Translate this page into:
Treatment of Xanthelasma Palpebrarum using Pulsed Dye Laser: Original Report on 14 Cases
Address for correspondence: Dr. Kannangath Jyothy, 2nd Floor, Balakrishnan Hospital, 100 Feet Road, Coimbatore 641012, Tamil Nadu, India. E-mail: joederm@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Xanthelasma palpebrarum, a benign xanthoma occurring around the eyes, are treated using lasers like carbon dioxide, argon, pulsed dye, YAG, and diode(1450) laser .Several studies on PDL for xanthelasma palpebrarum (XP) have been reported from abroad but as per our knowledge there are no Indian studies in this regard. We report the efficacy of pulsed dye laser in the management of xanthelasma palpebrarum in Indian patients.
Keywords
Pulsed dye laser
xanthelasma palpebrarum
Indian study
Introduction
Xanthelasma palpebrarum (XP), the most common cutaneous xanthoma, presents with yellowish plaques over the medial aspect of upper and lower eyelids. It is a benign skin problem commonly affecting the middle-aged and the older adults and can be very disfiguring.[1] Various modalities of treatments are available ranging from medicines such as probucol, alirocumab, and pingyangmycin to simple excision, cryotherapy, TCA peels, phenol cautery, radio frequency, and lasers.[23] The disadvantages of the procedures include delayed wound healing, chances of scarring, pigmentary alterations, and recurrence. Among the lasers used, pulsed dye laser (PDL) is a promising approach but has not been widely used in India for the treatment of XP. We report the efficacy of PDL in the management of XP.
Materials and Methods
Five cases of XP, aged between 40 and 50 years, were selected for PDL treatment after proper history taking and examination. They had in total 14 lesions, size ranging from 4 to 7mm. Two of them had hypercholesterolemia and one patient had diabetes and was on OHA (oral hypoglycemic agent). They had no absolute contraindications such as active infection at the treatment site or pregnancy. The selected patients were counseled and photo documentation was done before the procedure. Eutectic mixture of lignocaine (2.5% wt/wt) and prilocaine (2.5%) was used as topical anesthetic agent. Intraocular eye shields were used before starting the laser session. The patients were given four sessions of PDL (Vbeam; Candela, USA) treatment at an interval of 2 weeks. The parameters used were wavelength of 595nm, fluence 7–10 mj, pulse duration 1.5–3ms, spot size 5mm, number of passes 2, and DCD settings 30/10ms. After the procedure, the patients were observed for immediate complaints such as erythema, edema, pain, and blister formation. Most of them showed a bluish discoloration immediately at the treated site. All the patients tolerated the procedure well and had no pain or purpura. All of them developed minimal crusting that cleared within 5 days. They were asked to apply a repairing cream containing Rhealba oat and hyaluronic acid (0.2%) for 5 days and were advised to protect the treated area from ultraviolet rays till they completed their treatment. They were asked to visit the clinic after 2 weeks for assessment and for subsequent sessions. Photo documentation was done during each visit. The results were assessed clinically and by comparing photographs. They were followed up for 2 years at an interval of 6 months.
Results
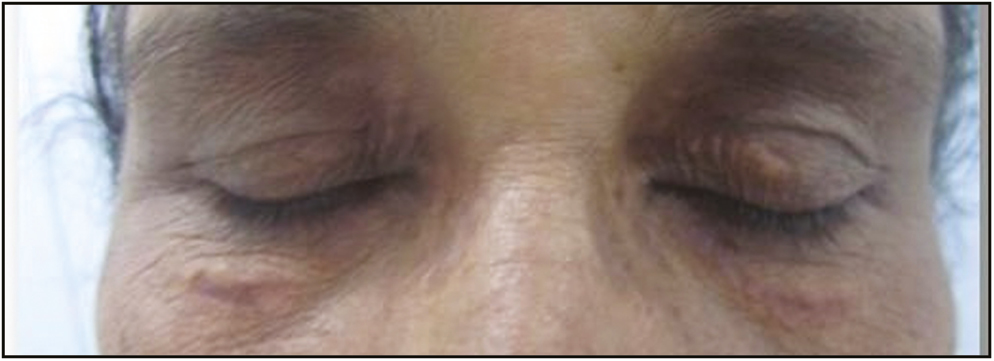
All the patients showed 90%–100% clearance after four sessions [Figure 1–4]. None of them had any complications such as scarring or dyschromia. There was no recurrence in any of the patients at the end of 2 years.

- Xanthelasma palebrarum: before PDL treatment

- Xanthelasma palebrarum: after four sessions of PDL

- Xanthelasma palebrarum: before PDL treatment
- Xanthelasma palebrarum: after four sessions of PDL
Discussion
XP is commonly treated surgically either by simple excision or by using radio frequency or lasers. Ablative procedures such as radio frequency and carbon dioxide/argon laser require local anesthetic injection; cause pain; and carry risk of infection, scarring, and pigmentation.[45678] These lesions could bleed profusely as the foam cells are intermingled with blood vessels. Moreover these techniques have downtime of 7–10 days. To overcome these issues, nonablative lasers such as PDL have been tried and are found to be effective in the management of XP.[9] But no studies on PDL are reported from India till date.
The exact mechanism of xanthelasma laser surgery is not fully understood. It is presumed that the heat energy, which originates from the coagulation of the vessels within the upper dermis, leads to a damage of the perivascular foam cells. The coagulation of the pathologically hyperpermeable vessels would lead to a block of the leakage of lipids into the tissue and thereby prevent recurrent lesions.
All the patients responded well to the PDL treatments and lesions were removed fully after the fourth session. No local anesthetic was injected and none of them had significant periorbital bruising, which is a major aesthetic advantage over ablative laser treatments. The postprocedure swelling was minimal and was managed with anti-inflammatory creams. There was no scarring as the skin was not cut or ablated during the procedure and none of the patients developed post-inflammatory hyper/hypopigmentation following any of the sessions. The patients were followed for 2 years after complete clearance and none of them had recurrence within that period. This is also a significant advantage over other conventional methods.
Conclusion
Our results prove the efficacy of PDL in the management of XP and this method should be offered for those patients who opt for nonablative laser procedures. Treatment of XP with PDL causes less scarring and the recurrence rate is also low.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Xanthelasma palpebrarum: A review and current management principles. Plast Reconstr Surg. 2002;110:1310-4.
- [Google Scholar]
- Assessment of efficacy and tolerability of different concentrations of trichloroacetic acid vs. carbon dioxide laser in treatment of xanthelasma palpebrarum. J Cosmet Dermatol. 2015;14: 209-15.
- [Google Scholar]
- Lasers in dermatology and medicine. London: Springer-Verlag; 2012.
- Pulsed erbium YAG laser ablation in cutaneous surgery. Lasers Surg Med. 1996;19:324-30.
- [Google Scholar]
- Ultrapulse carbon dioxide laser ablation of xanthelasma paplebrarum: A case series. J Cutan Aesthet Surg. 2015;8:46-9.
- [Google Scholar]
- Is Q-switched neodymium-doped yttrium aluminium garnet laser an effective approach to treat xanthelasma palpebrarum? Results from a clinical study of 76 cases. Dermatol Surg. 2009;35:1962-9.
- [Google Scholar]
- Xanthelasma palpebrarum treatment with a 1450-nm-diode laser. Dermatol Surg. 2011;37:791-6.
- [Google Scholar]
- Treatment of xanthelasma palpebrarum using a pulsed dye laser: A prospective clinical trial in 38 cases. Dermatol Surg. 2010;36:610-7.
- [Google Scholar]






