Translate this page into:
Follicular Unit “Exploitation”: Follicular Unit Extraction Followed by Laser Hair Reduction—A Novel Approach to Repigmentation of Postburn Leukodermic Scars
Address for correspondence: Dr. Sidharth Sonthalia, Department of Dermatology, SKINNOCENCE: The Skin Clinic and Research Center, C-2246, Sushant Lok 1, Block-C, Gurugram 122009, Haryana, India. E-mail: sidharth.sonthalia@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Correction of depigmentation of postburn leukodermic scars is daunting. In contrast to vitiligo, the success rate of skin grafting techniques is much lower in postburn scars owing to altered skin architecture and poor graft uptake. Cellular transfer techniques such as noncultured epidermal or epidermal or keratinocyte suspension suffer the limitations of modest efficacy and high procedural cost. Follicular transplantation by the follicular unit extraction technique is being extensively used in vitiligo. Recently, it has been reported for the correction of scar alopecia. Although this approach is expected to significantly repigment pliant scars, the cosmetic unacceptability of the retained hairs may warrant removal. We describe an innovative three-step protocol to provide a repigmented smooth scar. We vernacularly labeled this technique follicular unit “exploitation,” as the follicular units “exploited” positively for repigmentation were later removed by laser hair reduction.
Keywords
Follicular unit exploitation
follicular unit extraction
laser hair reduction
leukodermic scar
repigmentation
skin grafting
vitiligo
Introduction
Leukodermic scars following thermal or caustic burns pose a therapeutic conundrum. In contrast to the good outcome of immunomodulatory therapies in vitiligo, repigmentation of leukodermic scars mandates a direct melanocyte transfer technique. Phototherapy, skin grafting, and cellular melanocyte transfer (CMT) with noncultured epidermal or epidermal melanocyte cell suspension transfer have provided limited repigmentation in such scars.[1] Follicular unit extraction (FUE), the most popular approach for hair transplantation (HT) has been successfully repurposed for repigmenting vitiligo, including cases recalcitrant to CMT techniques.[23]
Although, this concept is worth extrapolation to repigment leukodermic scars, the cosmetic unacceptability of the post-FUE retained hairs remains a huge concern, for example, over the arm or forearm of a lady.
We devised an innovative three-step protocol involving HT by FUE technique in the leukodermic patches, phototherapy for pigment spread followed by laser hair reduction (LHR) to provide a hairless smooth-textured aesthetically pleasing repigmented scar.
Case Report
A 43-year-old healthy lady presented with a five-year-old postburn scar involving her right upper limb interspersed with hypo- to depigmented areas. The flatness, pallor, and soft and supple consistency confirmed the scar to be fully matured. Past treatments included multiple sessions of phototherapy and two sessions of different types of CMT techniques performed three years back, with treatment failure. Her psychological well-being with Patient Health Questionnaire (PHQ)-9 was assessed and a score of 13 confirmed moderate depression.
Owing to previous therapeutic failures, patient’s depression, and desperate desire for cosmetic improvement in the scar, we planned and suggested an innovative three-step treatment protocol that we vernacularly labeled follicular unit “exploitation” (FUe). The steps include the following: FUE in the leukodermic areas for pigmentation induction, phototherapy for pigment spread, and hair reduction with LHR. As the scar was fully mature with decent elasticity, it was viable for sustaining follicular implants. Realistic expectation, treatment duration, potential adverse effects, and cost issues were discussed during pre-procedure counseling. The patient was satisfied and she volunteered for the treatment protocol. Before surgery, she was referred to a psychiatrist who prescribed tablet escitalopram (5mg OD) for eight weeks. She was not on blood thinners or any other medication. Signed informed consent was obtained. The treatment protocol was conducted maintaining the ethical principles of human research outlined in the World Medical Association’s Helsinki Declaration 2013.[4]
FUe: Innovative Sequential Protocol
Follicular units were extracted from the occipital scalp of the patient using 0.8mm punches under local anesthesia and implanted in the depigmented areas of the scar. Initially, a test area of 10 units was carried out [Figure 1A]. The repigmentation over the test area was assessed after three months and was found satisfactory [Figure 1B]. The remaining depigmented areas of the scar were then transplanted by FUE maintaining 0.5cm interfollicular spacing [Figure 1C]. Repigmentation of these areas also started in 2.5–3 months and completed in 10 months, expedited with alternate day home-based narrowband ultraviolet B therapy. Three months later [Figure 2A], the third phase consisting of eight sessions of LHR with alexandrite laser was conducted to significantly reduce the number, caliber, color, and growth rate of the hair follicles. One month after completion of the LHR protocol, we had achieved >80% repigmentation with a smooth, almost hairless scar [Figure 2B]. The highly satisfied patient rated the overall improvement >90%. A repeat PHQ-9 score was only 3 (representing nil depression) despite being off escitalopram for many months. Excepting the expected perioperative discomfort, and temporary pain and burning sensation during FUE and LHR respectively, the overall patient tolerability was excellent; with no other local or systemic adverse effects noted. The patient is on six-monthly follow-up for maintenance sessions of LHR, and no pigment dilution was noticed till 12 months after the last LHR session.
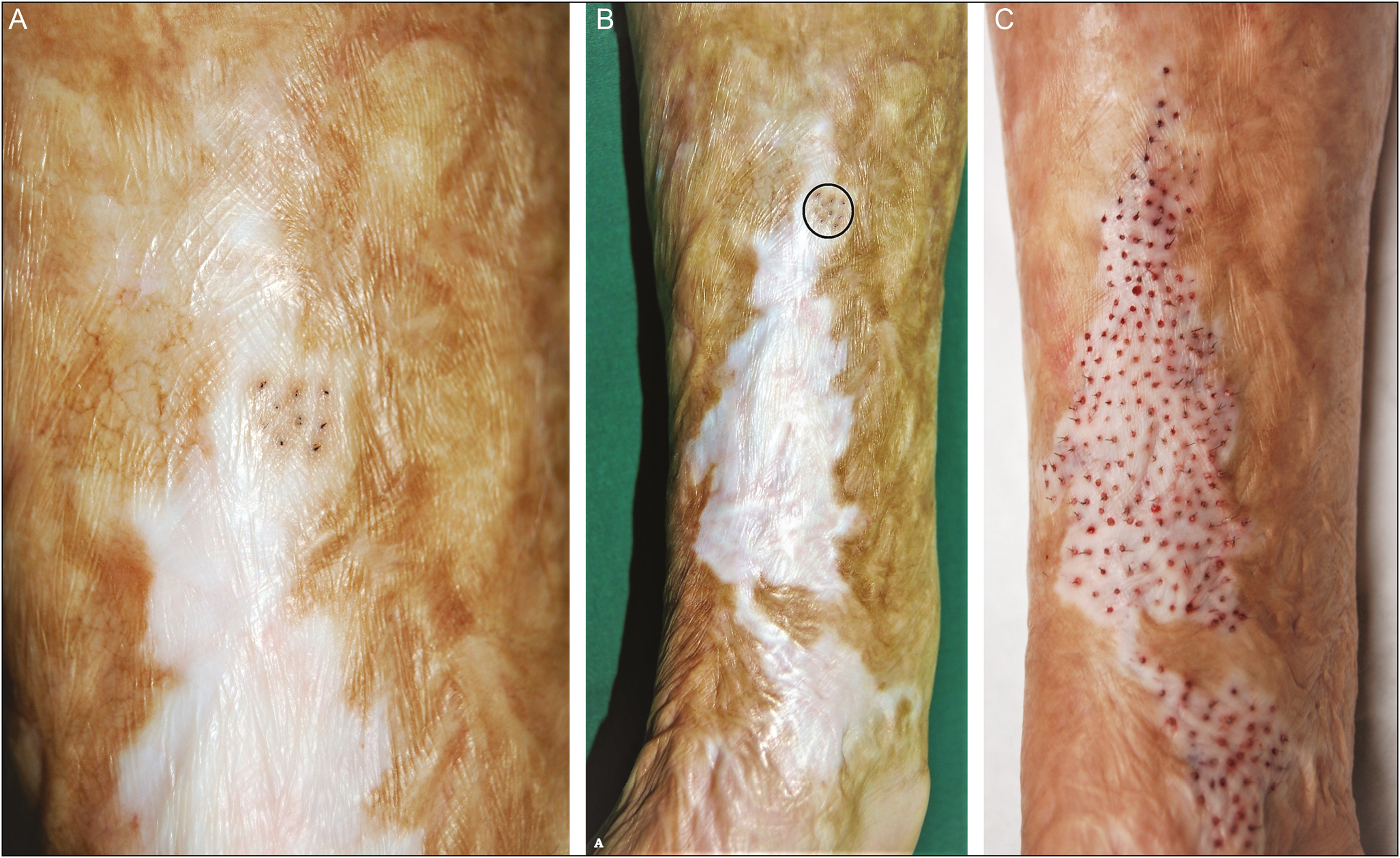
- Postburn leukodermic scar involving the forearm of an adult lady. (A) Baseline appearance of a part of the scar with focus on the test site. (B) View of the entire scarred area with visible repigmentation at the test site three months after follicular implantation (black circle). (C) Immediately after completion of follicular unit grafting in the remaining leukodermic areas of the scar
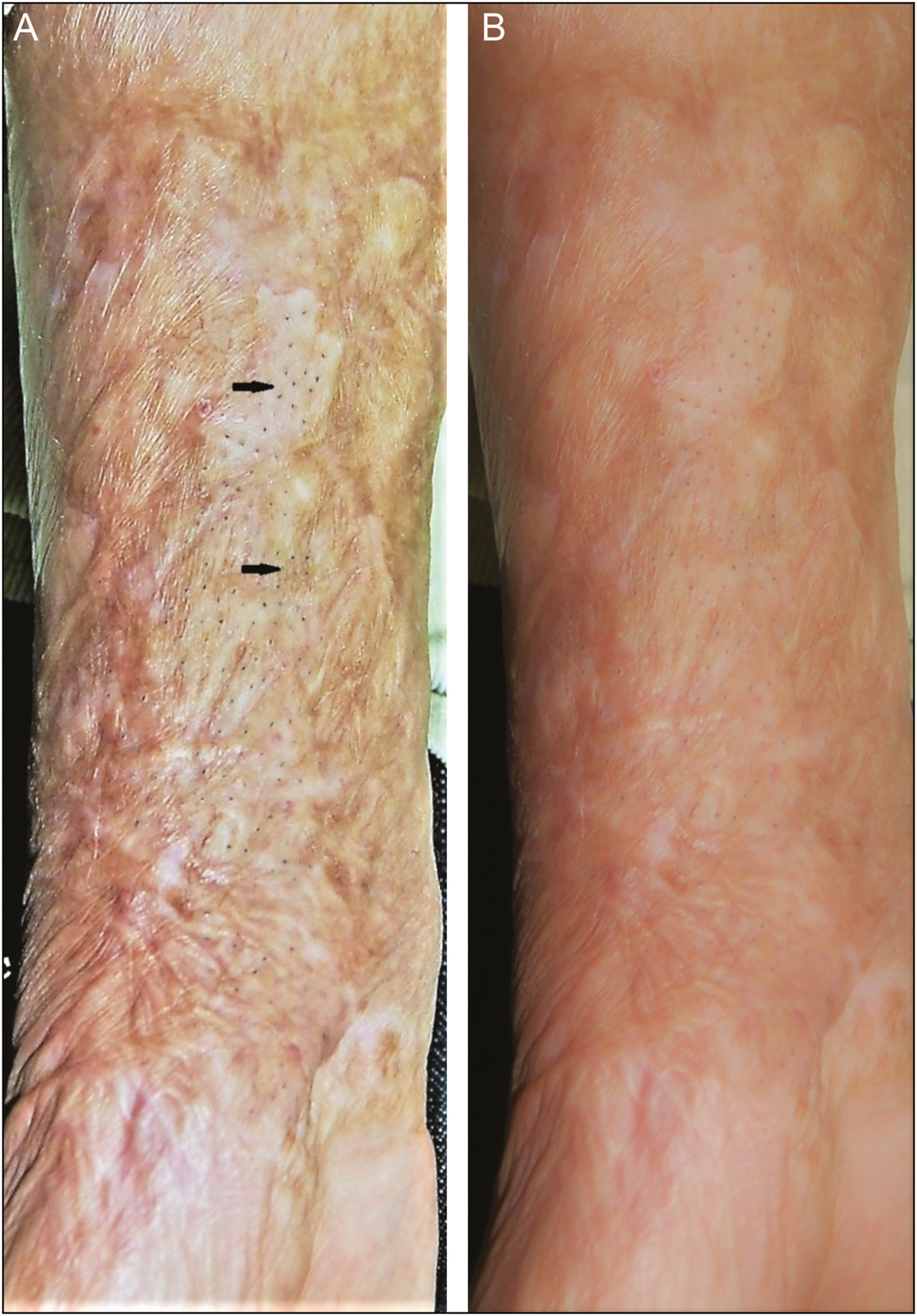
- Post follicular unit implantation of the leukodermic scar. (A) Three months later (after completed repigmentation) revealing prominence of many hair follicles (black arrows). (B) Appearance after six alexandrite LHR sessions revealing retained pigmentation, significant reduction in hair shafts with an overall cosmetically satisfactory outcome
Discussion
The transfer of melanocyte sourced from healthy skin or follicular units constitutes the basic principal of surgical correction of any acquired disorder of depigmentation whether stable vitiligo or leukoderma of postburn scar. Melanocyte transfer may be carried out by a tissue graft or cellular graft or CMT. In contrast to the macules of stable vitiligo, skin grafting into the depigmented areas of a postburn scar is tricky owing to the altered skin architecture, including loss of subcutaneous tissue, areas of hypertrophy, and reduced elasticity. In scarred tissue, tissue grafting has been attempted by split-thickness, chip, sheet, and mini punch skin grafting methods.[4] Although effective, these methods suffer the limitations of failure of graft uptake and/or need for large areas of donor skin. Cobblestone appearance is a common adverse cosmetic outcome of mini punch grafting. CMT techniques are preferred when treating large areas, as in our case. Cells are extracted from the unaffected skin or follicles and transplanted as a suspension. Cellular methods include transplantation of cultured pure melanocytes, cocultured melanocyte–keratinocyte cell suspension, cultured epidermis, and noncultured extracted hair follicle outer root sheath cell suspension.[5] However, nonavailability at many centers, high infrastructural cost, and therapeutic failure (as experienced by our patient) constitute major limitations of CMT in the attempt to repigment a postburn leukoderma.[6]
HT by FUE method is being increasingly used for stable vitiligo.[23] However, to the best of our knowledge, the use of HT in postburn scar has only been described once before, that too for the treatment of scar alopecia and not depigmentation per se.[7] Although the pre- and postsurgical images of the review article by Farjo et al.[7] do show significant repigmentation in depigmented areas, their purpose and emphasis was hair restoration in the scar. In our case, the patient had failed two CMT techniques having spent significant amount of money, and needed repigmentation without hairs. Scar maturity, good elasticity, and preserved subcutaneous tissue rendered our patient a good candidate for FUE in the scar. The advantage of follicular grafting over conventional skin grafting has been previously demonstrated and published by us.[8] This includes improved survival and uptake of the follicular grafts being wedged in the skin, and repigmentation of larger areas with FUE. After achieving the desired repigmentation with FUE and phototherapy, her scar was relieved of the transplanted hairs with regular LHR sessions. We sincerely believe that this is the first report of successful repigmentation of a leukodermic postburn scar with follicular implantation and maintenance of cosmesis by subsequent LHR. This novel approach may be considered for leukodermic scars that fail to repigment by conventional methods. We call this technique follicular unit “exploitation” or FUe, as the follicular units are positively exploited for their repigmenting potential, but later removed by LHR.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Autologous, noncultured epidermal cell suspension grafting in the management of mechanically and chemically induced leukodermic scars. J Cutan Med Surg. 2015;19:488-93.
- [Google Scholar]
- Repigmentation of vitiligo using the follicular unit extraction technique. Dermatol Surg. 2014;40:1425-7.
- [Google Scholar]
- Restoration of pigmentation by follicular unit extraction transplant in three cases of focal vitiligo recalcitrant to therapy including with previous nonculture melanocyte-keratinocyte transplant. Int J Trichology. 2016;8:87-8.
- [Google Scholar]
- [The Helsinki Declaration of the World Medical Association (WMA). Ethical principles of medical research involving human subjects] Pol Merkur Lekarski. 2014;36:298-301.
- [Google Scholar]
- Comparison between autologous noncultured extracted hair follicle outer root sheath cell suspension and autologous noncultured epidermal cell suspension in the treatment of stable vitiligo: a randomized study. Br J Dermatol. 2013;169:287-93.
- [Google Scholar]
- Combined treatment of post-burn leukoderma with autologous minigrafting and topical Khellin-natural sunlight among Egyptian patients. Asian J Dermatol. 2014;6:25-33.
- [Google Scholar]
- Hair transplantation in burn scar alopecia. Scars Burn Heal. 2015;1:2059513115607764.
- [Google Scholar]
- Follicular unit transplantation in the treatment of segmental vitiligo of the beard. Egyptian J Dermatol Androl. 2013;33:3-10.
- [Google Scholar]






