Translate this page into:
Innovative Paradigm in Aesthetics Medicine: Proposal for Diagnostic Morphological Geometric by Thirds, Semiology in Clinical Applied to Aging Facial
Address for correspondence: Dr. Dubraska V. Suárez-Vega, Department of Research, University of the Andes (ULA), and 23rd Street between avenues 2 and 3, Mérida 5101, Venezuela. E-mail: dubraskasuarez.ula@gmail.com.
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The diagnosis of aging based on the morphogeometric changes experienced by the face, measured by the application of facial stratigraphic semiology by thirds, could become a novel approach that guarantees an efficient replacement of aged tissues through minimally invasive aesthetic medicine strategies. Facial aging should be analyzed by thirds, because not all thirds grow old at the same time. Owing to this is necessary go giving solve the aging problems each one of them, by means of therapies of the facial restructuring into sequential treatment appointments, with the purpose of being go giving time to the tissues rearrangement of the face, so that it is perceived as a subtle progressive reversal of aging and so generate a comfortable social acceptance of the resulting changes of said facial rejuvenation. This article intends to present the practical approach of the concepts and guidelines illustrated in the routine aesthetic diagnosis, the anatomical changes in the various tissue layers that are externally appreciated, but detailing them under a regional approach (upper, middle, and lower thirds). Our paradigm seeks that as professionals of aesthetic and regenerative medicine we identify facial aging not only as the obvious wrinkles and other changes in the skin, but that we diagnose according to the proposed parameters, so that when considering the rejuvenation treatment, we identify which are facial tissues that have changed due to aging and must therefore be restored to harmonize the face according to the ideal forms and proportions that must prevail (morphometry).
Keywords
Aesthetic facial diagnosis
facial aging
facial anthropometry
acial morphometry
facial thirds
INTRODUCTION
Aging is a biological process resulting from the gradual reduction in structural component and cell function. A young face has normal volume and well-defined contours. As we age, the regional facial aesthetic units separate more, mainly due to resorption into bone and fat tissues.[1]
Despite this, aging is still being diagnosed based only on skin findings, such as skin flaccidity, thinner skin and elastosis, and deeper folds and ridges, without considering that they often partly result from the deterioration of the ligaments that sustain soft tissues, such as the orbitomalar, zygomatic, and masseteric ligaments.[2]
The loss of bone support, along with the reduction in fat pad volume, accentuates skin folds. For example, it is more pronounced in areas such as the nasolabial fold, the labiomandibular fold (marionette line), and the nasojugal fold.[3]
As such, understanding facial aging by layers is essential for an accurate diagnosis and for deciding on the right treatment plan. It involves using a model that assumes that facial aging affects every layer and not only the obvious rhytids and elastosis in the skin. This process involves changes in subcutaneous fat redistribution that lead to soft-tissue deflation, ptosis, or descent due to a loss of volume in the superficial and deep panniculus adiposus underneath the dermis, and lipomatosis due to fat accumulation, making the skin more flaccid. These changes underlie the thinning of the superficial muscular aponeurotic system, the laxity of the main skin-retaining ligaments that have to counterbalance the changes in fat pad volume, and facial muscle hyperfunction to compensate for a loss of fixation and resorption into the facial skeleton, the first aging changes to occur.
However, facial aging should also be analyzed by thirds, given that not every third ages in the same way, with the aim of being able to provide a solution for each one, with a progressive response during subsequent treatment appointments. This allows facial tissue to reform and for the change to be accepted socially, given that progressive aging reversion is subtle, based on facial restructuring treatments.
This article aimed to encourage the practical incorporation of the presented concepts and guidelines, considering externally evident anatomical changes in the different tissue layers, but examining them by specific regions (upper, middle, and lower thirds). This approach aims to both detect obvious changes in the skin and use the proposed parameters to determine if they are moving away from ideal forms and proportions (morphometry).
Once those concepts are understood, this article proposes to establish facial aging analysis by thirds, by applying clinical symptomatology in the structural analysis of the associated changes, in order to propose more accurate treatment protocols that are directly proportional to the changes that need compensating.
STRUCTURAL ANALYSIS BY THIRDS AND APPLIED CLINICAL SYMPTOMATOLOGY
Diagnosing facial aging-derived changes is possible by analyzing the structure by thirds, which is based on studying the individual characteristics of the face by studying facial proportions.[4] The aforementioned study is essential for an aesthetic diagnosis of the face. This evaluation generally takes place prior to planning treatments of the cranium, vertebra, and face, for both aesthetic medicine and plastic surgery.
Guidelines for analyzing the face have been established as part of this anthropometric trend of studying “face proportions.” These consider fixed bone points, called anthropometric reference points, which are useful for establishing the reference planes for “facial geometric morphometric” diagnosis. Those points and planes are discussed later.
REFERENCE POINTS AND PLANES IN FACIAL GEOMETRIC MORPHOMETRIC DIAGNOSIS
Parameters that enable a pre- and post-operation understanding of any of the face’s components are essential for plastic and reconstructive surgery, prosthetic rehabilitation, and dentistry (orthopedics, orthodontics, and aesthetic mouth rehabilitation). This means that the treatments always ensure facial proportions remain consistent, a model that is synonymous with health and youthfulness, as well as beauty.
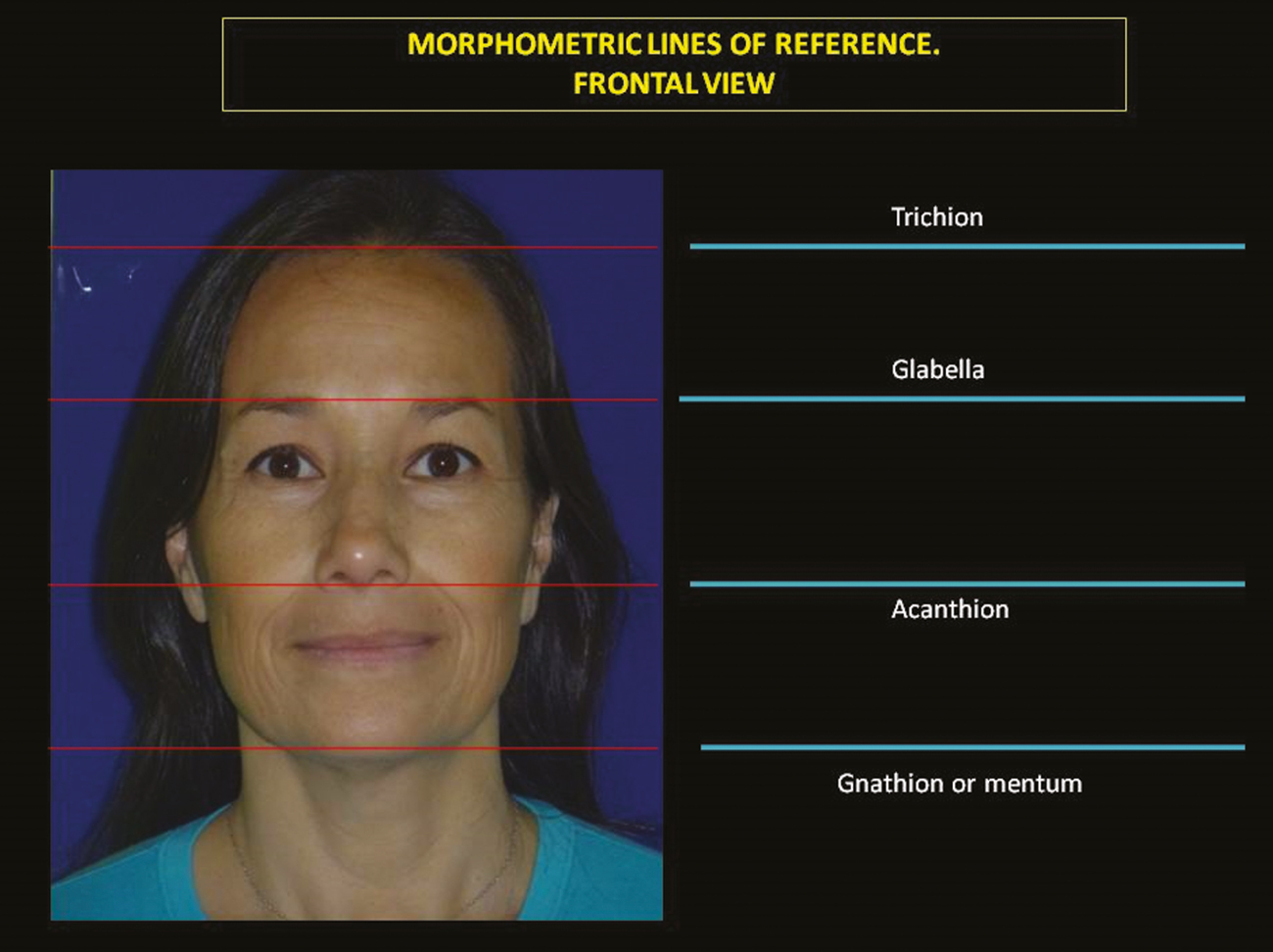
Analyzing the face requires using radiographic (lateral X-rays, computerized axial tomography, among others), photographic, and clinical studies, with subsequent cephalometric analysis based on universally accepted and standardized mathematical measurements and lines.[5] Some points and planes used as references for this facial analysis follow one of the resized neoclassical facial models based on the works of Farkas and Munro,[6] establishing cephalometric measurements that state that the total craniofacial height is divided into three equal parts or facial thirds, from the “trichion” to the “nasion”, from the nasion to the “acanthion”, and from the acanthion to the “gnathion.”[7]
Those four cephalometric points are located as follows: Trichion, the point where the hairline and the midsagittal plane intersect; glabella, the most prominent point of the forehead; nasion, the deepest depression where the forehead skin and the nasal root meet; acanthion, where the columella (base) ends and the upper lip skin portion starts; and menton or gnathion, the lowest part of the chin’s soft tissue.
To sum up, the height of face is divided into three equal parts. The first third or the “upper third” runs from the trichion to the glabella, the “middle third” from the glabella to the acanthion, and the “lower third” from the acanthion point to the inion or mental point, as shown in Figure 1.
- Craniometrical points and planes that are taken as a reference for facial geometric morphometric analysis
The aforementioned division is the basis of the proposal for analyzing facial aging by layers and thirds, and its derived clinical diagnoses.
THE UPPER THIRD
When referring to the upper third of the face, we mean practically the entire frontal bone that forms part of the facial skeleton or the face (approximately two-thirds of the frontal bone); that is, we exclude the part of the frontal bone under the scalp. Bone shape and muscle activity are closely linked with aesthetics. The width should be double its height.[8]
Aging of the frontal region clinically corresponds to a loss of frontal bone convexity. This leads to concavity developing above the eyebrow.[9] Muscle balance in the area is responsible for moving eyebrows.
These areas descend vertically, meaning central “frontal fat ptosis” leads to forehead ptosis, with descent vectors appearing that make the eyelid droop. The supraorbital and infraorbital areas, the peribuccal area, and even the mandibular contour become heavier.[10]
In addition, any fat in the area atrophies to a large extent, the fat volume that separated and masked the muscles in the area while youthful. On being lost, procerus and corrugator muscle activity in the frontal area is more evident, leaving permanent skin rhytids as a result.[11]
“Temporal region aging” is characterized by a gradual raising of superficial vascular topography and visible depressions, giving a clinical sign of a loss of volume. Movement vectors due to muscle atrophy, particularly the temporal muscle, also make the supraorbital and infraorbital areas, the peribuccal area, and even the mandibular contour[10] heavier. In both a frontal and side analysis, the most visible consequence of those changes is evidenced by the appearance of blepharochalasis of the upper eyelid, that is, the permanent descent of the upper eyelid [Figure 2].
![The side analysis of temporal region aging. Note that the temporal bone volume loss generates blepharochalasis of the upper eyelid. Adapted from Farkaset al.[12]](/content/173/2020/13/2/img/JCAS-13-112-g002.png)
- The side analysis of temporal region aging. Note that the temporal bone volume loss generates blepharochalasis of the upper eyelid. Adapted from Farkaset al.[12]
However, temporal bone volume loss can also be classified based on the depth of the area as follows:
Grade I: When the depression is at the supraorbital level
Grade II: When the depression is at the outer canthus level
Grade III: Temporal depression and pseudo-lifting of the zygomatic arch, either on one side or both sides[13]
Resulting from this descent and collapse in the upper third, changes occurring only in the upper area of the face end up in determining deflation in the middle and lower areas of the face.
STRUCTURAL ANALYSIS AND SYMPTOMATOLOGY APPLIED TO UPPER THIRD AGING
When determining the symptomatology of aging in the upper third, the clinical aspects of the upper area need to be taken into account, with the following recommendations:
Evaluate expression lines or rhytids during muscle rest.
Evaluate the trichion or the intersection between the midsagittal plane and the hairline, for studying the density of the scalp in both central and temporal areas.
Measure the height and breadth of the forehead (the distance between the mid-pupillary line and the anterior hairline, or the distance between the center of the eyebrow and the anterior hairline).
Measure the volumetry of the forehead compared to the opposite side by always considering the temporal depth or its loss of volume.
Measure the eyebrow position. There are several ways of doing this. The eyebrow can be measured in relation to the superior orbital rim or measured from the end of the supraorbital rim to the eyebrow, and from the medial canthus and the lateral canthus toward the medial eyebrow and in a lateral direction.[14]
Evaluate static and dynamic expressions of the glabellar complex (folds or rhytids associated with the movement of the corrugators or superciliaries and the pyramidal-shaped procerus muscle), classifying them as one of the four main patterns of glabellar complex contraction: U, V, Ω (omega), and Ʊ (inverted omega). This is in order to suitably distribute the doses of chemical denervation treatment using neuromodulators.[15]
MIDDLE THIRD AGING
The main changes occur in the bone tissue, with a resorption process producing the following:
The deepening of the maxilla superior in its virtual anatomical space
The opening of the pyriform space
The descent of the nasojugal fold
The flattening of the nasal slope, with axial orbital opening [Figure 3]
![Changes by Middle Third Aging. Posterior displacement of the alar base. Deepening of the maxilla results in posterior positioning of the nasolabial crease and adjacent upper lip. Adapted from Mendelson and Wong[16]](/content/173/2020/13/2/img/JCAS-13-112-g003.png)
- Changes by Middle Third Aging. Posterior displacement of the alar base. Deepening of the maxilla results in posterior positioning of the nasolabial crease and adjacent upper lip. Adapted from Mendelson and Wong[16]
The anthropometric bone point called “pyriform”, located in the pyriform fossa of the maxilla superior bone, is in a more forward position than the anterior lacrimal crest (A) in this third during youth [Figure 4].
![Midface Aging. Reduction of the piriform angle and maxillary angle with aging. This angles recedes with aging, from youth (left) to old age (right). Adapted from Shaw Jr. and Kahn[17]](/content/173/2020/13/2/img/JCAS-13-112-g004.png)
- Midface Aging. Reduction of the piriform angle and maxillary angle with aging. This angles recedes with aging, from youth (left) to old age (right). Adapted from Shaw Jr. and Kahn[17]
With aging, the pyriform craniometric point located in front of the anterior lacrimal crest regresses as a result of selective bone resorption of the maxilla. The maxilla is more susceptible to age-related loss than the zygomatic bone. As a result, the pyriform angle, the glabellar angle, and the maxillary angle significantly regress with aging, from youth to old age.[1718]
It occurs due to atrophy of the maxilla superior bone (hypoplasia), which loses height, with the orbital cavity widening. The deep midfacial fat pads (suborbicular fat and deep medial fat) move to form any folds, particularly the nasojugal fold. This fold is a depression caused by the separation of the orbicular muscle from the eyelids and the levator labii superioris muscle, with anteroposterior regression of the globe of the eye. Externally on the skin, it constitutes the “area of transition” between the eyelid, nose, and cheek, forming a deepened triangular surface with an external base and medially located upper corner. The nasojugal fold anatomically occurs due to ptosis projection caused by medial and internal fat in the lower limit of the palpebral orbicularis muscle without supporting fat tissue throughout the fold.[19]
Bone loss in the pyriform area weakens the support of the lateral nasal cartilage. The deepening of the maxilla results in retropositioning (posterior) of the nasolabial fold and the upper lip. The weakness of the ligaments (sustaining tissues) along with the enlargement of the pyriform space creates the opening for the nasal alas in the soft tissues and a lowering of the nose tip, which end up reducing the nasolabial angle.[16]
Bone loss in the pyriform area weakens the lateral support. The deepening of the maxilla leads to deflation of the malar fat panniculus with posterior positioning of the nasolabial fold and the adjacent upper lip [Figure 5].[20]
![Deepening profile of the midface by aging. The angle of facial convexity decrease. The distance between facial plane ( line from glabella to gnathion) and maxilla increase leading to deflation of the malar fat panniculus with formation of the nasolabial fold and posterior positioning of the upper lip. Adapted from Cotofana et al.[20]](/content/173/2020/13/2/img/JCAS-13-112-g005.png)
- Deepening profile of the midface by aging. The angle of facial convexity decrease. The distance between facial plane ( line from glabella to gnathion) and maxilla increase leading to deflation of the malar fat panniculus with formation of the nasolabial fold and posterior positioning of the upper lip. Adapted from Cotofana et al.[20]
When it comes to the nasolabial fold, the factors in its formation include the significant involvement of some muscles, as well as bone resorption, atrophy, and the descent of superficial and deep fat panniculus in the region.
The shared levator muscle of the upper lip and nasal ala inserts into the medial nasolabial fold and the ala base, whereas the upper lip levator inserts into the middle third of the nasolabial fold and is involved in the formation of the nasolabial fold. This is because a separate muscle was identified at an oblique angle between the orbicularis oculi and the shared levator muscle of the upper lip and the nasal ala, inserting into the malar fat pad. This muscle is the “malar levator,” which was present in all cadaver specimens that were studied, and it is involved in medial periorbital wrinkles forming the nasojugal fold and the deepening of the nasolabial fold [Figure 6].[21]
![Muscles implied in the nasolabial and nasojugal fold formation. The cadaveric fresh dissection shows the location of the malaris muscle (ML) with its insertion into the malar fat pad (MFP), a recent finding with clinical implications in the formation of the nasojugal fold. Adapted from Snider et al.[21]](/content/173/2020/13/2/img/JCAS-13-112-g006.png)
- Muscles implied in the nasolabial and nasojugal fold formation. The cadaveric fresh dissection shows the location of the malaris muscle (ML) with its insertion into the malar fat pad (MFP), a recent finding with clinical implications in the formation of the nasojugal fold. Adapted from Snider et al.[21]
A classification of the volumetric aging of the middle third arose out of the movement of fat from the middle third and the formation of the resulting folds.
STRUCTURAL ANALYSIS AND SYMPTOMATOLOGY APPLIED TO MIDDLE THIRD AGING
The middle third is to be understood as the entire medial area of the face that runs vertically from the glabellar plane (an imaginary line extending horizontally from both sides of the glabella bone anthropometric point) to the acanthion plane (an imaginary line running horizontally from the anterior nasal bone anthropometric point). As such, evaluating that zone will require dividing the middle third into the following:
Upper middle third (UMT): From the Frankfort plane to the glabellar
Lower middle third (LMT): From the Frankfort plane to the acanthion plane
Two planes are found in the UMT:
-
(1)
The bipupillary plane subplane (BPPa): It divides the UMT into two parts with the upper and lower eyelids present.
-
(2)
The bipalpebral subplane (BPPb): Superior, joining two points located on the most visible folds of the upper eyelid.
This division is particularly useful for evaluating blepharoptosis, eyelid ptosis, or “eyelid blepharochalasis or dermatochalasis,” one of the most significant consequences of aging in the upper third and UMT, with symptoms such as permanent lower or eyelid droop observed, which can involve one side or both sides.
Therefore, one of the objectives of facial aging symptomatology of the UMT will involve measuring the grade of true dermatochalasis or blepharochalasis compared to dermatochalasis caused by forehead ptosis, establishing the presence of superior dermatochalasis or superior blepharochalasis (DCHS) and/or lower blepharochalasis or inferior dermatochalasis (DCHI). To that end, it is essential to evaluate the position of the lateral, central, and medial; retro-orbicularis oculi fat (ROOF); and suborbicularis oculi fat pat (SOOF) fat pads, and any lacrimal gland prolapse.
Classification of superior blepharochalasis
Superior blepharochalasis or superior palpebral ptosis” is the descent or droop of the upper eyelid. This is divided into: Mild: when the descent hardly forms a fold (nonsurgical)
Moderate: when it runs under the bipalpebral plane (surgical or nonsurgical blepharoplasty with a sublimation protocol)
Severe: when it runs more than 1 mm under the bipalpebral plane, a descent that restricts upper vision (surgical)
Classification of inferior blepharochalasis
“Inferior blepharochalasis or inferior palpebral ptosis” is the descent of the lower eyelid, causing in some cases, ectropion due to the increased weight of the eyelid.
Mild: when only some periorbicular depressions occur
Moderate: when the tissue is descending without going below the Frankfort plane
Severe: when the descent goes below the Frankfort plane
This zone also requires evaluation of any periorbital rhytids or lines that are present.
In the LMT, it is mainly possible to evaluate the following:
-
(1)
The position of the nose
-
(2)
A loss of cheek projection due to a higher nasolabial angle
-
(3)
The presence of pigmentations
-
(4)
Malar descent
-
(5)
Joint opening and closing observation
-
(6)
The ear’s location
-
(7)
Hyperactivity of the nasal slope muscles
-
(8)
The nasojugal fold
Adhering to the nasofacial angle guidelines is recommended for evaluating the nose’s position, which establishes that the approximate angle of the nose’s position is within 30° and 40°, a measurement that enables the prediction of the elevation of the nose tip. Its reduction undoubtedly implies aging in the LMT.
Classification of the type of aging of the middle third
Type 1 or hypotrophic (aging caused by hypotrophy): In type 1, there is extensive volume reduction in all maxilla fat tissues, mainly in the deep pads (of the eye’s lateral suborbicular fat and the cheek’s deep medial fat). The entire region looks flat or concave. The nasolabial fold is caused by pseudoptosis of the skin that is not compatible with the underlying soft tissues and is redundant. The cheek is concave because of hypotrophy in the mid part of the cheek fat.[22]
Type 2 hypotrophic/ptotic (aging caused mainly by hypotrophy, but with a secondary ptotic component): Hypotrophy mainly occurs in the deep fat pads (of the medial and lateral suborbicular fat and the cheek’s deep medial fat). The entire area looks concave in the suborbital section while the section close to the nasolabial fold is slightly convex due to ptosis of the nasolabial pad. The nasolabial fold is again determined by pseudoptosis of the skin, appearing more prominent due to ptosis of the nasolabial fat. The cheek is slightly convex due to ptosis of the cheek’s medial fat.
Type 3 ptotic/hypertrophic (aging mainly caused by ptosis, but with a secondary hypertrophic component): Damaged maxilla fat tissue moves downwards due to ptosis of superficial fat pads. The infraorbital region appears flat or slightly concave due to hypotrophy of the eye’s medial suborbicular fat and ptosis of the cheek’s medial fat, while the nasolabial region is convex due to hypertrophy of the nasolabial fat pad. Nasolabial folds are caused by ptotic descent and hypertrophic nasolabial fat. The cheek is convex due to ptosis and hypertrophy of the cheek’s medial fat. The sunken posterior part of the cheek starts to become apparent due to hypertrophy of the cheek’s lateral fat.
Type 4 hypertrophic/ptotic (aging mainly caused by hypertrophy, but with a secondary ptotic component): Maxilla fat tissue is hypertrophic and moves downwards due to ptosis of the superficial fat pads. The region appears concave only in the nasojugal fold although the central part and the nasolabial region are clearly convex. Nasolabial folds are caused by the descent of superficial fat pads and accentuated by hypertrophy. Hypertrophy and ptosis of the cheek’s medial fat make the cheek convex, notably defined by the cheek’s lateral fat hypertrophy.[22]
As such, middle third volume recovery treatments target compensating zones where superficial and deep fat panniculus have experienced hypotrophy and ptosis (suborbicular lateral and medial fat, and the cheek’s deep medial fat).
However, an aged middle third appearance does not only derive from bone resorption, but rather middle third mimic muscle dynamics, which are involved in these clinical symptoms of aging. For example, involvement of the malaris muscle has even been associated with the deepening of the nasojugal and nasolabial fold present at rest below the lower eyelid area fold present below the lower eyelid area.
THE LOWER THIRD
Facial skeleton remodeling occurs constantly, both when teeth are present and when they are missing, although losing teeth significantly accelerates maxilla and mandibular bone resorption. So the mandibular angle increases, while the height of the ramus, the height and length of the mandibular body decrease.
Lower third aging is characterized by active bone resorption. All these resorptive changes of the inferior maxilla appear as follows:
In the maxilla superior
The menton area
A reduction in mandibular height
A change in position of the external oblique line
Lip reversion
Subsequent fold formation and accentuation, such as the nasolabial and labiomental fold
A loss of facial contouring
Deflation of the mouth floor
As these bone changes start to occur, the soft tissue starts to detach due to a reduced area and loss of support from the facial ligaments, that is, the deflation of the submental area. The line of the mandible laterally defines the lower border of the face. As the fat pads that cover it descend and the mandibular septum loosens, “jowling” develops as a sign of aging. Submental ptosis and the movement of submalar fat are significant characteristics in the loss of facial contouring in the lower third due to aging [Figure 7].[2]
![Changes involved in the fat pads in the loss of facial contouring in the lower third due to aging. (A) Computerized tomography (CT) of the lower third, which shows the skin’s surface (upper panel) and the anterior part of the mandible with the labiomandibular (LM) fat pads, and the left inferior menton fat (Jowl, lower panel). The yellow arrows indicate the position of the LM fold. The white arrow indicates the position of the mandibular retaining ligament. (B) CT of the menton, which shows the submental fat. This pad is not adjacent to the mentolabial fold. Adapted from Gierloff et al.[23]](/content/173/2020/13/2/img/JCAS-13-112-g007.png)
- Changes involved in the fat pads in the loss of facial contouring in the lower third due to aging. (A) Computerized tomography (CT) of the lower third, which shows the skin’s surface (upper panel) and the anterior part of the mandible with the labiomandibular (LM) fat pads, and the left inferior menton fat (Jowl, lower panel). The yellow arrows indicate the position of the LM fold. The white arrow indicates the position of the mandibular retaining ligament. (B) CT of the menton, which shows the submental fat. This pad is not adjacent to the mentolabial fold. Adapted from Gierloff et al.[23]
Although these bone changes are responsible for several of the external signs of aging, such as the deepening of the nasolabial fold, many studies and techniques approach eliminating the nasolabial fold under the belief that the predominant cause is the loss of volume and the descent of soft tissue. However, the nasolabial fold’s etiology also derives from prolonged muscle activity.
Understanding the impact of the mimic muscles involved simply requires observing the appearance of the face’s lower third in patients with facial nerve paralysis, who lose almost the entire nasolabial fold on the side denerved by the paralysis, providing solid evidence for understanding the clinical implication of muscle activity in accentuating the nasolabial fold. This phenomenon mainly involves middle third facial muscles (with activity of the levator of the upper lip and nasal ala), the transverse nasal muscle, the upper lip levator, and an emerging muscle between the eyelid orbicular and the levator of the upper lip and the nasal ala, responsible for rotating the medial fat or malar fat panniculus of the face during its action, the malaris, or malar levator.[21]
The loss of facial bone volume largely contributes to age-related facial changes. The skin starts to fold as a result, and elasticity is lost because there is smaller biologic response, making the facial expression dark, with the folds deriving in secondary complications, and generating conditions such as:
-
(1)
angular cheilitis
-
(2)
lacrimal infections
-
(3)
vertical deflation
-
(4)
negative vectors
-
(5)
ectropion
-
(6)
keratosis
-
(7)
joint pain
-
(8)
fat pad descent
-
(9)
pseudoptosis, and
-
(10)
myofascial pain.
This is the moment when aging changes from physiological to pathological, meaning that restoring tissues not only achieves an aesthetic/cosmetic objective for facial beauty and rejuvenation, but also has a true corrective treatment purpose.
STRUCTURAL ANALYSIS AND SYMPTOMATOLOGY APPLIED TO LOWER THIRD AGING
This area extends from the acanthion plane to the submental plane. Here we have to detect the pathognomonic clinical signs of aging. Evaluating the following is recommended:
-
(1)
The presence and length of the nasolabial depression
-
(2)
The presence and length of the mentolabial depression
-
(3)
The vertical size
-
(4)
Masseter dystonia
-
(5)
A study of the lips or clinical cheilometry
-
(6)
The mental region: the width and projection, the mentolabial fold, the labiomandibular fold (the marionette line), and mental hypercontraction
-
(7)
The submalar region: positioning and volume
-
(8)
A loss of mandible line contouring and the grade of mentocervical deflation
Aesthetic vertical dimension
When evaluating lower third aging, a pragmatically useful parameter is the determination of the aesthetic vertical dimension (AVD). This is a facial measurement that enables the predictive calculation of the initial position of facial structures and their grade of deflation.
This is a fixed reference, which enables reconsideration of the original youthful facial proportions, recalling lip volume, the profile shape or the smile line, and natural folds, along with the shape and unique size of teeth. It varies by patient, and even the same patient will provide diagnostic parameters for the grades of aging of the lower third that are also directly proportional to the aging of the facial complex.
AVD is based on measuring the vertical dimension during occlusion. This is the space between the maxilla of an individual in the frontal plane, defined as the measurement of the anterior facial height, taken between two randomly selected, conventionally located points, coinciding with the midline, one in the upper maxilla (acanthion) and another on the mandible (menton). In accordance with the above, the AVD is the distance between those two craniometric points projected on the soft tissue.
Determining the grade of aging of the lower third will come from comparing this height between the maxilla with the measurement of the facial area that does not experience changes due to bone resorption. This is the zygomatic area up to the zone where the temporomandibular joint is located. These two measurements should be proportional and if they differ because of a shorter distance between the maxilla, this undoubtedly derives from a reduction in the vertical dimension and, therefore, the aging of the face’s lower third.
This technique is known as “Knebelman’s method” in which an adjustable caliper was used to establish that “the measurement of the distance from the eye’s outer canthus to the ear’s tragus is proportionately related to the measurement of the nose-menton distance.” In addition, the measurement of the distance between the lower mandible surface and the nose bone is proportional to the distance measured from the outer canthus to the labial commissure.
On the basis of the level of discrepancy between these measurements, it is possible to classify the grade of aging as mild, moderate, and severe:
Mild: a difference of 2–5 mm between both measurements
Moderate: a difference of 7–10 mm between both measurements
Severe: over 10 mm difference between both distances
Clinical cheilometry
Lip study and analysis form part of the facial examination in both dentistry (orthodontics, prosthodontics, and dental aesthetics) and aesthetic medicine. Applying filler to lip structures without prior clinical analysis can cause major functional and aesthetic inconveniences to patients that undergo the procedure.
Cheilometry is defined as the study of lip structures, specifying how the lip region with all that surface covered by skin and a mucous membrane, forms the oral sphincter,[24] considering the lips as part of the mouth cavity. The lips also have a fat pad and muscle support, which during youth gives them their volumetric appearance, reducing with aging [Figure 8].
![Reduction of the deep submuscular lips fat and the aging appearance of perioral zone. Vertical sectioning of the lower lip shows deep submuscular fat. Of particular note, this specimen’s lower lip showed anterior projection and eversion similar to that seen in a much younger individual. The clinical impression from this research is that the volume of deep lip fat contributes significantly to the appearance of the youthful lip. Adapted from Rohrich et al.[25]](/content/173/2020/13/2/img/JCAS-13-112-g008.png)
- Reduction of the deep submuscular lips fat and the aging appearance of perioral zone. Vertical sectioning of the lower lip shows deep submuscular fat. Of particular note, this specimen’s lower lip showed anterior projection and eversion similar to that seen in a much younger individual. The clinical impression from this research is that the volume of deep lip fat contributes significantly to the appearance of the youthful lip. Adapted from Rohrich et al.[25]
As part of aging symptomatology in the perioral region, evaluations should examine the presence of rhytids; the lip length of the skin portion of the lips, particularly if the upper lip is stretched by elastosis; a loss of fat volume; and a loss of bone support. The flattening of the labial philtrum is to be evaluated, which reduces the projection of Cupid’s bow.
The region of the semi-mucous portion of the lips or the labial vermillion border should be evaluated for the shape, position of the commissures, the proportion and the contour, the length of the opening, the lip position, or the upper and lower lip-face profile with respect to Ricketts’ aesthetic plane (the distance of the lips with respect to a plane made by a line drawn from the nose tip to the most prominent point of the menton). Also required evaluation is the upper and lower lip length of the vermilion border to the Klein line, and througth a cheilogram its must be measured the length of each segment of the lip vermilion border, in order to detect discrepancies, lip incompetence, and lip asymmetries that could be correcteds [Figure 9].
![Cheilogram points and zones. The cheilogram, a diagnostic tool in applied clinical cheilometry with possible correction zones using dermal fillers. Adapted from Maqueda et al.[26]](/content/173/2020/13/2/img/JCAS-13-112-g009.png)
- Cheilogram points and zones. The cheilogram, a diagnostic tool in applied clinical cheilometry with possible correction zones using dermal fillers. Adapted from Maqueda et al.[26]
THE MENTOCERVICAL DEFLATION SCALE
The oldest etymological origin of “deflation” comes from Latin, made up of three parts of that language: the prefix “des,” which is used to indicate separation or descent; the verb “flare,” which is synonymous for “swell”; and the suffix “tion,” which is indicative of “action.” It is the action of detachment. It has been etymologically associated with the descent of facial structures caused by aging or aggressive and rapid fat loss.[27]
Establishing the grade of lower third aging also needs to consider the position of the tissues in the mandibular contour. As these tend to experience laxity, a scale has been proposed to measure the level of descent objectively. The aforementioned mentocervical deflation scale uses the drawing of a tangent to the mandibular edge as a reference, drawn in the patient’s photograph facing both to the front and to the side, in which the head’s position enables the location of parallelism between the Frankfort plane and the horizon or floor.
It sets out three levels of deflation. The scale runs from 0 to 4 for the level of sagging; the neck volume grades can vary from 0 (no sagging or deflation) to 4 (very severe sagging). However, this a subjective classification based on comparing a visual scale with some standardized photos by the authors, meaning that it was necessary to modify it to set objective measurements, using the mentocervical angle as a reference and its gradual opening in the more severe cases of mentocervical deflation. The mentocervical angle is a parameter that is normally between 80° and 95°; that is, higher angles would indicate the severity of the deflation [Figure 10].
![Mentocervical deflation scale. With the agin the mentocervical angle its gradual opening. Higher angles would indicate the severity of the deflation or severe sagging. Adapted from Sattler et al.[28]](/content/173/2020/13/2/img/JCAS-13-112-g010.png)
- Mentocervical deflation scale. With the agin the mentocervical angle its gradual opening. Higher angles would indicate the severity of the deflation or severe sagging. Adapted from Sattler et al.[28]
Grade 0 would be equivalent to the 80° and 95° guideline and indicate no deflation.
Grade 1, or mild deflation, would be equivalent to measurements ranging between approximately 105° and 130°, still considered as within an acceptable variation from the guideline.
Grade 2 or moderate deflation is between 140° and 170°.
Grade 3 or severe deflation is at an angle 180°.
Grade 4 or very severe mentocervical deflation is between approximately 190° and 230°.
CONCLUSION
Facial aging should be analyzed by thirds, given that not all thirds age the same, with the aim of being able to resolve each one and with a progressive response for any that subsequently follow. New understanding of the facial aging process in the structural planes of facial anatomy (mainly the fat pads, the retaining ligaments, the muscle vectors, and the bone tissue conditions) is relevant to effectively dispose regenerative medicine treatments in facial aesthetics.
As such, clarifying the diagnostic parameters for age-related structural and morphofunctional changes can lead to the correct treatments based on:
the grades or types of aging based on the three major facial zones in a vertical direction;
the level of skin aging and derived pathologies requiring a solution using redensifying, skin remodeling, indirect cell biostimulation using photonic medicine or electromedicine, and direct cell biostimulation using intradermal therapy, or using other latest generation transdermal release systems;
facial kinetics, mimic, and masticatory, for determining the muscle lifting vectors (e.g., frontal) or descent vectors (e.g., the platysma muscles) that should be tackled with neuromodulators in order to restore facial balance;
establishing the most suitable orofacial support protocol in accordance with the grade of tissue displacement (e.g., considering the most suitable dosing and vectorization of the dermal fillers for infiltration); and
the skin support strategy to use in accordance with the grade of deflation and diagnosed lipomatosis (e.g., re-absorbable threads to support the skin and physicochemical remodeling of the face’s fat pads).
However, it is always worth remembering that one algorithm cannot effectively manage facial aging for all, as despite facial anatomy research revealing epidemiologically consistent structures across most individuals, the anomalies and variations of anatomical structures make each individual unique, and as a result, the diagnosis and treatment of aging vary and should be adapted to individual needs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Three-dimensional approach of cosmetic patient: aging gracefully. In: Issa M, Tamura B, eds. Botulinum toxins, fillers and related substances. Cham, Switzerland: Springer; 2018. p. :1-22. Clinical approaches and procedures in cosmetic dermatology doi:10.1007/978-3-319-20253-2_40-1
- [Google Scholar]
- Approach to the mature cosmetic patient: aging gracefully. J Drugs Dermatol. 2017;16:s84-6.
- [Google Scholar]
- Software Antropmeter, una nueva herramienta para análisis facial. 2008. Int J Morphol. 26:973-4. doi:10.4067/S0717-95022008000400031. Available from: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0717-95022008000400031&lng=es
- [Google Scholar]
- Advances in facial contouring and implants. Facial Plastic Surg Clin North Am. 1999;7:1-15.
- [Google Scholar]
- Anthropometric facial proportions in medicine. Springfield, IL: Charles. C. Thomas; 1987. doi:10.1016/0889-5406(87)90240-X.
- 2018. Master techniques in facial rejuvenation. London: Elsevier; doi:10.1016/B978-0-323-35876-7.00029-7. Available from: http://www.sciencedirect.com/science/article/pii/B9780323358767000297
- Cirugía de Cabeza, del cuello y maxilofacial. Lima, Perú: MAD Corp SA; 2002.
- High-resolution magnetic resonance imaging of aging upper face fat compartments. Plast Reconstr Surg. 2017;139:829-37. 10.1097/PRS.0000000000003860.
- [Google Scholar]
- Anthropometric measurements of the facial framework in adulthood: age-related changes in eight age categories in 600 healthy white north Americans of European ancestry from 16 to 90 years of age. J Craniofac Surg. 2004;15:288-98.
- [Google Scholar]
- The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J. 2006;26:S4-9. doi:10.1016/j.asj.2005.09.012.
- [Google Scholar]
- Clinical validation of the surface volume coefficient for minimally invasive treatment of the temple. J Drugs Dermatol. 2019;18:533-40.
- [Google Scholar]
- Mid forehead brow lift. 2019. StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK535452/
- [Google Scholar]
- Glabellar contraction patterns: a tool to optimize botulinum toxin treatment. Dermatol Surg. 2012;38:1506-15. doi:10.1111/j.1524-4725.2012.02505.x.
- [Google Scholar]
- Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36:753-60. doi 10.1007/s00266-012-9904-3.
- [Google Scholar]
- Proximal alveolar bone loss in a longitudinal radiographic investigation. Swed Dent J Suppl. 1986;35:1-108.
- [Google Scholar]
- Aging of the midface bony elements: a three-dimensional computed tomographic study. Plast Reconstr Surg. 2007;119:675-81. doi 10.1097/01.prs.0000246596.79795.a8.
- [Google Scholar]
- Patterns of change in facial skeletal aging. JAMA Facial Plast Surg. 2017;19:413-7. doi 10.1001/jamafacial.2017.0743
- [Google Scholar]
- The science and theory behind facial aging. Plast Reconstr Surg Glob Open. 2013;1:e8-15. doi 10.1097/GOX.0b013e31828ed1da.
- [Google Scholar]
- Midface: clinical anatomy and regional approaches with injectable fillers. Plast Reconstr Surg. 2015;136:219-34S. doi 10.1097/PRS.0000000000001837
- [Google Scholar]
- New insights into the anatomy of the midface musculature and its implications on the nasolabial fold. Aesthetic Plast Surg. 2017;41:1083-90. doi 10.1007/s00266-017-0889-9.
- [Google Scholar]
- The midface treatment with fillers the bolus technique (2nd ed – Spanish edition). Florence, Italy: OEO Chapter 6, The invisible lifting; 2017. p. :109-57.
- The subcutaneous fat compartments in relation to aesthetically important facial folds and rhytides. J Plast Reconstr Aesthet Surg. 2012;65:1292-7. doi 10.1016/j.bjps.2012.04.047.
- [Google Scholar]
- Reconstrucción labial: principios y técnicas. Cuadernos de Cirugía. 2018;18:98-105. doi 10.4206/cuad.cir.2004.v18n1-16
- [Google Scholar]
- The anatomy of suborbicularis fat: implications for periorbital rejuvenation. Plast Reconstr Surg. 2009;124:946-51. doi 10.1097/PRS.0b013e3181b17b76
- [Google Scholar]
- Queilometría clínica aplicada a rellenos labiales con ácido hialurónico. Acta bioclínica. 2012;2:26-34.
- [Google Scholar]
- Deflación facial vs lipomatosis mitos y realidades. 2017. Acta Bioclin. 7:1-4. Available from: http://erevistas.saber.ula.ve/index.php/actabioclinica/article/view/8347/8292
- [Google Scholar]
- Validated assessment scale for neck volume. Dermatol Surg. 2012;38:343-50. doi 10.1111/j.1524-4725.2011.02253.x.
- [Google Scholar]






