Translate this page into:
Mastoplasty after Massive Weight Loss: Redefinition and Stabilization of the Breast Mound with Submuscular Autoprosthesis
Address for correspondence: Dr. Verdiana Di Pietro, Via Aldo Moro, 7, 67100 L’Aquila (AQ), Italy. E-mail: verdiana.di.pietro@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
After massive weight loss, breast changes dramatically becoming ptotic, flat in the upper pole, with significant skin excess. After mastoplasty, often ptosis can recur and the upper pole can lose its fullness again. The technique described in this study treats breast deformities ensuring stable results and avoiding ptosis recurrence.
Aim:
To analyze a new modality of breast reshaping after massive weight loss, evaluating outcomes and complications as well as patient satisfaction.
Settings and Design:
This was a case series.
Materials and Methods:
Fifteen patients (all women, average age, 43.1 years) with bilateral breast ptosis after massive weight loss underwent mastoplasty: the technique included the creation of an inferior pedicle flap that was placed as a prosthesis under the pectoralis muscle and a superomedial pedicle flap containing the nipple–areola complex (NAC). Patients were followed up for at least 6 months, reporting any complications, and measuring the jugulum–NAC distance. Patients’ satisfaction was also reported.
Statistical Analysis Used:
Nil.
Results:
All patients were extremely satisfied with the breast volume, shape, symmetry, and ptosis correction. The new mammary contour and the distance between the jugular fossa and the nipple were stable during the follow-up and the upper pole maintained its fullness. No major complications were reported.
Conclusion:
Mastoplasty with submuscular autoprosthesis proved to be a safe and effective technique to treat breast deformities after massive weight loss because removed redundant tissue repositioned the NAC and filled the upper pole with stable results over time. A similar technique has not been described yet.
Keywords
Autoprosthesis
breast reshaping
inferior pedicle flap
massive weight loss
mastopexy
submuscular pocket
Introduction
After massive weight loss, people complain about redundant skin, body deformation, and ptosis of tissues. Breast is very important for a woman’s appearance; therefore, it is one of the body area that patients want to improve first. The main problems of the breast after weight loss concern the following:
-
-
Redundant, inelastic, and poor-quality skin because of the reduced content of elastin[1]
-
-
Ptosis of the nipple–areola complex (NAC) that is often medially rotated
-
-
-
-
Volume that can still be excessive despite slimming or greatly reduced
For this reason, in patients after massive weight loss, breast reshaping includes the following:
-
-
Removal of excess skin
-
-
Lifting and lateralization of the NAC
-
-
Restoration of the fullness of the upper pole and medialization of the breasts
-
-
Restoration of breast volume and symmetry
There are several systems of classification of breast ptosis.[456] According to the Pittsburgh Rating Scale (PRS), there are three types of breast deformities: (1) those with moderate ptosis, adequate breast parenchyma, and no skin laxity; (2) those with more significant ptosis and the NAC located 2–4cm below the inframammary fold (IMF), skin laxity, some breast parenchyma, and no marked medial deviation of the NAC; and (3) those with the most severe deformities with significant ptosis, extreme skin laxity, reduced breast parenchyma, and medial displacement of the NAC. These breast deformities represent a major challenge for surgeons because often ptosis recurs and the upper pole loses its fullness. We propose a new technique of mammaplasty for the redefinition and stabilization of the breast mound based on an inferior pedicle flap of autoprosthesis placed under the pectoralis major muscle.
Materials and Methods
Between January 2015 and September 2017, 15 women aged between 33 and 60 years (mean age, 46.4 years) underwent mastoplasty with submuscular autoprosthesis. Inclusion criteria were as follows:
-
-
Patients with massive weight loss after bariatric surgery with moderate/severe breast ptosis (type 2/3 in the PRS)
-
-
Patients who are young and healthy
-
-
Patients with body mass index (BMI) and weight stable for at least 6 months
-
-
Patients with a valid nutritional status (absence of severe protein, vitamins, minerals, or trace elements deficiencies)
-
-
Patients who underwent bariatric surgery at least 1 year before and patients who underwent any other plastic surgery at least 3 months before
The exclusion criteria were as follows:
-
-
Severe comorbidities (severe cardiac failure, severe metabolic or hemostatic imbalance, cirrhosis, and renal failure)
-
-
Unstable weight
-
-
Active breast disease (infections or cancer)
-
-
Severe mammary hypertrophy (quantity of breast tissue to be removed >800g) or severe ptosis (jugulum–NAC distance >33cm, ptosis of the NAC >12cm)
-
-
Breast ptosis with insufficient parenchyma
Preoperative data included the age at the time of surgery, amount of weight lost, BMI at the time of surgery, maximum BMI, and BMI variation. Surgical data included the duration of the intervention, amount of tissue removed, time for drainage removal, and length of hospital stay. The patients were followed for at least 6 months reporting:
-
-
Jugulum–NAC distance.
-
-
Incidence of major complications (bleeding, thromboembolism, and sepsis) and minor complications (hematoma, seroma, infection, wound dehiscence, nipple or skin necrosis, and nipple sensitivity disorders).
-
-
Patient satisfaction assessed by a six-point Likert scale (extremely satisfied, very satisfied, somewhat satisfied, somewhat dissatisfied, very dissatisfied, extremely dissatisfied). The parameters evaluated were breast volume, shape, symmetry, ptosis correction, and quality of scars.
Surgical Technique
The patient is marked on the day of surgery. With the patient in the standing position, the midline, midclavicular line and the inframammary fold are traced. The ideal position of the NAC is located on the breast meridian using the midpoint of the humerus or the anterior projection of the inframammary fold as a reference. The Wise pattern is placed two centimeters above this point and the areolar and the lateral and medial limbs of the pattern are marked. Then with the patient supine, we identify the skin excess to be removed between the pattern’s lower extremities and the inframammary fold by bimanual manoeuvre and we draw it. The final appearance of the markings are shown in [Figure 1]. The operation is conducted under general anesthesia and orotracheal intubation. The patient is in a supine position with the arms abducted at 90degrees and positioned on appropriate supports. We perform an antibiotic prophylaxis with 2g of cefazolin or 600mg of clindamycin in case of allergy, given 30–60min before the surgical incision. The patient wears antithrombotic stockings or elastic wraps throughout the duration of the surgery as a preventive measure from thromboembolic risk. We take great care to ensure that the patient’s body temperature remains adequate avoiding a too low temperature in the operating room, covering the patient with blankets, using a heated bed, and heating the infusion fluids. The incisions are made following the preoperative design according to Planas-Pitanguy technique.[7] The skin around the NAC is de-epithelialized. The incisions are deepened along the lateral pillars up to the pectoralis major muscle. An inferior pedicle flap is delimited tangent to the lower margin of the NAC with a width between 4 and 5cm as proposed by Ribeiro.[8] This flap is detached from the pectoralis muscle and de-epithelialized. Excess adipose and glandular tissues are removed [Figure 2A]. The pocket for the flap is created under the pectoralis major muscle after detachment of its lower rib insertions [Figure 2B]. The flap is placed under the muscle at a height that gives the proper projection to the breast mound [Figure 2C]. We generally place the flap quite high to prevent secondary ptosis and to fill the upper pole. Furthermore, to give more projection to the breast, we vertically incise the muscle on its back side. The inferior edge of the pectoralis muscle is anchored to the lower rib insertions using PDS-II 0, ©Ethicon US, LLC (polydioxanone) sutures [Figure 2D]. The superomedial flap containing the NAC is transposed and anchored in the proper position with 4-0 Monocryl, ©Ethicon US, LLC (poliglecaprone 25) stitches. The medial and lateral pillars are sutured together and anchored to the middle portion of the IMF with 3-0 Vicryl stitches ©Ethicon US, LLC (polyglactin 910) [Figure 2E]. Two laminar drains are placed inside the subpectoral pocket and other two drains are inserted in the retroglandular space. The areolas are sutured with Gillies stitches in 4-0 Monocryl. The vertical and the inframammary line sutures are completed with intradermal suture in 3-0 Monocryl [Figure 2F]. Petrolatum gauzes are placed on the NACs and adhesive skin closures are used to provide wound support. A compressive dressing is carried out.
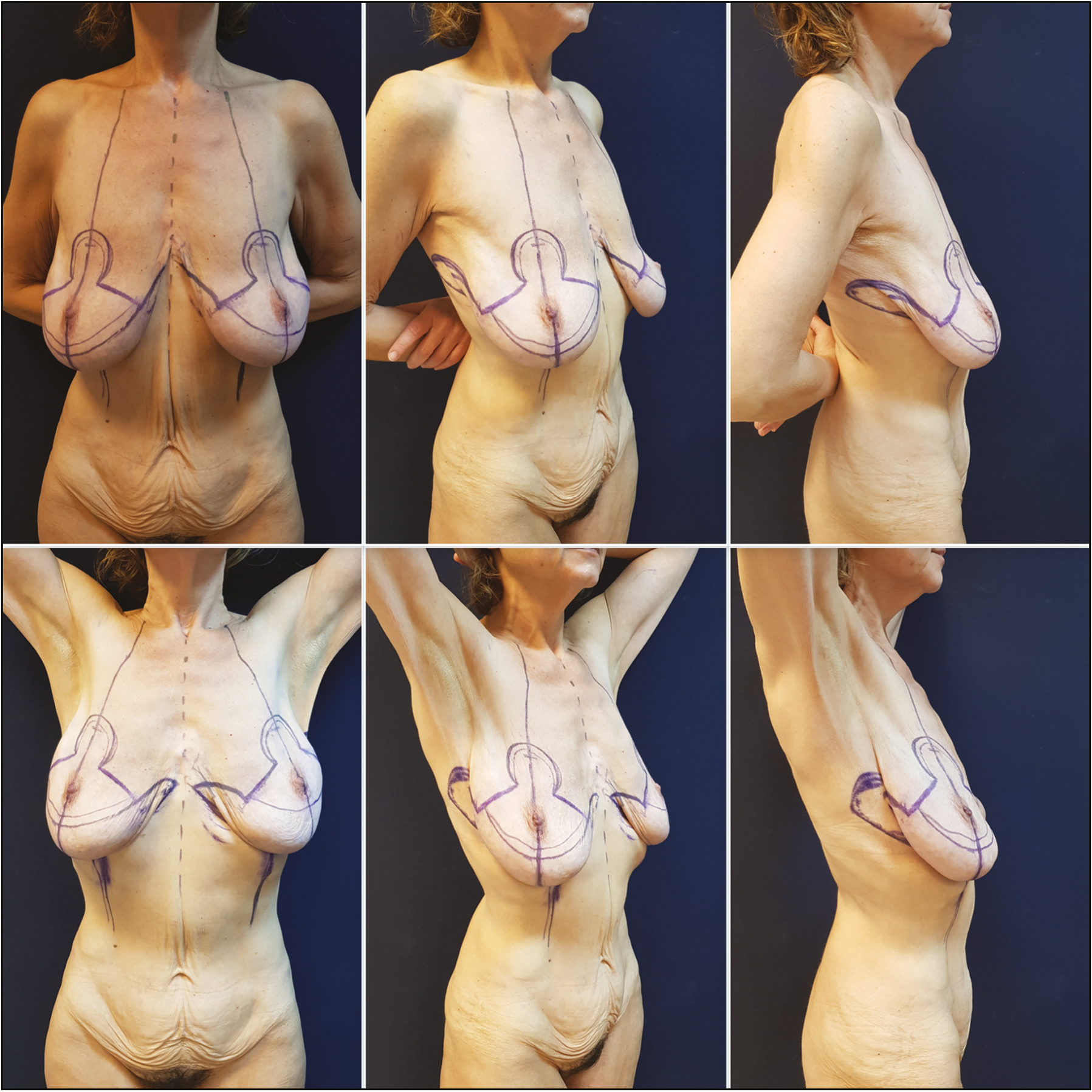
- Preoperative markings according to inverted-T mastoplasty
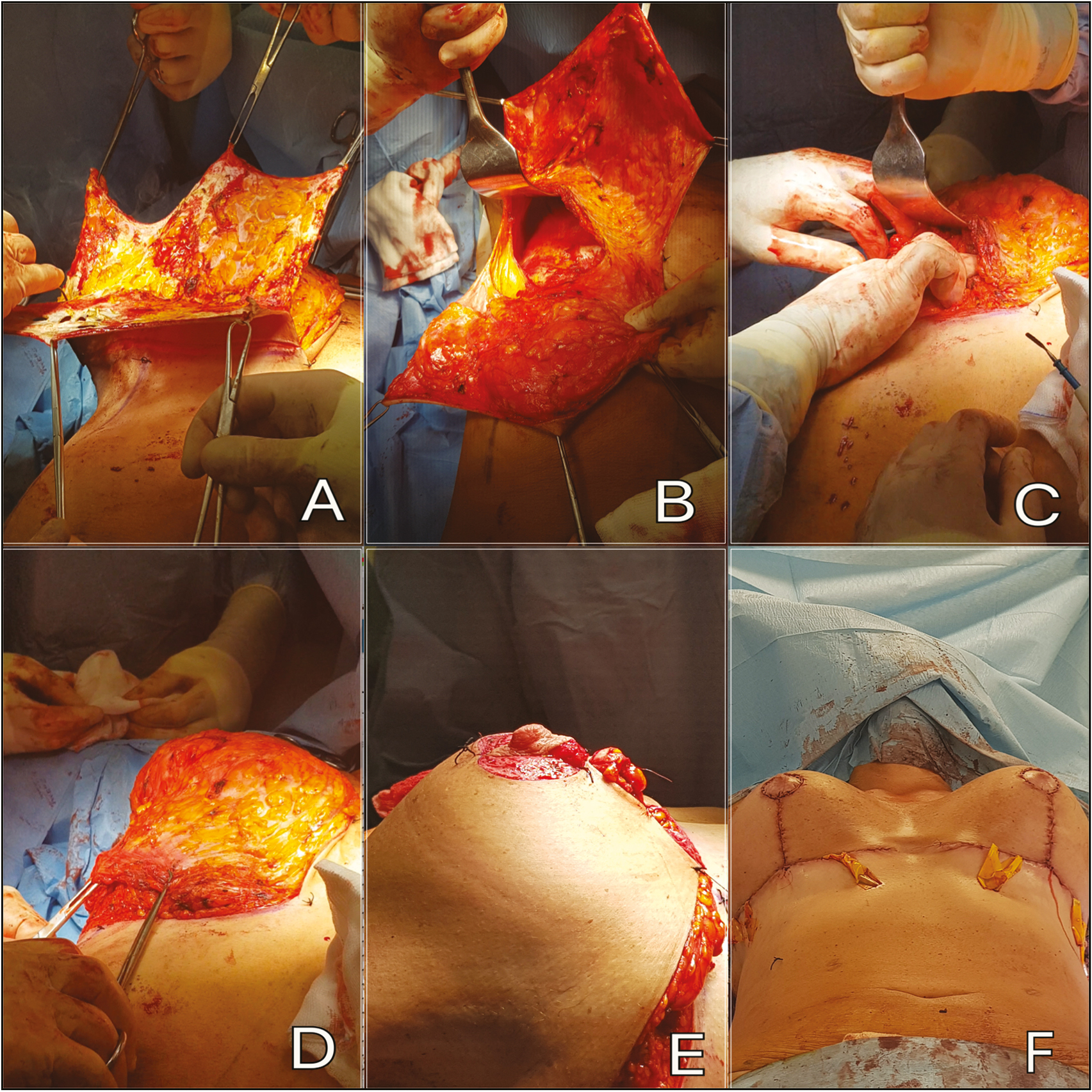
- Intraoperative pictures. (A) The flap is de-epithelialized. (B) Pectoralis muscle is detached from the lower ribs insertions. (C) The flap is inserted under the muscle. (D) The pocket is closed. (E) NAC projection is checked after submuscular flap positioning. (F) Final view
Results
All patients treated were women with a mean age at the time of surgery of 43.1 years (range, 22–66 years). The mean weight loss was 57.2 kg (range, 32.6–93 kg), the mean body weight of the patients at the time of surgery was 73 kg (range, 57–95 kg) with a mean BMI of 26.6kg/m2 (range, 20.9–34.4kg/m2), the mean maximum BMI was 49kg/m2 (range, 39–58kg/m2), and the mean delta-BMI was 21kg/m2 (range, 13.9–34kg/m2); in all patients, the weight loss was obtained with bariatric surgery and eight of them were smokers [Table 1].
| Demographic variables | Overall |
|---|---|
| No. of patients | 15 |
| Age at surgery (year) | 43.1 (min, 22; max, 66) |
| Mean weight loss (kg) | 57.2 (min, 32.6; max, 93) |
| Weight at surgery (kg) | 73 (min, 57; max, 95) |
| BMI at surgery (kg/m2) | 26.6 (min, 20.9; max, 34.4) |
| Maximum BMI (kg/m2) | 49 (min, 39; max, 58) |
| Change in BMI (kg/m2) | 21 (min, 13.9; max, 34) |
| Smokers | 8 |
BMI = body mass index, min = minimum, max = maximum
The mean duration of the intervention was 208.7min (range, 175–250min), the mean hospital stay was 2.3 days (range, 2–3 days), and the time to drain removal was 1.9 days (range, 1–3 days). The mean amount of tissue removed was 638.7g (range, 300–1200g). The minimum follow-up time was 6 months [Table 2].
| Surgical variables | Overall |
|---|---|
| No. of patients | 15 |
| Surgery duration (minutes) | 208.7 (min, 175; max, 250) |
| Resection weight (g) | 638.7 (min, 300; max, 1200) |
| Time to drain removal (days) | 1.9 (min, 1; max, 3) |
| Hospital stay (days) | 2.3 (min, 2; max, 3) |
Min = minimum, max = maximum
The mean jugulum–NAC distance before surgery was 33.9cm (range, 28–40cm), whereas after surgery was 23.7cm (range, 23–25cm); at 6 months, the mean jugulum–NAC distance was 24.6cm (range, 23–26cm), with an average variation of 0.8 (range, 0–2cm). The submuscular flap remained vital at a minimum follow-up of 6 months, and the breasts maintained the volume and projection of the NACs [Figures 3–5]. No patient had experienced a recurrence of ptosis or loss of fullness of the upper pole, which had maintained the postoperative fullness for all the duration of the follow-up [Table 3].

- Preoperative (upper line), 6 months after (middle line), and 12 months postoperatively (lower line) views of a 48-year-old woman who underwent mastoplasty with submuscular autoprosthesis after sleeve gastrectomy and weight loss of 49 kg. Note the NAC projection and the fullness of the upper pole

- Preoperative (upper line), 6 months after (middle line), and 12 months postoperatively (lower line) views of a 49-year-old woman who underwent mastoplasty with submuscular autoprosthesis after gastric bypass and weight loss of 60 kg. Note the quality of the scars

- Preoperative (upper line), 6 months after (middle line), and 9 months postoperatively (lower line) views of a 54-year-old woman who underwent mastoplasty with submuscular autoprosthesis after sleeve gastrectomy and weight loss of 55 kg. Note the nice shape and the adequate volume of the breast
| Measures | Overall |
|---|---|
| No. of patients | 15 |
| Jugulum–NAC distance before surgery (cm) | 33.9 (min, 28; max, 40) |
| Jugulum–NAC distance after surgery (cm) | 23.7 (min, 23; max, 25) |
| Jugulum–NAC distance 6 months after surgery (cm) | 24.6 (min, 23; max, 26) |
| Jugulum–NAC distance variation after surgery (cm) | 0.8 (min, 0; max, 2) |
Min = minimum, max = maximum
The incidence of complications was globally 13.3%; no major complications were observed. Two patients had wound dehiscence at the intersection of the vertical suture with the IMF, resolved with secondary-intention wound healing consisting of daily dressing. No cases of hematoma, seroma, or infection were observed. The scars were all of good quality, and no cases of scar migration or keloids were reported. No patients had ptosis recurrence [Table 4].
| Complication | Overall |
|---|---|
| No. of patients | 15 |
| Seroma | 0 |
| Hematoma | 0 |
| Wound dehiscence | 2 |
| Wound infection | 0 |
| Surgical revision | 0 |
| Scar complications | 0 |
| Ptosis recurrence | 0 |
| Total patients with complications | 2 |
All patients were satisfied after surgery: 100% of the patients were extremely satisfied with the breast volume, shape, symmetry, and ptosis correction. About the quality of the scar, 60% of women were somewhat satisfied and 40% were extremely satisfied [Table 5].
| Benchmarks | Extremely dissatisfied | Very dissatisfied | Somewhat dissatisfied | Somewhat satisfied | Extremely satisfied |
|---|---|---|---|---|---|
| Volume | 0 | 0 | 0 | 0 | 15 |
| Shape | 0 | 0 | 0 | 0 | 15 |
| Symmetry | 0 | 0 | 0 | 0 | 15 |
| Ptosis correction | 0 | 0 | 0 | 0 | 15 |
| Quality of scar | 0 | 0 | 0 | 9 | 6 |
Representative cases are shown in Figures 3–6.

- Preoperative (upper line), 6 months after (middle line), and 10 months postoperatively (lower line) views of a 44-year-old woman who underwent mastoplasty with submuscular autoprosthesis after sleeve gastrectomy and weight loss of 40 kg. Note the location of the flap that is too high with abnormal upper pole projection
Discussion
Massive weight loss significantly jeopardizes the appearance of breasts and compromises total body harmony. Depending on the type and the severity of these defects, different techniques have been proposed over time for breast reshaping,[9101112] therefore a precise definition of the problem and an accurate choice of the surgical technique are essential.[23] The main problems of breast reshaping after massive weight loss include the ptosis relapse, loss of fullness of the upper pole, pseudoptosis (“bottoming out deformity”), and upward rotation of the NAC (“star-gazing deformity”). When the ptosis is mild and the volume is enough, it is possible to use silicone prosthesis: in our case, we preferred not to use prostheses because the patients of this case series belonged, as mentioned, to type 2 or 3 in the PRS, and the weight of the prosthesis, especially if large in size, would have caused a ptosis recurrence.[13] In this technique, the flap is sustained by the muscle and gives fullness to the breast without weighing down the skin.
The use of autologous tissues for breast reshaping is widely described. Often in patients after massive weight loss the excess tissue present in the lateral thoracic region or in the epigastrium can be used to restore the volume of the breast. Hurwitz et al.[1415] described a mastoplasty technique using the excess tissue coming from the epigastrium and the lateral thoracic region and creating a double pedicle (one medial and one lateral) autoprosthesis to fill and give projection to the breast mound. However, this technique offered better results when combined with a reverse abdominoplasty and often required a second operative time with a prosthetic implant. They also reported an incidence of necrosis of the apical portion of the flaps in up to 20% of cases,[16] probably because of the considerable length of the flaps. No case of necrosis was instead observed in our study, probably due to the favorable relationship between base flap and its height. The technique by Rubin and Khachi[17] can be used only in case of considerable dermoadipose excess in the lateral thoracic region; therefore, it is not usable in patients with thin and narrow thorax. Losken and Holtz[18] proposed a technique already described by Silveira Neto,[19] based on Wise’s markings with superomedial pedicle flap that also contains the areola. This technique is suitable for patients with sufficient breast volume in the upper pole but could not be used in many of the patients of this case series, who had a poor residual dermoglandular tissue. The use of superior abdominal excess during a reverse abdominoplasty has also been described.[20] The excess tissue is de-epithelialized and reshaped as an autoprosthesis to improve volume and projection. However, with this technique the risk of cancel the IMF is high because moving the flap from the upper abdomen to the breast, the pedicle has to cross the inframmary fold with the risk of reducing its definition.
The use of remote flaps taken from the abdomen (transverse rectus abdominis myocutaneous flap or deep inferior epigastric perforator flap), from the inner thigh or gluteal region, or those based on lateral intercostal artery perforator or anterior intercostal artery perforator[212223] are technically more demanding and require microsurgical knowledge. In addition, these techniques are more invasive, often require longer operative time, and are not feasible if the patients previously underwent upper body lift, brachioplasty, or abdominoplasty. Our technique proved to be safe; recovery times were rapid with a short hospital stay and a quick return to daily activities. No major complications were reported, and just two patients experienced wound dehiscence.
Moreover, our technique proved to be extremely effective for the correction of ptosis and ensured long-lasting results; other authors proposed the anchorage of the flap to the muscle fascia or to the periosteal rib to prevent the recurrence of ptosis and the flattening of the upper pole.[24252627282930313233] In our case, jugulum–NAC distance was adequately restored with a minimal variation in the follow-up time and the breast maintained its projection [Figures 3–5]. In fact, the weight of the flap is supported by the pectoral muscle, and this avoids the recurrence of ptosis because of the effect of gravity on loose and poor-quality tissues. It is preferable to not place the flap too high to avoid abnormal projection of the upper pole because the flap does not descend over time [Figure 6].
All the patients were extremely satisfied with the breast shape, volume, symmetry, and ptosis correction. Minor satisfaction was shown by the patients for scar location and extension; however, the scars were similar to those of other techniques proposed to treat breast deformities of the same type in PRS. These results would encourage the use of the technique.
Conclusion
Mastoplasty with submuscular autoprosthesis is an effective technique for treating moderate or severe breast ptosis in patients after massive weight loss. In fact, it allows the removal of the redundant skin, obtaining a satisfactory shape and volume of the breast, using only patient’s tissues, and avoiding the cost of the prostheses. This technique also guarantees stable and long-lasting results and avoids recurrence of ptosis and emptying of the upper pole without increasing the incidence of complications. Moreover, considering the positive results and patient satisfaction, we currently use this technique even in other situations such as gigantomastia, mammary asymmetry, and aesthetic mastopexy. Finally, in the era of hybrid surgery, we are evaluating to combine our technique with breast lipofilling to improve the aesthetic results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Estudo histomorfome′trico comparativo do cola′geno e elastina na pele abdominal humana apo′s perda ponderal macic¸a. [Tese de Mestrado] In: Faculdade de Medicina. Universidade de São Pa São Paulo; 2009. p. :87. Available from: http://www.teses.usp.br [Last accessed on 30 March 2018]
- [Google Scholar]
- Preventing the “bottoming out” and “star-gazing” phenomena in inferior pedicle breast reduction with an acellular dermal matrix internal brassiere. Aesthetic Plast Surg. 2010;34:760-7.
- [Google Scholar]
- Breast reshaping after massive weight loss. In: Aly A, ed. Body contouring after massive weight loss. St Louis, MO: Quality Medical Publishing; 2006. p. :361-78.
- [Google Scholar]
- A classification of contour deformities after bariatric weight loss: the Pittsburgh rating scale. Plast Reconstr Surg. 2005;116:1535-44.:1545-44.
- [Google Scholar]
- Creation and evolution of 30 years of the inferior pedicle in reduction mammaplasties. Plast Reconstr Surg. 2002;110:960-70.
- [Google Scholar]
- Reduction mammaplasty with the inferior pedicle technique: early and late complications in 371 patients. Br J Plast Surg. 1996;49:442-6.
- [Google Scholar]
- Vertical mammaplasty: early complications after 250 personal consecutive cases. Plast Reconstr Surg. 1999;104:764-70.
- [Google Scholar]
- Augmentation mastopexy with implant and autologous tissue for correction of moderate/severe ptosis. J Invest Surg. 2016;29:40-50.
- [Google Scholar]
- Postbariatric surgery breast reshaping: the spiral flap. Ann Plast Surg. 2006;56:481-6.
- [Google Scholar]
- A clinical review of total body lift surgery. Aesthet Surg J. 2008;28:294-303.:304-303.
- [Google Scholar]
- Mastopexy after massive weight loss: dermal suspension and selective auto-augmentation. Clin Plast Surg. 2008;35:123-9.
- [Google Scholar]
- Versatility of the superomedial pedicle in managing the massive weight loss breast: the rotation-advancement technique. Plast Reconstr Surg. 2007;120:1060-8.
- [Google Scholar]
- Mastoplastia setorial com pediculo areolar interno. :13. Anais do XIIIth Congresso Brasileiro de Cirurgia Plastica, Porto Alegre, Brazil November 1976
- [Google Scholar]
- Augmentation mammaplasty by reverse abdominoplasty (AMBRA) Plast Reconstr Surg. 2009;124:1662-72.
- [Google Scholar]
- Autologous breast augmentation with the lateral intercostal artery perforator flap in massive weight loss patients. J Plast Reconstr Aesthet Surg. 2009;62:65-70.
- [Google Scholar]
- Mastopexy with autologous augmentation after massive weight loss: the intercostal artery perforator (ICAP) flap. Ann Plast Surg. 2006;57:361-5.
- [Google Scholar]
- Anterior intercostal artery perforator flap autologous augmentation in bariatric mastopexy. Plast Reconstr Surg. 2012;130:917-25.
- [Google Scholar]
- Reduction mammaplasty using inferior pedicle technique combined with dermal suspension. Plast Reconstr Surg. 2003;111:1362-3.
- [Google Scholar]
- Breast reduction with inferior pedicle fascial suspension. Aesthetic Plast Surg. 2005;29:532-7.:538-7.
- [Google Scholar]
- Improving the results of inferior pedicle breast reduction using pedicle suspension and plication. Aesthetic Plast Surg. 2006;30:390-4.
- [Google Scholar]
- Long-lasting evolution of ptosis control after reduction mammaplasty using the hammock technique. Aesthetic Plast Surg. 2007;31:266-74.
- [Google Scholar]
- The dermal suspension sling: shaping the inferior pedicle during breast reduction. Aesthetic Plast Surg. 2011;35:608-16.
- [Google Scholar]
- A new technique of reduction mammaplasty: dermis suspension and elimination of medial scars. Br J Plast Surg. 1999;52:45-51.
- [Google Scholar]
- Mammoplasty: breast fixation with dermoglandular mono upper pedicle flap under the pectoralis muscle. Aesthetic Plast Surg. 1998;22:276-83.
- [Google Scholar]
- Reduction mammaplasty and mastopexy with superficial fascial system suspension. Plast Reconstr Surg. 1999;103:1411-20.
- [Google Scholar]
- Curtain type combined pedicled reduction mammoplasty with internal suspension for extensive hypertrophic and ptotic breasts. Br J Plast Surg. 2003;56:114-9.
- [Google Scholar]






