Translate this page into:
Management of Delayed Skin Necrosis Following Hyaluronic Acid Filler Injection Using Pulsed Hyaluronidase
Address for correspondence: Dr. Sukhbir Singh, Department of plastic and cosmetic surgery, Resplendent The Cosmetic Studio, R-9, Greater Kailash Part 1, New Delhi 110048, India. E-mail: sukhi_1@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Facial fillers are minimally invasive aesthetic procedures performed for facial rejuvenation and contouring all over the world. Fillers even in the most experienced hands can lead to fatal complications such as vascular complications that need to be managed immediately with the help of hyaluronidase protocols mentioned in literature. In this case report, a patient was asymptomatic with no signs of vascular occlusion such as blanching or poor capillary refill for 48 h. He came after more than 48 h of the filler injection with complaints of pulsating pain in the right infraorbital and nasolabial area. We noticed necrosed microvesicles in the infraorbital artery territory with signs of impending skin necrosis extending from right infraorbital region up to the nasolabial fold (slightly medial to it). He was treated immediately with three pulsed doses of 500 units higher dilation of 10 ml each every hour (reconstitution carried out using 3mL normal saline). The skin color improved with decreased pain, and the next day (after 14 hours) we injected 500 units of hyaluronidase in higher dilution of 10mL as slight redness was still present. Skin redness, swelling, and pain disappeared the following day. Skin was completely healed and by 15 days we noticed slight post-inflammatory hyperpigmentation, which was easily managed with Q-switched laser and creams. We hereby report a case of delayed skin necrosis (>48 h) following filler injections in the cheek area, in the infraorbital artery vascular territory, which was successfully managed with pulsed dose of hyaluronidase.
Keywords
Delayed necrosis
hyaluronic acid filler
hyaluronidase
infraorbital artery
microvesicles
Introduction
Facial fillers are minimally invasive aesthetic procedures performed for facial rejuvenation and contouring all over the world. According to the global statistics 2016 of American Society of Plastic Surgeons, soft-tissue fillers are second most common minimally invasive procedures all over the world. But as all good things have some negative effects, fillers even in the most experienced hands can lead to fatal complications such as vascular complications, which need to be managed immediately with the help of hyaluronidase protocols mentioned in literature.[1]
In this case report, a patient was asymptomatic with no signs of vascular occlusion such as blanching or poor capillary refill for 48 h. He came to the clinic more than 48 h of the filler injection with complaints of pulsating pain in the right infraorbital and nasolabial area. We noticed necrosed microvesicles in the infraorbital artery territory with signs of impending skin necrosis and redness (livedo reticularis) extending from infraorbital region up to the nasolabial fold and slightly medial to it along with tenderness of tissues. He was treated immediately with 3 pulsed doses of hyaluronidase 500 units each every hour after giving test dose for the same. He felt much better with pain and swelling decreased, and the next day (after 14 hours) we injected more 500 units of hyaluronidase in higher dilution of 10mL as slight redness was still present. There was no ulcer and only necrosed microvesicles were observed. Skin redness, swelling, and pain disappeared the following day and during the recovery phase we followed up the patient. Skin had completely healed and by 15 days we noticed slight post-inflammatory hyperpigmentation (PIH), which was easily managed with Q-switched laser and creams.
We hereby report a case of delayed skin necrosis (>48 h) following filler injections in the cheek area, in the infraorbital artery vascular territory, which was successfully managed with pulsed dose of hyaluronidase.[1]
Case Report
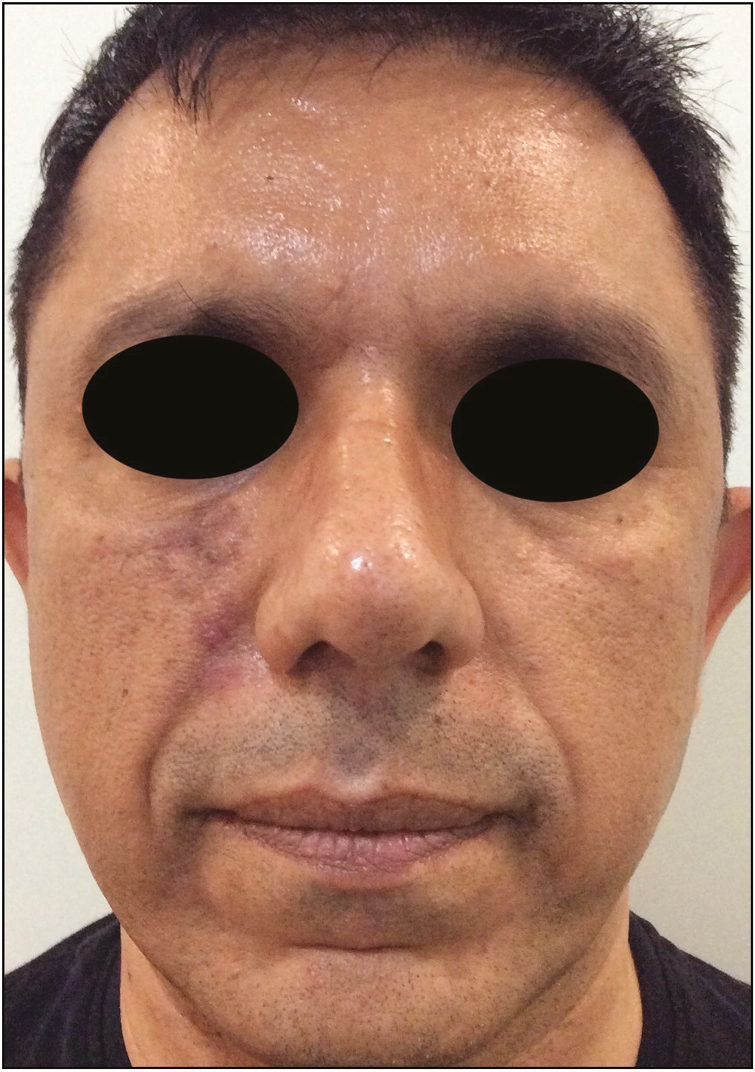
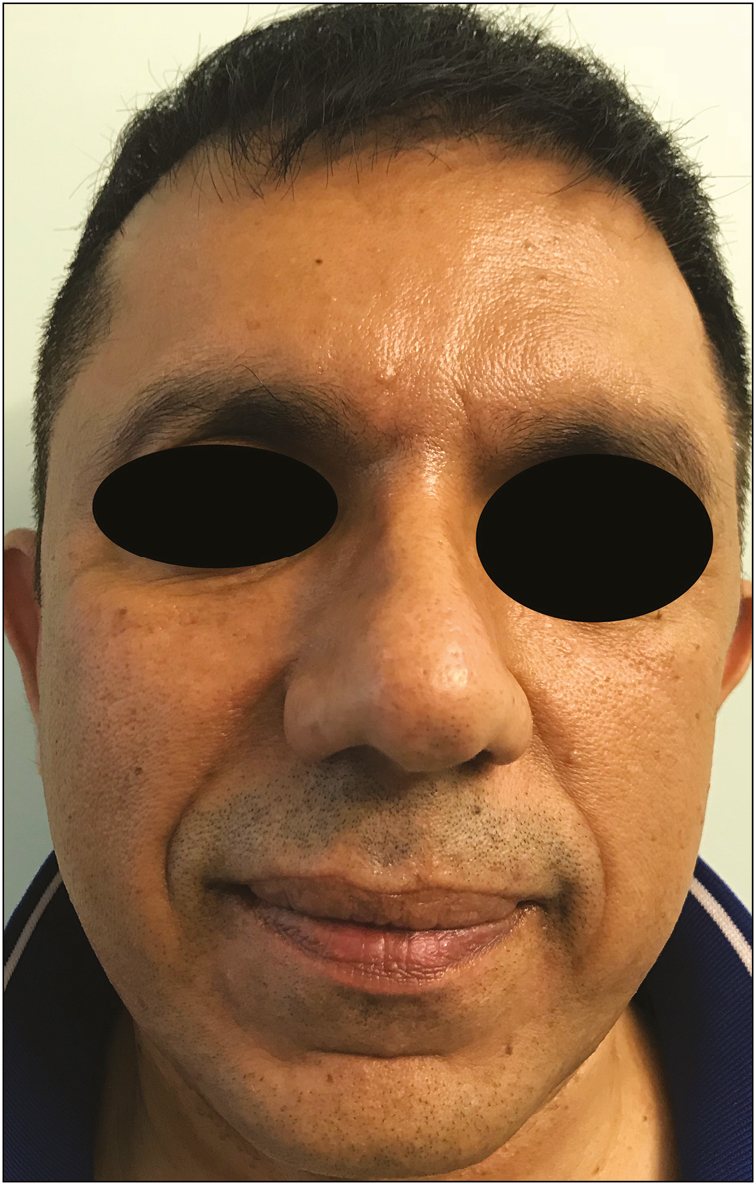
A 50-year-old male patient was injected in a private clinic in Delhi, India, for multiple areas of face on both sides. The experienced injector performed the filler injection with 27-G 0.5-in sharp needle. The hyaluronic acid (HA) concentration was 20mg/mL and the filler also contained lignocaine. A written informed consent was taken from the patient before starting the procedure. HA filler was injected at four different sites on each half of the face: 0.1mL was injected each at the zygomatic arch and zygomatic eminence, 0.05mL was injected below the infraorbital foramen level, and 0.1mL was injected at the nasolabial region (canine fossa). The injections were completed at both sides uneventfully and the patient did not complain of any excessive pain or discomfort after the injections. Patient left the clinic uneventfully. The next day as a routine, a follow-up call was made, and the patient expressed his happiness about the procedure without any complaints of pain or redness. But the next day, which was more than 48 h of the procedure, patient called up and over the phone he complained about redness and pulsating pain in right cheek area alone. We told him to come to the clinic immediately. He came within 2 h of the call, and on examining him, we were shocked to see necrosed microvesicles in the infraorbital artery territory with signs of impending skin necrosis and redness (livedo reticularis) extending from infraorbital region up to the nasolabial fold and slightly medial to it as seen in Figure 1 along with tenderness of tissues. We suspected vascular compromise of the infraorbital artery territory area with minimal involvement of the communication with the facial artery as it did not extend beyond the nasolabial fold and also spared the angular artery and lateral nasal artery territory area (lateral nasal wall, sides, ala and other nasal areas with its anastomosis). We immediately started hyaluronidase injections. One vial of hyaluronidase contains 1500 units, so we decided to split the 1500 units into 3 equal divided doses and injected it every 1 h rather than in a 1500-unit direct dose. So, we first gave 500-unit dose using a 25-G cannula all along the cheek and nasolabial areas extending slightly beyond the involved areas territory. After 1 h, we did not notice any improvement and the pain was still persisting, so we gave another 500 units of hyaluronidase. After 2 h, pain had decreased significantly but some swelling and redness was still present. So we repeated another 500 units of hyaluronidase, and after 3 h following 3 pulsed doses of hyaluronidase, we saw a remarkable change in the skin color, redness, and swelling. We observed the patient for one more hour, and thereafter he was sent back home and advised to inform immediately if he felt any more pain or redness and if swelling increased. The next day, which was exactly 14 h following our last (third) pulsed dose of hyaluronidase, the patient came to the clinic. Patient had no complaints of pain but we saw minimal redness in the nasolabial area. We repeated 500 units more hyaluronidase with higher dilution of 10mL. We observed the patient for 1 h after which he was sent home and reviewed after 48 h. On this review, as seen in Figure 2, redness and swelling had completely disappeared and healing had started well. Patient was on regular follow-up and we reviewed him after 15 days and found complete healing of the tissues with no residual scarring, as seen in Figure 3. For his PIH, we gave him Q-switched laser therapy and creams to apply. We followed the patient for 3 months, and at the end of 3 months, as seen in Figure 4, skin had completely healed without any residual scarring or pigmentation.

- Necrosed microvesicles in right infraorbital artery territory with signs of impending skin necrosis extending from right cheek to right nasolabial fold and just medial to it

- Forty-eight hours after last dose of hyaluronidase injection of 500 units in higher dilution, skin is in healing phase with no redness or skin ischemia
- Fifteen days postinjections, showing complete skin healing with mild PIH
- Three months after filler injections, showing complete healing with no scarring and resolved pigmentation after Q-switched laser
Discussion
We are presenting this case report because of its uniqueness in the fact that most of the intra-arterial occlusions and signs of ischemic skin necrosis occur immediately or within few hours of the filler injection going intravascular. There have been very rare reports of delayed necrosis all over the world following filler injections. In this case, the patient reported pain only after 48 h following filler injections, which is an important sign of intra-arterial injection,[2] but may not be appreciated well because of the lignocaine present in filler injections.[2] This case report is a caution for all injectors that signs and symptoms can occur even after 48 h following injections and one has to be careful and vigilant if any patient complains of any excessive pain or redness later on also. Thorough knowledge of the anatomy is utmost important for demarcating accurately the vascular territory involved; in this case, the infraorbital artery was involved with minimal involvement of the communication with facial artery and its branches especially the angular and lateral nasal artery, which supply the entire nasal area and lateral nasal walls with their corresponding anastomosis. Bravo et al.[3] reported a case of delayed necrosis more than 36 h of HA injection in the zygomaticofacial artery territory. The hypothesis given was of an embolus after the injection due to fragment of filler going intravascularly and migrating further because of facial muscle movement and poor collateral circulation to supply nutrition to the area, resulting in late necrosis. This may be the probable cause in our case also along with a component of external compression of the vessel because of edema around the foramen level rather than intravascular injection of the filler causing complete occlusion. Hyaluronidase is essential for every aesthetic physician practicing in injectables.[4] The high-dose pulsed hyaluronidase protocol[5] suggests using 500 units for one vascular territory and 1,000 units for two areas, and the same has been followed in this case.[1] Also there is no unanimity on dosage and the interval between two doses of hyaluronidase.[6] In our case, we used 500 units of hyaluronidase as pulsed doses every hour followed by one more 500 units in more dilution of 10mL the next day. This helped us to completely heal the skin without any residual scarring. The high-dose pulsed hyaluronidase works on the principle of achieving high concentration levels of hyaluronidase at local tissue level for sufficiently long duration for it to dissolve the HA material present in the affected areas of filler injections.[1] There is no documentation of natural HA being reduced or degraded by hyaluronidase injections. Only hypersensitivity reactions are documented in literature after hyaluronidase injections.
In conclusion, fillers though quite lucrative can lead to devastating complications if not managed properly and adequately. Thorough anatomical knowledge of the vascular territories is of utmost importance before venturing into injectables.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;37:814-25.
- [Google Scholar]
- Nicolau syndrome due to hyaluronic acid injections. J Cosmet Laser Ther. 2016;18:239-44.
- [Google Scholar]
- Delayed-type necrosis after soft tissue augmentation with hyaluronic acid. J Clin Aesthet Dermatol. 2015;8:42-7.
- [Google Scholar]
- Hyaluronidase in cosmiatry: What should we know? Surg Cosmet Dermatology. 2015;7:197-203.
- [Google Scholar]
- Successfully managed impending skin necrosis following hyaluronic acid filler injection, using high-dose pulsed hyaluronidase immediately after the filler injections. Plast Reconstr Surg Glob Open. 2018;6:e1639.
- [Google Scholar]
- Patient factors influencing dermal filler complications: Prevention, assessment, and treatment. Clin Cosmet Investig Dermatol. 2015;8:205-14.
- [Google Scholar]






