of “excited dimer.” It uses noble gas and halide molecules. The 308-nm MEL particularly uses xenon as a noble gas and chloride as a halide molecule.
MEL has a similar mechanism of action as that of a laser.[14] It emits monochromatic ultraviolet light of 308-nm wavelength, which unlike laser is non-collimated and noncoherent. It causes T cell apoptosis resulting in immunosuppression. It also results in DNA damage and stimulates melanocytic-stimulating hormone and melanocytic proliferation. These effects eventually bring in the repigmentation in the depigmented areas of vitiligo or HN.[1819] Localized vitiligo responded well with MEL in many studies and the most effective result was observed in the lesions on the face and neck.[11] Chimento et al.[20] in a pilot study treated 10 patients of stable vitiligo with ME and concluded that 308-nm MEL is a safe and effective therapeutic option in patients with stable vitiligo in skin types 3 to 6. Nisticò et al.[21] studied 53 patients of vitiligo and concluded that 308-nm MEL alone or in combination with 0.1% tacrolimus is effective in the treatment of vitiligo.
Mulekar et al.[12] treated four cases of HN on the face with an excimer laser. They reported 100% repigmentation in two cases and 80% repigmentation in the remaining two cases. They also reported retention of pigment at 18 months follow-up without any changes suggestive of melanoma.[12]
On the basis of this report and reports of successful treatment of vitiligo with MEL,[22] we decided to treat HN with MEL. In this study, patients with lesions affecting the facial and non-facial areas were selected. All patients showed improvement ranging from outstanding to good except two patients in whom no improvement was reported even after 10 consecutive sessions. No malignant changes were noticed in this study following MEL treatment. No statistically significant variation was reported in the treatment outcome based on the location of the lesion. However, lesions located on the face and neck responded faster as compared to that on the other areas. No studies are available to compare this entity in the literature. Nevertheless, in vitiligo, MEL produces better results in the facial and neck lesions as compared to lesions affecting other areas of the body.[23]
Association of melanoma with HN or development of melanoma following MEL treatment of HN is a great concern. There are reports to support the occurrence of melanoma after ablative lasers treatment.[24] A large systematic review by Eggen et al.[25] found no evidence of malignant transformation of congenital melanocytic nevus treated with lasers. In a doubtful case, dermoscopy or biopsy should be carried out to rule out melanoma. Having said this, it is also important to remember that incidence of melanoma in skin types 4, 5, and 6 is very low. A study by Weyant et al.[26] also confirmed that HN arise from a variety of histologic types of nevi, most of which are not dysplastic. Kolm et al.[27] examined 138 HN in 87 patients with dermoscopy and found that HN exhibits the characteristic dermoscopic feature of benign melanocytic nevi. Thus, we believe that MEL in HN is a good therapeutic option because repigmentation occurs with a rapidity, which is also cosmetically acceptable by the patients. In this study, repigmentation was satisfactory in most patients. Although no significant difference in the treatment outcome between the sites and size of HN was observed, lesions on the face and neck achieved faster repigmentation as compared to lesions present in other areas.
CONCLUSION
HN causes apprehension in the Indian population because of the social stigma associated with depigmented or hypopigmented patches on the body. Mere observation and carrying out simple follow-ups in treatment protocol are not sufficient. Hence HN should be treated. MEL is a noninvasive procedure, which results in excellent repigmentation of HN without scarring.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We are grateful to Dr. Manjula Kashinakunti, Associate Professor, Department of PSM, S. Nijalingappa Medical College and H. S. K. Hospital and Research Centre, Bagalkot, Karnataka, India, for her assistance in statistics.
REFERENCES
- An unusual variety of vitiligo (leucoderma acquisitum centrifugum) J Cutan Dis. 1916;34:797-800.
- [Google Scholar]
- Factors associated with development of vitiligo in patients with halo nevus. Chin Med J (Engl). 2017;130:2703-8.
- [Google Scholar]
- Prognostic value and clinical significance of halo naevi regarding vitiligo. Br J Dermatol. 2011;164:743-9.
- [Google Scholar]
- A comparative study of mitochondrial ultrastructure in melanocytes from perilesional vitiligo skin and perilesional halo nevi skin. Arch Dermatol Res. 2015;307:281-9.
- [Google Scholar]
- Differences in the melanosome distribution within the epidermal melanin units and its association with the impairing background of leukoderma in vitiligo and halo nevi: a retrospective study. Arch Dermatol Res. 2017;309:323-33.
- [Google Scholar]
- Melanocyte mutation in halo naevus and malignant melanoma? Br J Dermatol. 1979;100:423-6.
- [Google Scholar]
- Halo congenital nevus undergoing spontaneous regression. Involvement of T-cell immunity in involution and presence of circulating anti-nevus cell IgM antibodies. Arch Dermatol. 1994;130:1036-41.
- [Google Scholar]
- Treating benign halo nevus and focal vitiligo with topical tacrolimus: a brief report. Am J Clin and Exp Med. 2014;2:103-5.
- [Google Scholar]
- Resolution of vitiligo following excision of halo congenital melanocytic nevus: a rare case report. Dermatol Ther. 2016;29:145-7.
- [Google Scholar]
- Treatment of halo nevus with a 308-nm excimer laser: a pilot study. J Cosmet Laser Ther. 2007;9:245-8.
- [Google Scholar]
- 308-nm excimer lamp vs. 308-nm excimer laser for treating vitiligo: a randomized study. Br J Dermatol. 2010;163:188-92.
- [Google Scholar]
- Broad spectrum of leukoderma acquisitum centrifugum. Arch Dermatol. 1965;92:14-33. discussion 33-5
- [Google Scholar]
- Melanocytic tumors. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick’s dermatology in general medicine. New York: McGraw-Hill; 2008. p. :1105.
- [Google Scholar]
- The natural history of halo nevi: a retrospective case series. J Am Acad Dermatol. 2012;67:582-6.
- [Google Scholar]
- 308nm monochromatic excimer light in dermatology: personal experience and review of the literature. G Ital Dermatol Venereol. 2008;143:329-37.
- [Google Scholar]
- Efficacy of excimer light therapy for treatment of localized, progressive vitiligo. Our Dermatol Online. 2015;6:149-52.
- [Google Scholar]
- A pilot study to determine the safety and efficacy of monochromatic excimer light in the treatment of vitiligo. J Drugs Dermatol. 2008;7:258-63.
- [Google Scholar]
- Vitiligo treatment with monochromatic excimer light and tacrolimus: results of an open randomized controlled study. Photomed Laser Surg. 2012;30:26-30.
- [Google Scholar]
- Monochromatic excimer light 308nm in the treatment of vitiligo: a pilot study. J Eur Acad Dermatol Venereol. 2003;17:531-7.
- [Google Scholar]
- Rapid response of facial vitiligo to 308nm excimer laser and topical calcipotriene. J Clin Aesthet Dermatol. 2011;4:41-4.
- [Google Scholar]
- Malignant melanoma occurring at the periphery of a giant congenital naevus previously treated with laser therapy. Br J Dermatol. 2003;149:886-8.
- [Google Scholar]
- Laser treatment of congenital melanocytic naevi: a systematic review. Br J Dermatol. 2018;178:369-83.
- [Google Scholar]
- Halo nevus: review of the literature and clinicopathologic findings. Int J Dermatol. 2015;54:e433-5.
- [Google Scholar]





