Translate this page into:
Does the Optimal Layer of the Skin Include the Orbicularis Oculi Muscle When Elevating Cheek Rotation Flap?
Address for correspondence: Prof. Naohiro Ishii, Department of Plastic and Reconstructive Surgery, International University of Health and Welfare Hospital, 537-3, Iguchi, Nasushiobara City, Tochigi 329-2763, Japan. E-mail: ishinao0916@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
The cheek rotation flap is widely used as an optimal technique for lower eyelid reconstruction; however, the elevation layer of the skin including the orbicularis oculi muscle (OOM) remains unresolved.
Materials and Methods:
Between February 2006 and October 2012, 11 patients who underwent repair of partial-thickness defects of the lower eyelids using the cheek rotation flap were included in this prospective study. We investigated the influence of elevating the layer of skin including the OOM on the incidence of perioperative complications, operation time, long-term postoperative morphology, and function of the lower eyelid. The layer of flap elevation was deep to the OOM in four patients (deep to OOM cases) and superficial to the OOM in seven (superficial to OOM cases).
Results:
The superficial to OOM cases had a similar incidence of perioperative complications including flap congestion as the deep to OOM cases. However, the superficial to OOM cases required a significantly longer operation time. Furthermore, lid retraction was found in all of the deep to OOM cases and none of the superficial to OOM cases. In addition, the postoperative results in all the superficial to OOM cases showed satisfactory contours of the lower eyelid without revision surgery. However, many of the deep to OOM cases needed revision surgery to improve lid retraction.
Conclusion:
The cheek rotation flap should be elevated in superficial to the OOM cases because postoperative lid retraction occurred significantly more in the deep to OOM cases than in the superficial to OOM cases, although elaborate dissection may prolong the operation time.
Keywords
Cheek rotation flap
lower eyelid reconstruction
malar flap
orbicularis oculi muscle
Introduction
In lower eyelid reconstruction, a lid of adequate height with a stable edge should be formed, and the mucosa should not escape over the lid margin into the skin area. Furthermore, it is best to select an approach that does not interfere with the upper lid. The cheek rotation flap can fulfill these requirements; in addition, this flap is simple to design, and the skin color and texture are a good match for the normal lower lid skin. Therefore, it is widely used for partial or complete lower lid reconstruction.[12]
It is often stated that the cheek skin in this flap should be elevated in the face-lift plane so as not to injure the temporal branch of the facial nerve.[123] The skin covering the orbicularis oculi muscle (OOM) is generally thin, and therefore, elaborate dissection is needed to elevate this flap superficial to the OOM. In contrast, elevating this flap deep to the OOM can be easily performed with blunt dissection, but the effect of this technique on postoperative morphology and function of the lower eyelid is of concern. No significant data were reported to date concerning whether skin dissection should be performed superficial to or deep to the OOM when elevating this flap.
This investigation is a descriptive, prospective study and aims to analyze the influence of the skin elevation layer—superficial to or deep to the OOM—on long-term postoperative morphology and function of the lower eyelid and the incidence of perioperative complications in lower eyelid reconstruction using the cheek rotation flap.
Materials and Methods
Patients
Eleven patients with a malignant tumor of the lower eyelid who underwent wide resection, preserving the tarsus and palpebral conjunctiva, and reconstruction, using the cheek rotation flap, between February 2006 and October 2012, were included in this study. The patients consisted of 5 men and 6 women; age ranged from 56 to 85 years, with a mean age of 71.0 years. There were nine cases of basal cell carcinoma and two cases of squamous cell carcinoma. The central location of the defect was classified into four cases as the medial lower eyelid, five cases as the median lower eyelid, and two cases as the lateral lower eyelid. The layer of flap elevation was deep to the OOM in four patients in the first half of the study period (between February 2006 and February 2010) and superficial to the OOM in seven patients in the last half of the study period (between March 2010 and October 2012). Operation time ranged from 58 to 191min. Table 1 summarizes patients’ characteristics. All patients provided written informed consent for the publication of this article and the use of their images.
| Case | Age (years) | Tumor type/location | Defect dimension (height × width, cm) | Flap dimension (height × width, cm) | Layer of flap elevation | Operation time (min) |
|---|---|---|---|---|---|---|
| 1 | 60 | BCC/median | 4.5×3.0 | 8.0×10.0 | Deep to OOM | 119 |
| 2 | 85 | BCC/medial | 4.2×2.5 | 5.8×8.0 | Deep to OOM | 85 |
| 3 | 70 | BCC/median | 4.5×2.0 | 8.0×8.5 | Deep to OOM | 100 |
| 4 | 63 | SCC/median | 4.5×2.8 | 8.0×9.5 | Deep to OOM | 115 |
| 5 | 72 | BCC/lateral | 3.0×1.5 | 4.5×6.0 | Superficial to OOM | 79 |
| 6 | 56 | BCC/lateral | 2.5×1.5 | 3.5×5.5 | Superficial to OOM | 58 |
| 7 | 81 | BCC/median | 4.8×2.2 | 6.0×10.0 | Superficial to OOM | 105 |
| 8 | 78 | SCC/medial | 6.0×2.5 | 8.5×12.0 | Superficial to OOM | 154 |
| 9 | 73 | BCC/median | 6.5×3.5 | 9.2×11.0 | Superficial to OOM | 191 |
| 10 | 73 | BCC/medial | 3.2×2.5 | 5.4×10.5 | Superficial to OOM | 120 |
| 11 | 70 | BCC/medial | 6.5×3.3 | 9.0×10.0 | Superficial to OOM | 160 |
BCC, basal cell carcinoma; SCC, squamous cell carcinoma
Surgical procedure
Wide resection of the malignant tumor, including dog ear at the inferior site, was performed, preserving the tarsus and palpebral conjunctiva. The cheek rotation flap was prepared to be placed along the lateral edge of the lower eyelid up to the lateral canthus, and then run in a large concave arc from the lateral canthus to the preauricular lesion, with the length determined on the basis of defect size and skin tension [Figure 1A and B].

- Flow of the surgical procedure. The flap design was drawn in a large concave arc from the lateral canthus to the preauricular lesion. (A) Deep to OOM cases. (B) Superficial to OOM cases. The flap was elevated superficial to the OOM with elaborate dissection or deep to the OOM with blunt dissection at the lower eyelid and in the face-lift plane at sites other than the lower eyelid. (C) Deep to OOM cases. (D) Superficial to OOM cases. The flap was pulled forward and rotated medially onto the defect with anchoring to the periosteum and soft tissue over the zygoma. (E) Deep to OOM cases. (F) Superficial to OOM cases
The flap was elevated from medial to lateral deep to or superficial to the OOM at the lower eyelid and in the face-lift plane at locations other than the lower eyelid, following careful hemostasis [Figure 1C and D]. The zygomatic cutaneous ligament was preserved.
The flap was pulled forward and rotated medially onto the defect with minimal tension as much as possible. The undersurface of the flap was anchored to the periosteum and soft tissue over the zygoma with nonabsorbable sutures, as anchoring can prevent ptosis of the flap and subsequent ectropion.
Excess skin at the base of the vertical cheek suture line was trimmed, and the surrounding skin was undermined as required. A closed suction drain was inserted underneath the flap to prevent hematoma, and then the skin suture was performed [Figure 1E and F]. Revision surgery was performed for the patients with severe ectropion from postoperative 6 months to postoperative 1 year.
All the procedures were performed under general anesthesia by the first author or an operator supervised by him.
Postoperative assessment
Perioperative complications were recorded. The follow-up period was 5 years in all cases. We evaluated the degree of postoperative lagophthalmos and lid retraction during follow-up. We also evaluated them just before revision surgery in cases requiring revision. The degree of lid retraction was evaluated by the increase in affected fissure height (IFH) between the preoperative period and postoperative period (0 ≤ IFH < 2 (–)/2 ≤ IFH < 4 (+)/4 ≤ IFH (++), unit: mm). We used the Fisher’s exact test to compare the incidence of perioperative complications, postoperative lagophthalmos, and lid retraction in the patients treated with the layer of flap elevation deep to the OOM (deep to OOM cases) versus superficial to the OOM (superficial to OOM cases).
We investigated the correlation between the product of flap dimensions and operation time in both the groups. Furthermore, we used Student’s t-test to compare the average operation time per unit for the product of flap dimensions in both the groups.
Data were analyzed using the software Statistical Package for the Social Sciences (SPSS) version 23 for Windows (IBM Corporation, Chicago, Illinois). For all statistical tests, a P value of <0.05 was considered significant. The protocol for this study was approved by the institutional review board, and all the authors adhered to the strengthening the reporting of observational studies in epidemiology guidelines.
Results
During the follow-up period, no tumor recurrence was found in any of the patients. Table 2 shows the perioperative and postoperative results. Regarding perioperative complications, no cases of wound infection or seroma were identified. Hematoma was diagnosed in one patient among the superficial to OOM cases. Flap congestion was diagnosed in three of four deep to OOM cases and four of seven superficial to OOM cases. No significant differences in the incidence of hematoma or flap congestion were found between groups (P = 1.00 and 1.00, respectively). Debridement and resuturing were performed because of severe flap congestion in one of the deep to OOM cases. No cases of lagophthalmos were identified. In addition, lid retraction was found in all of the deep to OOM cases and in none of the superficial to OOM cases; a significant difference in the incidence of lid retraction was found between groups (P < 0.05). Severe lid retraction was improved by revision surgery, which included graft surgery for the patients with too severe lid retraction. The postoperative results of all superficial to OOM cases showed satisfactory contours of the rim of the lower eyelid and cheek without any requirement for revision surgery. Typical cases are shown in Figures 2–4.
| Case | Hematoma | Flap congestion* | Lagophthalmos | Lid retraction** | Revision surgery |
|---|---|---|---|---|---|
| 1 | – | ++ | – | + | Debridement, resuture |
| 2 | – | – | – | ++ → + | Ear cartilage graft |
| 3 | – | + | – | ++ → + | Kuhnt–Szymanowski method |
| 4 | – | + | – | ++ → + | Tensor fascia graft |
| 5 | – | – | – | – | – |
| 6 | – | – | – | – | – |
| 7 | – | – | – | – | – |
| 8 | – | + | – | – | – |
| 9 | + | + | – | – | – |
| 10 | – | + | – | – | – |
| 11 | – | + | – | – | – |
*moderate (+), severe (++), no occurrence (–)
**increase in fissure height (IFH, mm), 0 ≤ IFH < 2 (–)/2 ≤ IFH < 4 (+)/4 ≤ IFH (++)
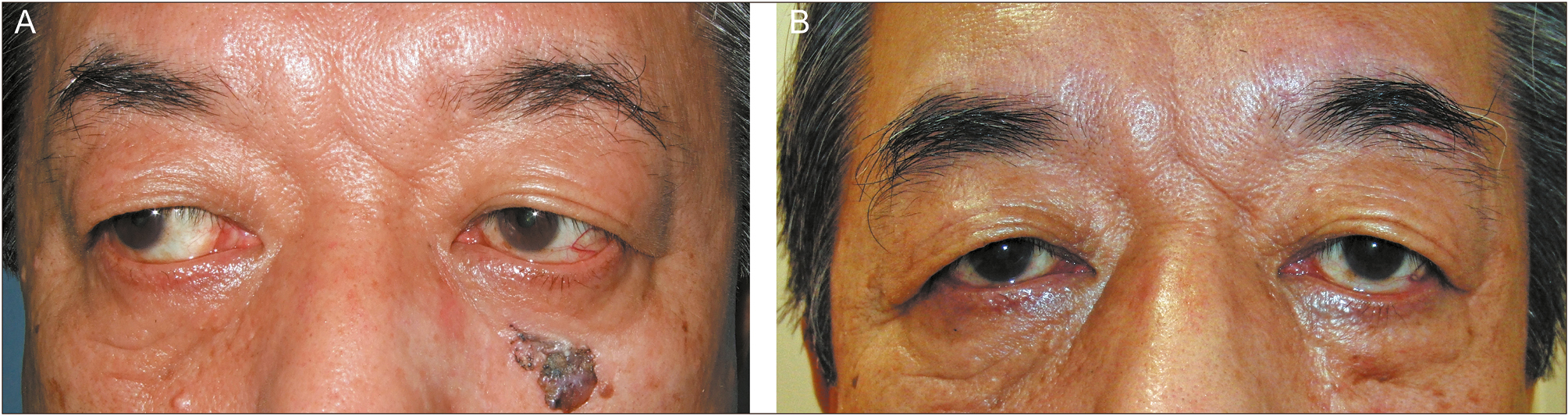
- Case 1: The flap was elevated deep to the OOM, and thereafter, debridement with resuturing was needed as revision surgery because of severe flap congestion.
- (A) Preoperative photograph. (B) Five years postoperative photograph; moderate lid retraction (IFH = 2) was found
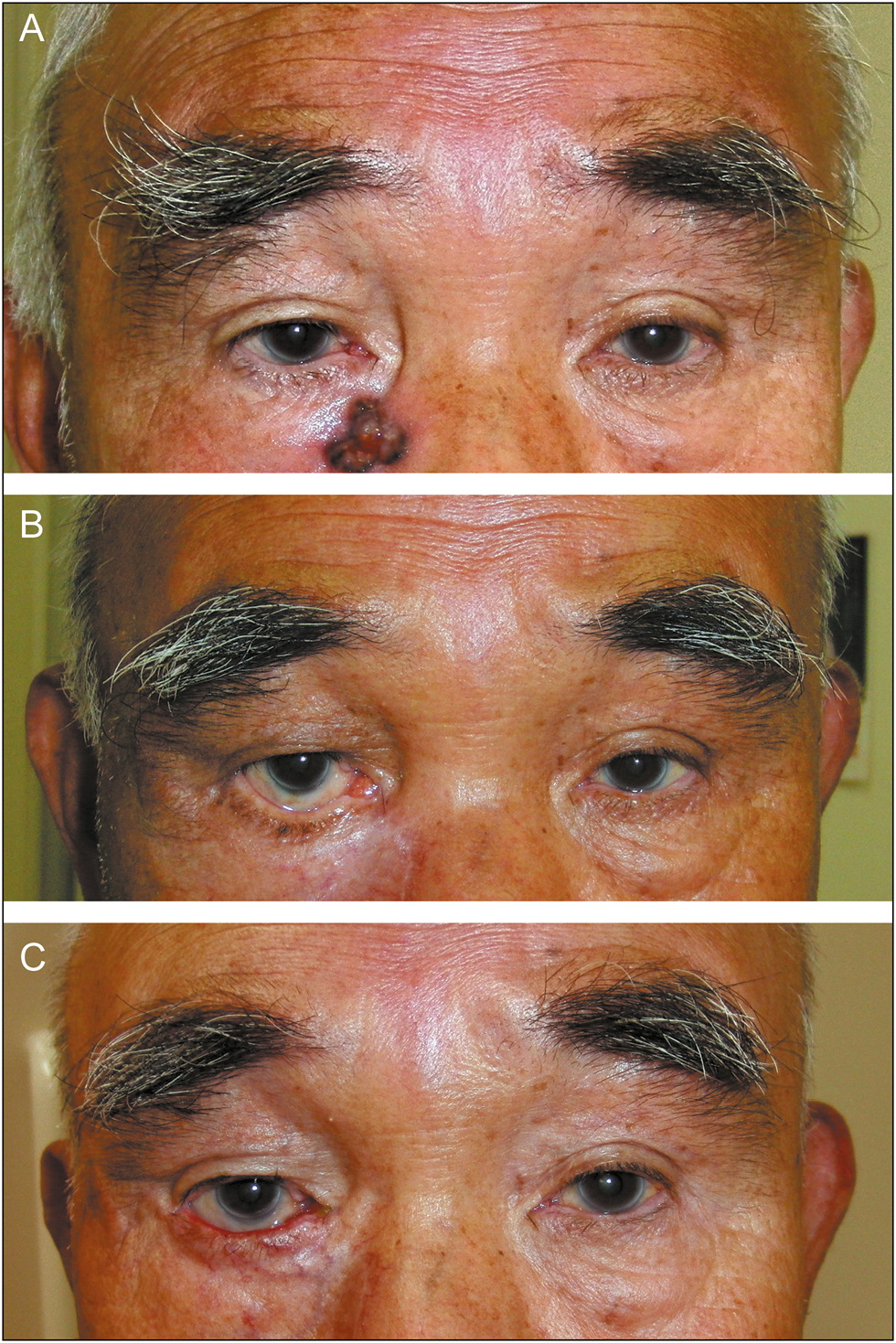
- Case 2: The flap was elevated deep to the OOM, and thereafter, ear cartilage graft was required as revision surgery because of severe lid retraction.
- (A) Preoperative photograph. (B) Seven months postoperative photograph; severe lid retraction (IFH = 4.5) was found. (C) Five years postoperative photograph; lid retraction (IFH = 2) improved to moderate after revision surgery
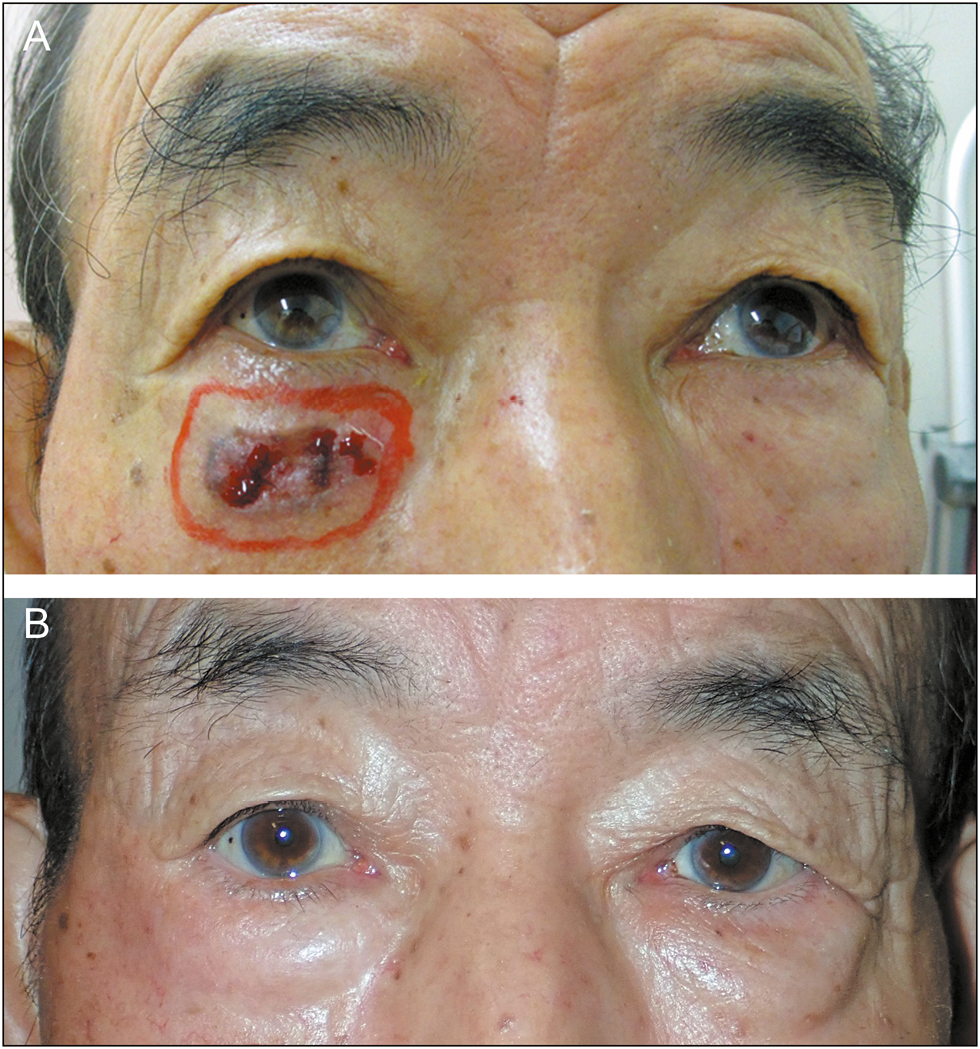
- Case 9: The flap was elevated superficial to the OOM, and thereafter, satisfactory contours of the rim of the lower eyelid and cheek were achieved without revision surgery.
- (A) Preoperative photograph. (B) Five years postoperative photograph; no lid retraction (IFH=0) was found
Significant correlation was found between the product of flap dimensions and operation time in the deep to OOM cases (R = 0.962, P < 0.05) and in the superficial to OOM cases (R = 0.975, P < 0.05) [Figure 5]. Furthermore, the average operation time per unit for the product of flap dimensions in the deep to OOM cases was 1.58min/cm2; for the superficial to OOM cases, the average operation time per unit was 2.14min/cm2. Thus, the average operation time per unit was significantly less in the deep to OOM group (P < 0.05).
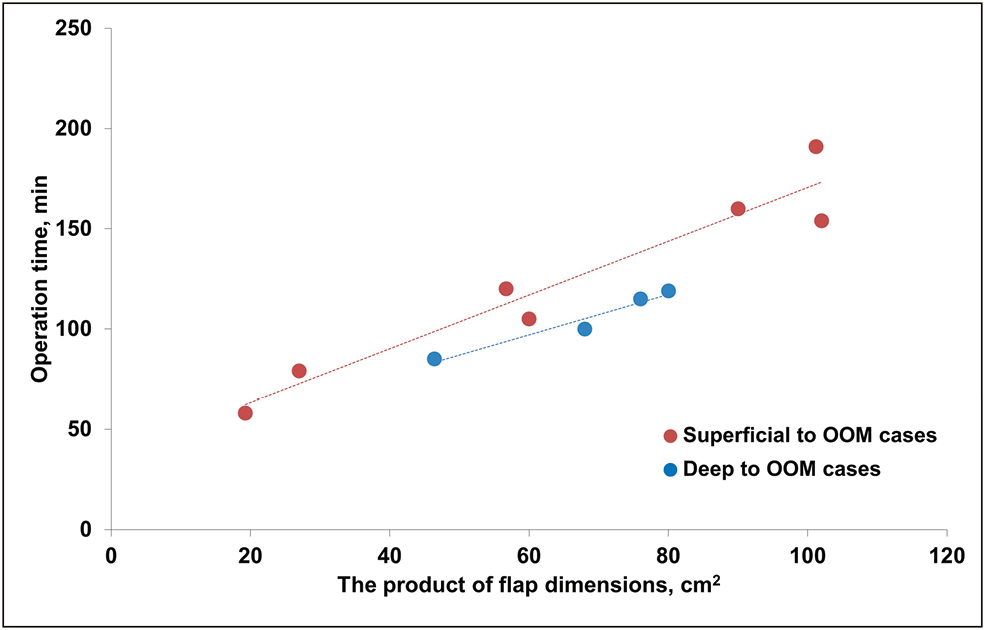
- Scatter plot and simple linear regression of the product of flap dimensions and operation time in deep to OOM cases and superficial to OOM cases. Deep to OOM cases, patients in whom the layer of flap elevation was deep to the OOM; superficial to OOM cases, patients in whom the layer of flap elevation was superficial to the OOM
Discussion
Several methods can be employed for lower eyelid reconstruction, including techniques using the upper lid, the forehead skin, the nasolabial skin, or the skin over the cheek area as a rotational flap.[124] However, forehead and nasolabial skin is thicker and its color is lighter; moreover, contour and function of the upper lid should be preserved as much as possible. The cheek rotational flap is a technique that can achieve good aesthetic and functional results using adjacent skin and reconstructing a large defect of the lower eyelid, including the medial canthus and nasal sidewall defect[1256]; therefore, it is widely considered to be the optimal choice. For full-thickness lower eyelid reconstruction, it can be combined with chondromucosal graft, fascia lata graft, and split-thickness palatal mucosal graft to create separate lining tissue.[278] The modified cheek rotation flap was also reported as a rotation–advancement tarsoconjunctival flap and combined flap with Z-plasties.[910]
In designing and elevating this flap, several pitfalls have been reported in the literature. To achieve sufficient height of the lid, preventing its postoperative retraction and reducing tension of the medial suture line, the incision line should be drawn in a large concave arc from the lateral canthus to the preauricular lesion and should be extended to the neck, with the length determined on the basis of the defect size and skin tension.[12] In addition, the pedicle of this flap should be inferior-based rather than lateral-based to prevent postoperative lid retraction.[11] Postoperative anthropometric measurements of this flap showed that poor design can cause a significantly increased risk of lower lid distortion, and therefore careful design must be performed to apply techniques that prevent lower lid retraction.[12] To prevent cheek sagging and ectropion, suturing the undersurface of the flap to the malar periosteum is strongly recommended.[12] Regarding the layer of elevation of this flap, earlier studies have shown that the cheek skin should be elevated in the face-lift plane so as to avoid injury to the temporal branch of the facial nerve[123]; however, whether the layer of skin should include the OOM remains unresolved.
This study investigated the influence of elevating the skin with or without the OOM on long-term postoperative morphology and function of the lower eyelid and the incidence of perioperative complications in lower eyelid reconstruction using the cheek rotation flap.
Results show that the superficial to OOM and deep to OOM cases had similar incidences of perioperative complications, including flap congestion. The superficial to OOM cases required significantly longer operation time because elevating the flap superficial to the OOM requires elaborate dissection. Lid retraction was found in all of the deep to OOM cases and in none of the superficial to OOM cases, representing a significant difference. In addition, the postoperative results in all of the superficial to OOM cases showed satisfactory contours of the rim of the lower eyelid and cheek without the need for revision surgery. In contrast, many deep to OOM cases needed revision surgery to improve lid retraction. On the basis of these results, we recommend that the elevation layer of the skin including OOM should be superficial to the OOM.
Limitations and Further Study
This study is limited by the small sample size. Therefore, our study may not be generalizable to the general population. However, it may demonstrate useful findings regarding the effect of the skin elevation layer and its association with the OOM when performing the cheek rotation flap. A further study with a larger sample size is being considered to evaluate these findings, including full-thickness lower eyelid reconstruction.
Conclusion
The elevation layer of the cheek rotation flap should be superficial to the OOM because postoperative lid retraction is significantly more common in cases treated with deep to OOM elevation. In addition, the incidence of perioperative complications including flap congestion was not affected by the elevation layer about OOM. However, complex dissection may prolong the operation time when performing superficial to OOM dissection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cheek rotation skin flap of the lower eyelid. In: Grabb’s encyclopedia of flaps (2nd ed). Philadelphia, PA: Lippincott-Raven; 1998. p. :56-60.
- [Google Scholar]
- Local flaps in head and neck reconstruction (2nd ed). St. Louis, MO: Quality Medical Publishing; 2007. p. :365-77.
- Complications following the use of a cheek flap rotation to reconstruct the lower lid. Ophthalmic Surg. 1975;6:42-3.
- [Google Scholar]
- Surgical management of lower-lid basal cell carcinoma involving the medial canthus: a modification of the Mustarde cheek rotation flap. Ophthalmic Plast Reconstr Surg. 1998;14:367-9.
- [Google Scholar]
- Lower eyelid reconstruction with a cheek flap supported by fascia lata. Plast Reconstr Surg. 1999;103:1650-4.
- [Google Scholar]
- Full-thickness reconstruction of the eyelid with rotation flap based on orbicularis oculi muscle and palatal mucosal graft: long-term results in 12 cases. J Plast Reconstr Aesthet Surg. 2009;62:1389-94.
- [Google Scholar]
- Reconstruction of the lower eye lid with a rotation-advancement tarsoconjunctival cheek flap. J Craniofac Surg. 2010;21:1786-9.
- [Google Scholar]
- Reconstruction of skin defects in the medial cheek using lateral cheek rotation flap combined with Z-plasties. J Plast Reconstr Aesthet Surg. 2015;68:e183-8.
- [Google Scholar]
- An inferiorly based rotation flap for defects involving the lower eyelid and medial cheek. Facial Plast Surg. 2015;31:411-6.
- [Google Scholar]
- Cheek rotation flap reconstruction—an anthropometric appraisal of surgical outcomes. Clin Oral Investig. 2014;18:1251-7.
- [Google Scholar]






