Translate this page into:
Scar orientation: Principles in plastic surgery
Address for correspondence: Mr. Kavit R. Amin, Department of Plastic Surgery, Royal Preston Hospital, Sharoe Green Lane, PR2 9HT Preston, UK. E-mail: kavamin@yahoo.co.uk
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
For biopsy proven skin cancers that are deemed to be high risk, a wide local excision (WLE) is recommended to reduce the risk of local recurrence. For this reason, it is pragmatic to account for the likelihood of a WLE at the time of the initial biopsy. We illustrate a staged approach to excision of lesions to facilitate this, bearing in mind the optimal reconstruction is primary closure. In our experience as plastic surgeons, having to perform a locoregional flap or skin graft prevents the opportunity to perform a local anesthetic procedure. This increases the risk of postoperative complications, especially if adjuvant radiotherapy further exposes reconstructed tissues to radiation toxicity. Collectively, this often results in an inferior aesthetic outcome. We value the referrals from allied colleagues and want to share the principles we adhere to when planning an excision biopsy, which aid in the delivery of the optimal reconstruction.
Keywords
Healing
scar
scar orientation
skin cancer
For biopsy proven skin cancers that are deemed to be high risk, a wide local excision (WLE) is recommended to reduce the risk of local recurrence. This includes (not limited to) basal cell carcinoma, squamous cell carcinoma, soft-tissue sarcoma, and malignant melanoma. Up to 20% of malignant melanomas are biopsied in primary care.[1] There is a strong case for dermatologists to take the lead in diagnosing these lesions.[2] In accordance with updated guidelines from the National Institute for Clinical Excellence (NICE), a confirmed diagnosis of melanoma requires a WLE around the biopsy scar of between 1 and 2cm dependent on the Breslow thickness of the primary lesion.[3]
It is pragmatic to account for the likelihood of a WLE at the time of the initial biopsy, bearing in mind the optimal reconstruction is primary closure. In our experience as plastic surgeons, having to perform a locoregional flap or skin graft prevents the opportunity to perform a local anesthetic procedure. This increases the risk of postoperative complications, especially if adjuvant radiotherapy further exposes reconstructed tissues to radiation toxicity.[4] Collectively, this often results in an inferior aesthetic outcome. We find that this is most evident on the neck, back, and distal lower limb where tissue laxity is limited.
A longitudinally orientated scar is preferred on the limbs, in order to take advantage of the circumferential laxity often found in extremities and the parallel alignment to the direction of lymphatic drainage [Figure 1]. This has beneficial effects in minimizing edema.[5]
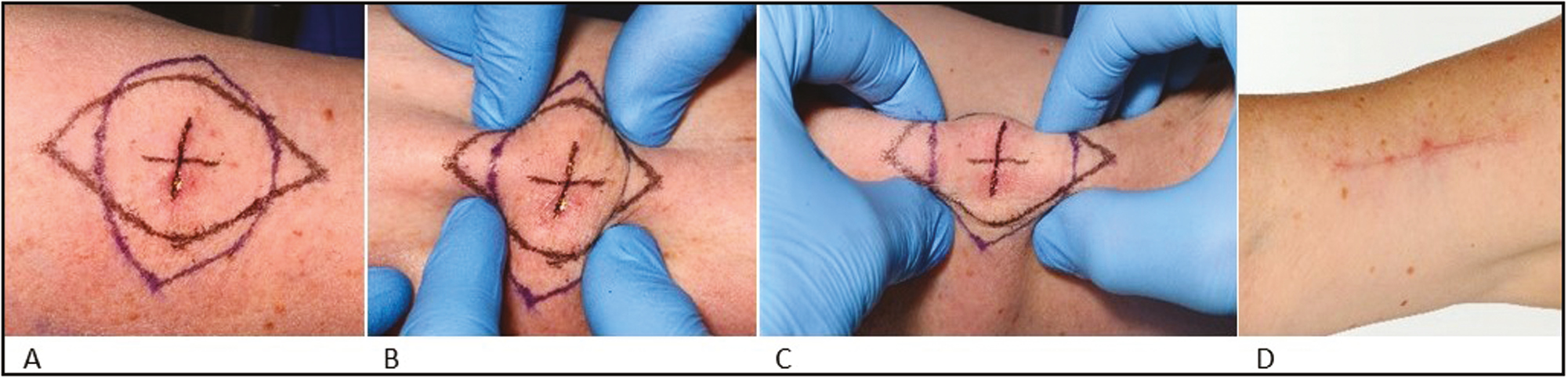
- (A) scar on the arm of patient denoted by +. (B) Transverse orientation of WLE scar and limited skin laxity. (C) Longitudinal orientation and maximal recruitment of circumferential laxity. (D) Healed, longitudinally orientated WLE scar
Thirdly, biopsies that incorporate an ellipse lengthen the scar. We find that a non-epileptiform, entirely marginal excision of the lesion first, enables a more controlled assessment of wound closure. For small defects, a useful exercise is to pinch and approximate the wound edges gauging the direction the laxity is arising from, aiding in the decision of scar orientation. For larger wounds, the same exercise can be repeated with skin hooks or Kilner “catspaw” retractors. Following closure, the wound can then be extended in order to excise any resulting standing cone/“dog-ear’’ deformity.
We value our referrals from colleagues in Primary Care and Dermatology. We wanted to share the principles we adhere to when planning an excision biopsy, which aid in the delivery of the optimal reconstruction.
LEARNING POINTS
Primary wound closure is the optimal reconstructive option
Longitudinal orientation of the scar in limbs recruits circumferential laxity and runs parallel to lymphatics to minimize edema.
Marginal excision followed by approximation of wound edges with the’ pinch test’ reduces surplus skin excision and identifies optimal scar orientation.
Following closure of the marginal defect, the wound can be extended to eliminate any resulting standing cone/“dog ear” deformity and closed
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- Primary excision of cutaneous melanoma: Does the location of excision matter. Br J Gen Pract. 2011;61:131-4.
- [Google Scholar]
- Dermatological surgery: a comparison of activity and outcomes in primary and secondary care. Br J Dermatol. 2009;161:110-4.
- [Google Scholar]
- 2015. Melanoma: assessment and management. Available from: https://www.nice.org.uk/guidance/ng14/resources/melanoma-assessment-and-management-pdf-1837271430853.
- Wound healing after radiation therapy: review of the literature. Radiat Oncol. 2012;7:162.
- [Google Scholar]






