Translate this page into:
A Novel Technique to Improve Accuracy of Mohs Mapping for Large Stages with a Small Tumor Burden
Address for correspondence: Dr. Atieh Jibbe, 3901 Rainbow Boulevard, MS 2025, Kansas City, Kansas 66160, USA. E-mail: ajibbe@kumc.edu
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Precision of the Mohs micrographic surgery (MMS) process during orientation, microscopic analysis, tissue mapping, and tumor clearance of specimen margins is essential for MMS to attain high cure rates; however, this elaborate process is subject to error. Large tumor stages with a small tumor burden present an avenue for error during MMS mapping. We present a novel technique to improve the accuracy of MMS mapping using an MMS slide marked for residual tumor superimposed onto a mobile device photograph of the surgical defect. This is taken to better identify location of residual tumor both on the digitalized MMS photomap and surgical defect. This novel technique decreases recurrence rates by decreasing the inevitable subjectivity involved with the superimposition of residual tumor foci from a microscopic view onto the digitalized MMS photomap then onto the surgical defect particularly in larger stages with a small tumor burden.
Keywords
Digital
mapping
micrographic surgery
Mohs
technology
INTRODUCTION
Mohs micrographic surgery (MMS) relies on the ability of a surgeon to identify residual tumor on a histologic frozen section, then extrapolate the tumor location onto a specimen map. The surgeon uses the map to identify positive margins in the surgical defect so that a further stage can be excised. Techniques to improve MMS mapping such as tissue orientation procedures and imaging versus hand-drawn maps have been documented in the literature. We present a novel technique using an MMS slide marked for residual tumor superimposed onto a mobile device photograph of the surgical defect taken to better identify the location of residual tumor both on the digitalized MMS photomap and surgical defect. Our technique aims to improve the accuracy in mapping of residual tumor onto a digitalized MMS photomap and subsequently increase the accuracy of extrapolation of the map onto the surgical defect. This technique is most useful for large tumor stages with minimal epidermal landmarks and small tumor foci where it can be difficult to delineate where residual tumor lies.
TECHNIQUE
As the surgeon excises the first stage, attention is taken to properly score the tissue specimen and defect to preserve orientation of the tissue relative to the wound. Orientation techniques may include the use of tissue nicks, gentian violet, suture, staples, or methylene blue; for our case, tissue nicks and gentian violet were used.[1] After marking the tissue stage, a mobile device photograph is taken of the surgical defect using a 12 megapixel or greater digital camera on a smartphone or tablet. For accurate replication of the defect, the smartphone or tablet should be held parallel to the skin. Distance from the skin should be manipulated until the most proximate, focused photograph is attainable without touching the surgical field. When taking an image of the surgical defect, the surgeon must visualize on the mobile device screen the entirety of the surgical defect with a border of surrounding skin, and at the same time ensure clarity of the image by focusing the image before taking the photo. This photograph is then uploaded into the electronic medical record (EMR) system for digital photomapping.
The next step involves the microscopic analysis of the frozen sections of the MMS specimen for residual tumor. Once residual tumor has been identified, the surgeon, during microscopic examination, uses a fine-tipped white Sharpie marker to mark the location of the residual tumor on the slide [Figure 1]. The marked slide is then held in front of the mobile device photograph. The photograph is manually adjusted on the phone/tablet screen by the surgeon to best match the size and orientation of the slide specimen. The orientation of the image can later be adjusted to match the orientation of the MMS map using the rotation feature on the smartphone. This allows direct visualization of the residual tumor location on the photograph [Figure 2]. The tumor location is then marked on the digitalized MMS photomap in the EMR [Figure 3]. This technique may be repeated until all specimen margins are microscopically free of tumor.
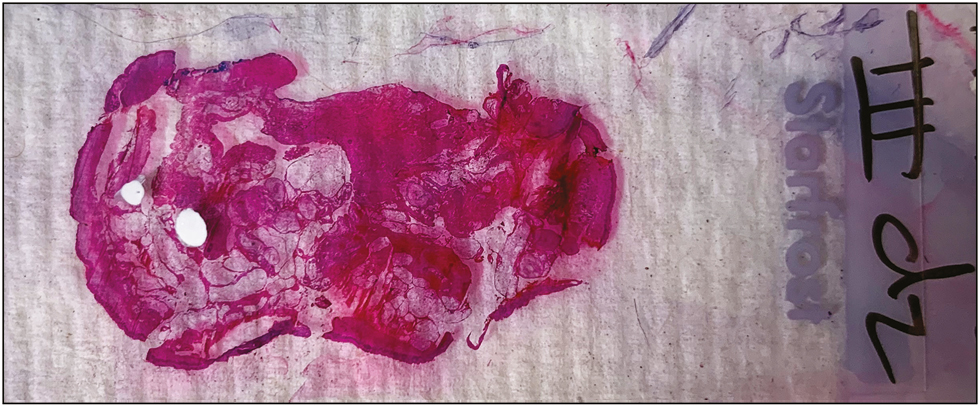
- Frozen section slide marked for residual tumor using fine-tipped white Sharpie marker
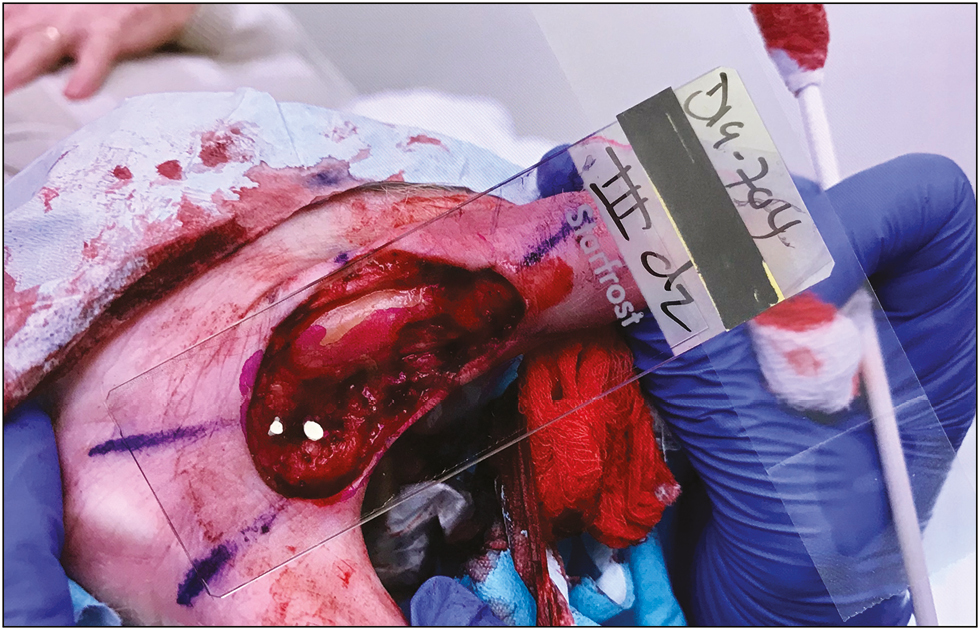
- Marked slide placed in front of mobile device photograph of surgical defect
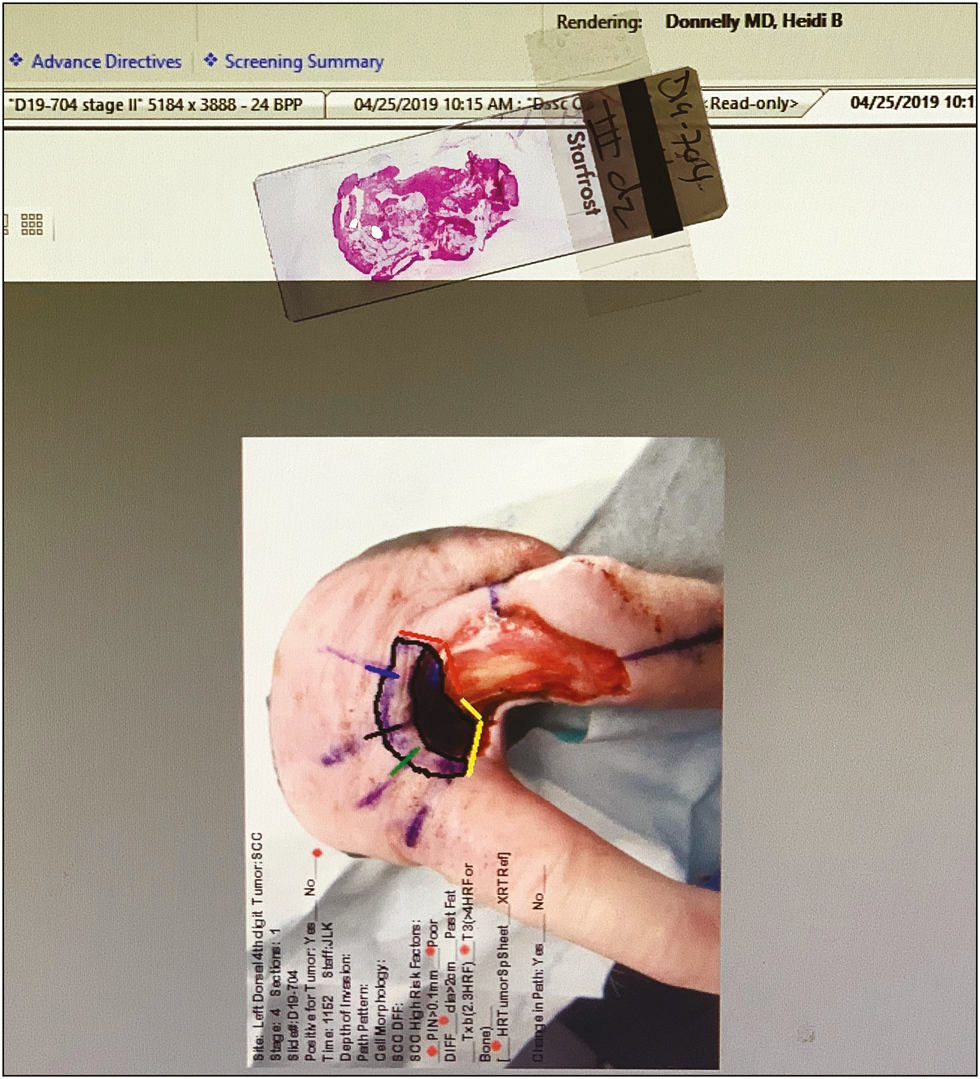
- Digitalized MMS photomap in EMR marked for residual tumor
DISCUSSION
Precision in the MMS process during orientation, microscopic analysis, tissue mapping, and tumor clearance of specimen margins is essential for MMS to attain high cure rates. However, each step in this elaborate process is subject to error. Techniques to reduce this error have been proposed, intending to improve tissue marking, transfer, flattening, processing, and mapping.[1] The use of digital photography for MMS mapping to reduce error in MMS process has been well-documented in the literature. In 1997, Ratner et al.[2] introduced the uses of digital photography in dermatology including imaging of MMS surgical defects. In 2000, Alcalay[3] described the use of digital computerized MMS mapping based on image processing in a computer. Since then, the use of digital photography in MMS, although frequently used for pre-op and post-op imaging of the defect and repair, has been used for MMS mapping by a minority of surgeons. In a 2019 study surveying Mohs tracking practices, only 1.6% of Mohs surgeons used digital photography for tissue mapping.[4] The advantages of digital photography for tissue mapping include depicting the precise size, shape, and orientation of the tumor and wound in addition to the patient anatomy at each stage, ease of use, and improved documentation capability, making photography an excellent option for tissue mapping, especially for large defects with minimal epidermal landmarks and small tumor foci.[15]
Our technique incorporates the use of photography of the scored tissue defect, a corresponding digitalized MMS photomap, and a slide marked for residual tumor. The superimposition of the marked slide onto the mobile device photograph delineates the exact location of the residual tumor, which is then transferred to the digitalized MMS photomap, thus improving the accuracy of mapping. Given that the digitalized MMS photomap is a visual of the surgical defect, this technique will also improve the accuracy of the projection of the map onto the surgical defect.
The advantages of this technique include ease of use, improved documentation of the location of the layer taken, and improved precision of MMS mapping and extrapolation of the digitalized MMS photomap onto the surgical defect. Serial photographs also make it easier to interpret the inevitably changing anatomy when multiple stages are taken.[5] In our case, the third-stage surgical defect of a large squamous cell carcinoma contained periosteum and soft tissue. Superimposition of the marked slide onto the mobile device photograph identified residual tumor in the soft tissue rather than over the adjacent bone allowing us to excise a further stage without concern for bony involvement.
A disadvantage of this technique is that it requires additional time to take the photograph of the marked stage, upload the photo into the EMR for mapping, indicate positive areas on the slide with a white Sharpie marker, and superimpose the slide over a mobile device photograph. The additional time required is around 3–5 min. Another disadvantage is resource dependence given that the surgeon needs to have access to an EMR system that can accommodate digitalized MMS photomaps and capability to use a smartphone or tablet. However, this is becoming less relevant in modern society given that the use and dependability of smartphones and tablets is gradually increasing with time. A final disadvantage to this technique is the risk of surgical contamination with the non-sterile smartphone or tablet. However, we recommend surgeons proceed with caution with the non-sterile smartphone hovering far enough from the surgical site to avoid any contact with surgical field.
Finally, in the last decade, the use of reflectance confocal microscopy (RCM) has been applied at the patient’s bedside for lateral margin detection in basal cell carcinoma and lentigo maligna, because of its capability of exploring the skin histologically, enabling the identification of tumor characteristics.[6] We believe that our technique is a cheap and efficient way to better assess location of positive tumor on the frozen section relative to the surgical defect, once a positive tumor margin is already diagnosed via microscopy that functions independently of RCM. These techniques both supplement the MMS process at a different stage: RCM at the level of diagnosis of positive tumor margins within the defect, and our technique, superimposing the already identified positive tumor margin onto the surgical defect.
In conclusion, this novel technique would theoretically decrease recurrence rates by decreasing the inevitable subjectivity involved with the superimposition of residual tumor foci from a microscopic view onto the digitalized MMS photomap then onto the surgical defect particularly in larger stages with a small tumor burden.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Mohs mapping fidelity: optimizing orientation, accuracy, and tissue identification in Mohs surgery. Dermatol Surg. 2018;44:1-9.
- [Google Scholar]
- The uses of digital photography in dermatology. J Am Acad Dermatol. 1997;41:749-56.
- [Google Scholar]
- Digital computerized mapping in Mohs micrographic surgery. Dermatol Surg. 2000;26:692-3.
- [Google Scholar]
- Use of digital photographic maps for Mohs micrographic surgery. Dermatol Surg. 2014;40:349-51.
- [Google Scholar]
- In vivo and ex vivo confocal microscopy for dermatologic and Mohs surgeons. Dermatol Clin. 2016;34:497-504.
- [Google Scholar]






